Sunday Poster Session
Category: Liver
P1875 - Progressive Familial Intrahepatic Cholestasis Type 3: A Rare Cause of Chronic Liver Disease in a Young Female
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Uday Kumar Repalle, MBBS (he/him/his)
Dr. Pinnamaneni Siddhartha Institute of Medical Sciences and Research Foundation
Chinoutpalli, Andhra Pradesh, India
Presenting Author(s)
Asha Jyothika Kalagadda, MD1, Dinesh Gupta Satyavarapu, MD2, Uday Kumar Repalle, MBBS3, Sarayu Devabhaktuni, MBBS4, Hanisha Reddy Kukunoor, MBBS5, Vijetha Reddy Katta, MBBS6
1Guntur Medical College, Guntur, Andhra Pradesh, India; 2Guntur medical College, Guntur, Andhra Pradesh, India; 3Dr. Pinnamaneni Siddhartha Institute of Medical Sciences and Research Foundation, Chinoutpalli, Andhra Pradesh, India; 4Dr. Pinnamaneni Siddhartha Institute of Medical Sciences and Research Foundation, Vijayawada, Andhra Pradesh, India; 5Maheshwara medical college and hospital, Patancheruvu, Telangana, India; 6Sri Padmavathi Medical College for Women, San Francisco, CA
Introduction: Progressive familial intrahepatic cholestasis (PFIC), refers to a group of inherited autosomal recessive disorders that cause rapidly progressive intrahepatic cholestasis. PFIC is classified into three types: PFIC1, PFIC2, PFIC3. PFIC3 is the rarest, with an incidence of 1 in 5,00,000 births, it is caused by mutations in the ATP binding cassette subfamily B member 4 gene (ABCB 4) located on chromosome 7, that encodes multidrug resistance class III (MDR3) protein crucial for bile secretion.
Case Description/
Methods: A 15year-old female patient, presented with complaints of insidious onset and gradually progressing pedal edema, abdominal distension, facial puffiness. She reported history of similar complaints 4 months prior. Clinical examination revealed moderate splenomegaly. Ultrasonography demonstrated coarsely echo textured liver with surface irregularities and moderate splenomegaly measuring 11cm. Laboratory investigations demonstrated Hb 8.9 g/dl, Platelet count of 1,70,000/ μL, Serum bilurubin 2.9 mg/dL, SGOT 202U/L, SGPT 96 U/L, ALP 310 U/L, GGT 107 U/L, SAAG of 1.5. T3:0.63ng/ml, TSH:7.49mlU/L. 24hour urinary copper:62mg/day, Serum Ceruloplasmin:25mg/dl, MRI brain shows symmetrical T1hyperintesities in bilateral basal ganglia. UGI endoscopy shows G-2 Esophageal varices. Liver biopsy shows altered architecture with mild rosetting, mild lobular inflammation. Portal tracts show infiltration by lymphoplasmacytic cells and polymorphs. Portal fibrosis present, copper staining seen. Genetic analysis revealed mutation of ABCB4 on chr7
Discussion: PFIC 3 is a rare autosomal recessive disease defined by mutations in the ABCB4 gene, which encodes the MDR3 protein. Dysfunction of MDR3 due to ABCB4 mutations cause impaired PtdCho secretion, leading to the accumulation of unneutralized bile salts, causing bile salt-induced injury to the biliary epithelium and bile canaliculi thus acquiring cholestasis, advanced liver disease and cirrhosis.
Clinically PFIC 3 manifests within 1st year of life with symptoms of cholestasis that may progress to cirrhosis and end-stage liver damage over time. Older children typically have symptoms of portal hypertension such as splenomegaly and hematemesis. Given its rarity and overlapping clinical features with other hepatobiliary diseases, diagnosis is heavily reliant on genetic testing thereby causing significant delays. Its low prevalence and variable presentation, poses PFIC3 as a diagnostic challenge, underscoring the importance of understanding this medical rarity.
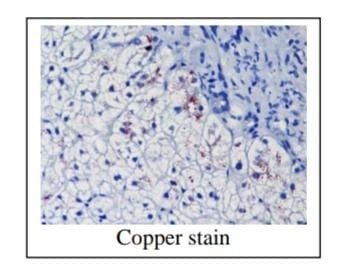
Figure: HE LIVER
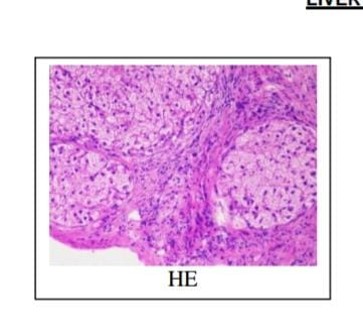
Figure: COPPER STAIN LIVER
Disclosures:
Asha Jyothika Kalagadda indicated no relevant financial relationships.
Dinesh Gupta Satyavarapu indicated no relevant financial relationships.
Uday Kumar Repalle indicated no relevant financial relationships.
Sarayu Devabhaktuni indicated no relevant financial relationships.
Hanisha Reddy Kukunoor indicated no relevant financial relationships.
Vijetha Reddy Katta indicated no relevant financial relationships.
Asha Jyothika Kalagadda, MD1, Dinesh Gupta Satyavarapu, MD2, Uday Kumar Repalle, MBBS3, Sarayu Devabhaktuni, MBBS4, Hanisha Reddy Kukunoor, MBBS5, Vijetha Reddy Katta, MBBS6. P1875 - Progressive Familial Intrahepatic Cholestasis Type 3: A Rare Cause of Chronic Liver Disease in a Young Female, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Guntur Medical College, Guntur, Andhra Pradesh, India; 2Guntur medical College, Guntur, Andhra Pradesh, India; 3Dr. Pinnamaneni Siddhartha Institute of Medical Sciences and Research Foundation, Chinoutpalli, Andhra Pradesh, India; 4Dr. Pinnamaneni Siddhartha Institute of Medical Sciences and Research Foundation, Vijayawada, Andhra Pradesh, India; 5Maheshwara medical college and hospital, Patancheruvu, Telangana, India; 6Sri Padmavathi Medical College for Women, San Francisco, CA
Introduction: Progressive familial intrahepatic cholestasis (PFIC), refers to a group of inherited autosomal recessive disorders that cause rapidly progressive intrahepatic cholestasis. PFIC is classified into three types: PFIC1, PFIC2, PFIC3. PFIC3 is the rarest, with an incidence of 1 in 5,00,000 births, it is caused by mutations in the ATP binding cassette subfamily B member 4 gene (ABCB 4) located on chromosome 7, that encodes multidrug resistance class III (MDR3) protein crucial for bile secretion.
Case Description/
Methods: A 15year-old female patient, presented with complaints of insidious onset and gradually progressing pedal edema, abdominal distension, facial puffiness. She reported history of similar complaints 4 months prior. Clinical examination revealed moderate splenomegaly. Ultrasonography demonstrated coarsely echo textured liver with surface irregularities and moderate splenomegaly measuring 11cm. Laboratory investigations demonstrated Hb 8.9 g/dl, Platelet count of 1,70,000/ μL, Serum bilurubin 2.9 mg/dL, SGOT 202U/L, SGPT 96 U/L, ALP 310 U/L, GGT 107 U/L, SAAG of 1.5. T3:0.63ng/ml, TSH:7.49mlU/L. 24hour urinary copper:62mg/day, Serum Ceruloplasmin:25mg/dl, MRI brain shows symmetrical T1hyperintesities in bilateral basal ganglia. UGI endoscopy shows G-2 Esophageal varices. Liver biopsy shows altered architecture with mild rosetting, mild lobular inflammation. Portal tracts show infiltration by lymphoplasmacytic cells and polymorphs. Portal fibrosis present, copper staining seen. Genetic analysis revealed mutation of ABCB4 on chr7
Discussion: PFIC 3 is a rare autosomal recessive disease defined by mutations in the ABCB4 gene, which encodes the MDR3 protein. Dysfunction of MDR3 due to ABCB4 mutations cause impaired PtdCho secretion, leading to the accumulation of unneutralized bile salts, causing bile salt-induced injury to the biliary epithelium and bile canaliculi thus acquiring cholestasis, advanced liver disease and cirrhosis.
Clinically PFIC 3 manifests within 1st year of life with symptoms of cholestasis that may progress to cirrhosis and end-stage liver damage over time. Older children typically have symptoms of portal hypertension such as splenomegaly and hematemesis. Given its rarity and overlapping clinical features with other hepatobiliary diseases, diagnosis is heavily reliant on genetic testing thereby causing significant delays. Its low prevalence and variable presentation, poses PFIC3 as a diagnostic challenge, underscoring the importance of understanding this medical rarity.
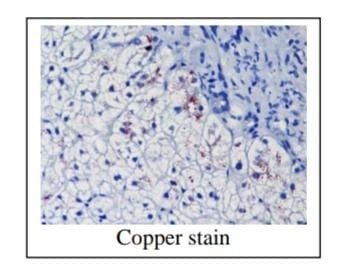
Figure: HE LIVER
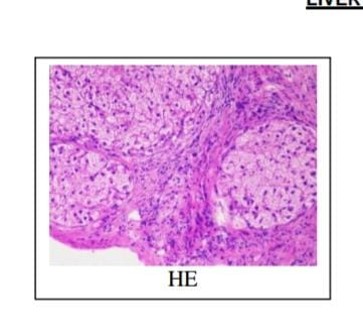
Figure: COPPER STAIN LIVER
Disclosures:
Asha Jyothika Kalagadda indicated no relevant financial relationships.
Dinesh Gupta Satyavarapu indicated no relevant financial relationships.
Uday Kumar Repalle indicated no relevant financial relationships.
Sarayu Devabhaktuni indicated no relevant financial relationships.
Hanisha Reddy Kukunoor indicated no relevant financial relationships.
Vijetha Reddy Katta indicated no relevant financial relationships.
Asha Jyothika Kalagadda, MD1, Dinesh Gupta Satyavarapu, MD2, Uday Kumar Repalle, MBBS3, Sarayu Devabhaktuni, MBBS4, Hanisha Reddy Kukunoor, MBBS5, Vijetha Reddy Katta, MBBS6. P1875 - Progressive Familial Intrahepatic Cholestasis Type 3: A Rare Cause of Chronic Liver Disease in a Young Female, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
