Sunday Poster Session
Category: Liver
P1833 - Zieve’s Syndrome: A Rare Cause of Hemolytic Anemia in Chronic Alcohol Use – A Case Report
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Muhamad Oum, MD (he/him/his)
Saint Agnes Medical Center, Fresno CA
Fresno, CA
Presenting Author(s)
Award: ACG Presidential Poster Award
Muhamad Oum, MD1, Celise Nardes Ferreira, MD2, Mahwish Sheikh, MD1, Hamna Javed, MD3, Shahab Dian, MD, MBA4
1Saint Agnes Medical Center, Fresno CA, Fresno, CA; 2Saint Agnes Medical Center, Fresno, CA; 3Saint Agnes Medical Center, Fresno, CA, Fresno, CA; 4Saint Agnes Medical Center, Clovis, CA
Introduction: Zieve’s syndrome is an uncommon but clinically important triad of jaundice, hemolytic anemia, and hyperlipidemia that occurs in the setting of chronic alcohol use and underlying liver disease. Due to its episodic nature and clinical similarity to other hepatic conditions, it is often misdiagnosed or overlooked. Prompt identification is critical to avoid unnecessary testing and guide appropriate management focused on alcohol cessation and supportive care.
Case Description/
Methods: A 38-year-old female with a history of daily alcohol intake presented with chest pain and melena. Physical examination showed scleral icterus and right upper quadrant tenderness. Initial labs revealed hemoglobin 7 g/dL, total bilirubin 2.0 mg/dL (direct 0.8 mg/dL), and ALP 157 IU/L. CT abdomen showed nodular cirrhosis. EGD revealed grade 1 esophageal varices. She was transfused and discharged.
Four months later, she returned with nausea, abdominal pain, tremors, and pruritus. Repeat labs demonstrated hemoglobin 7.1 g/dL, total bilirubin 6.5 mg/dL (direct 1.9), AST 88 U/L, ALT 37 U/L, and a markedly elevated reticulocyte index (21%). Hemoglobinuria and low haptoglobin (< 30 mg/dL) were present. Direct Coombs test was negative. Peripheral smear showed macrocytosis, anisopoikilocytosis, and polychromasia. Imaging revealed hepatosplenomegaly. The constellation of hemolytic anemia, jaundice, chronic alcohol use, and laboratory findings confirmed Zieve’s syndrome.
Discussion: Although first described in 1957, Zieve’s syndrome remains under-recognized, with fewer than 200 reported cases. Its pathophysiology involves alcohol-induced hepatocellular damage, erythrocyte membrane instability, and altered lipid metabolism. Diagnosis is primarily clinical and relies on identifying hemolysis in the context of alcohol use and liver disease. Hyperlipidemia, while classic, may be transient or absent at presentation, complicating diagnosis. This patient exhibited the core features of the syndrome during two separate admissions, underscoring the risk of recurrence and the importance of ongoing abstinence. Recognition of this reversible condition can prevent unnecessary interventions and enable prompt supportive care.
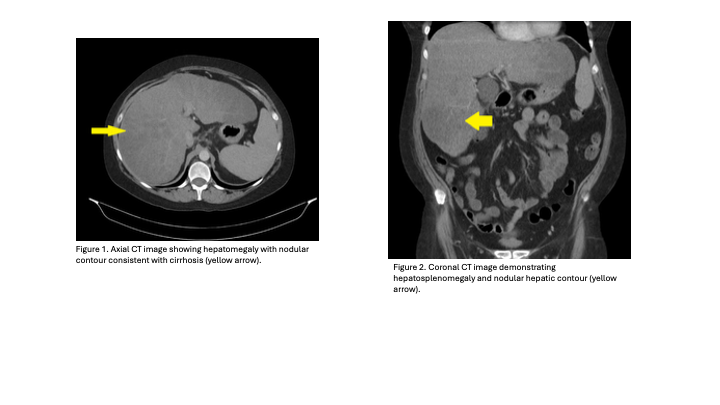
Figure: Figure 1. Axial CT image showing hepatomegaly with nodular contour consistent with cirrhosis (yellow arrow).
Figure 2. Coronal CT image demonstrating hepatosplenomegaly and nodular hepatic contour (yellow arrow).
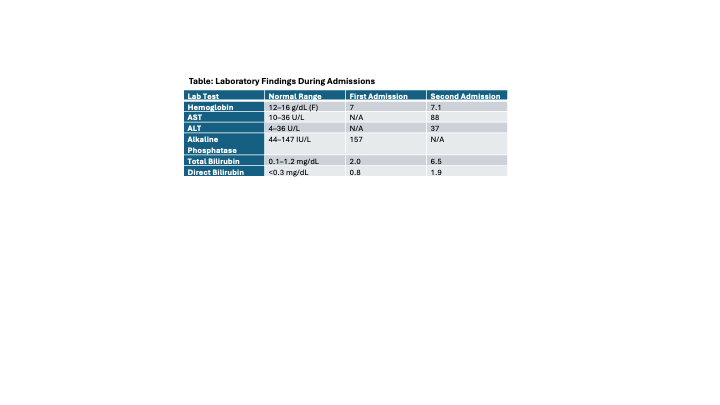
Figure: Table: Laboratory Findings During Admissions
Disclosures:
Muhamad Oum indicated no relevant financial relationships.
Celise Nardes Ferreira indicated no relevant financial relationships.
Mahwish Sheikh indicated no relevant financial relationships.
Hamna Javed indicated no relevant financial relationships.
Shahab Dian indicated no relevant financial relationships.
Muhamad Oum, MD1, Celise Nardes Ferreira, MD2, Mahwish Sheikh, MD1, Hamna Javed, MD3, Shahab Dian, MD, MBA4. P1833 - Zieve’s Syndrome: A Rare Cause of Hemolytic Anemia in Chronic Alcohol Use – A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Muhamad Oum, MD1, Celise Nardes Ferreira, MD2, Mahwish Sheikh, MD1, Hamna Javed, MD3, Shahab Dian, MD, MBA4
1Saint Agnes Medical Center, Fresno CA, Fresno, CA; 2Saint Agnes Medical Center, Fresno, CA; 3Saint Agnes Medical Center, Fresno, CA, Fresno, CA; 4Saint Agnes Medical Center, Clovis, CA
Introduction: Zieve’s syndrome is an uncommon but clinically important triad of jaundice, hemolytic anemia, and hyperlipidemia that occurs in the setting of chronic alcohol use and underlying liver disease. Due to its episodic nature and clinical similarity to other hepatic conditions, it is often misdiagnosed or overlooked. Prompt identification is critical to avoid unnecessary testing and guide appropriate management focused on alcohol cessation and supportive care.
Case Description/
Methods: A 38-year-old female with a history of daily alcohol intake presented with chest pain and melena. Physical examination showed scleral icterus and right upper quadrant tenderness. Initial labs revealed hemoglobin 7 g/dL, total bilirubin 2.0 mg/dL (direct 0.8 mg/dL), and ALP 157 IU/L. CT abdomen showed nodular cirrhosis. EGD revealed grade 1 esophageal varices. She was transfused and discharged.
Four months later, she returned with nausea, abdominal pain, tremors, and pruritus. Repeat labs demonstrated hemoglobin 7.1 g/dL, total bilirubin 6.5 mg/dL (direct 1.9), AST 88 U/L, ALT 37 U/L, and a markedly elevated reticulocyte index (21%). Hemoglobinuria and low haptoglobin (< 30 mg/dL) were present. Direct Coombs test was negative. Peripheral smear showed macrocytosis, anisopoikilocytosis, and polychromasia. Imaging revealed hepatosplenomegaly. The constellation of hemolytic anemia, jaundice, chronic alcohol use, and laboratory findings confirmed Zieve’s syndrome.
Discussion: Although first described in 1957, Zieve’s syndrome remains under-recognized, with fewer than 200 reported cases. Its pathophysiology involves alcohol-induced hepatocellular damage, erythrocyte membrane instability, and altered lipid metabolism. Diagnosis is primarily clinical and relies on identifying hemolysis in the context of alcohol use and liver disease. Hyperlipidemia, while classic, may be transient or absent at presentation, complicating diagnosis. This patient exhibited the core features of the syndrome during two separate admissions, underscoring the risk of recurrence and the importance of ongoing abstinence. Recognition of this reversible condition can prevent unnecessary interventions and enable prompt supportive care.
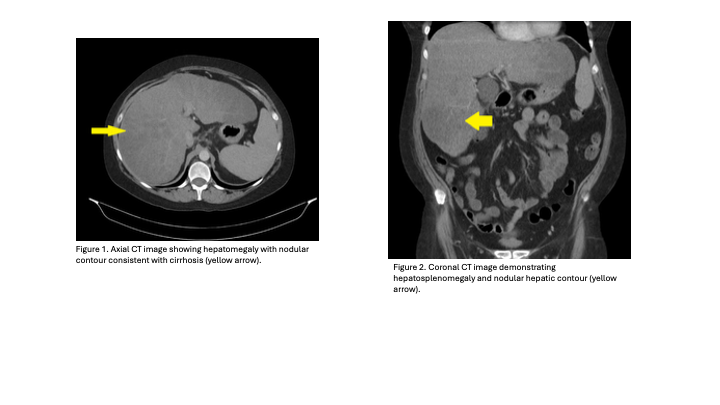
Figure: Figure 1. Axial CT image showing hepatomegaly with nodular contour consistent with cirrhosis (yellow arrow).
Figure 2. Coronal CT image demonstrating hepatosplenomegaly and nodular hepatic contour (yellow arrow).
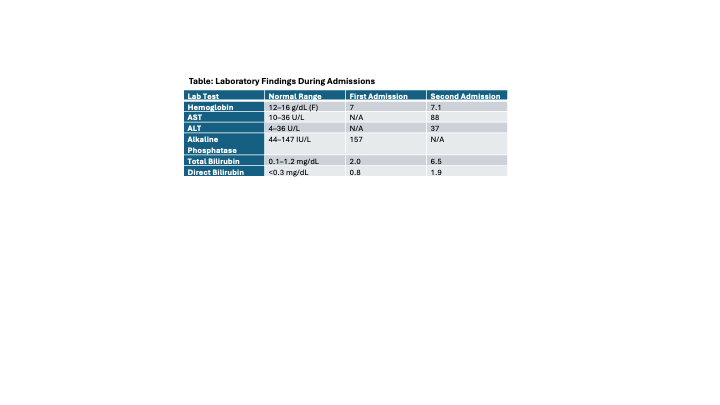
Figure: Table: Laboratory Findings During Admissions
Disclosures:
Muhamad Oum indicated no relevant financial relationships.
Celise Nardes Ferreira indicated no relevant financial relationships.
Mahwish Sheikh indicated no relevant financial relationships.
Hamna Javed indicated no relevant financial relationships.
Shahab Dian indicated no relevant financial relationships.
Muhamad Oum, MD1, Celise Nardes Ferreira, MD2, Mahwish Sheikh, MD1, Hamna Javed, MD3, Shahab Dian, MD, MBA4. P1833 - Zieve’s Syndrome: A Rare Cause of Hemolytic Anemia in Chronic Alcohol Use – A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

