Sunday Poster Session
Category: Liver
P1824 - The Liver That Broke the Belly: Abdominal Compartment Syndrome From Isolated Hepatomegaly
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- SA
Sultan Ahmed, DO
Mercyhealth Internal Medicine Residency
Rockford, IL
Presenting Author(s)
Award: ACG Presidential Poster Award
Sultan Ahmed, DO1, Nada Saleh, MD2, Abu Fahad Abbasi, MD3, Ammar Aqeel, MD4, Ediri Brume, MD2, Thayer Hamoudah, MD5
1Mercyhealth Internal Medicine Residency, Rockford, IL; 2Mercy Health, Rockford, IL; 3Mercyhealth Gastroenterology Fellowship, Rockford, IL; 4Mercyhealth, Rockford, IL; 5Mercyhealth Gastroenterology, Rockford, IL
Introduction: Abdominal Compartment Syndrome (ACS) is defined as pressure in the abdomen > 20 mmHg, with signs of end-organ damage. Typically, this occurs due to increased intraabdominal pressure (IAP). Common culprits include massive fluid resuscitation, polytransfusion, hypothermia, coagulopathy, sepsis, and hepatic dysfunction with ascites. We present a rare case of isolated hepatomegaly resulting in devastating ACS.
Case Description/
Methods: A 26-year-old male with a history of alcohol use disorder presented with intractable, nontraumatic epistaxis and was found to have abnormal labs with AST 473 U/L, ALT 33 U/L, total bilirubin 3.3 mg/dL, ALP 372 U/L, INR 1.4, alcohol level 0.42 gm/dL, and lactic acid of 7.8 mmol/L. Exam revealed profound abdominal distension without a fluid wave. Imaging demonstrated severe hepatomegaly and steatosis with right-sided colonic thickening. Assessment of bladder pressure ranged from 15–25 mmHg, consistent with intra-abdominal hypertension and evolving ACS. The patient developed worsening lactic acidosis, hypotension requiring vasopressors, respiratory failure necessitating intubation, and renal failure requiring dialysis. Emergent decompressive laparotomy and right hemicolectomy were performed. Despite intervention, IAP remained elevated. Repeat laparotomy revealed patchy necrosis of the distal ileum and colon, prompting end ileostomy and further resection. The patient’s condition continued to deteriorate, and care was transitioned to comfort measures.
Discussion: Excessive fluid resuscitation is the most common cause of ACS. Hepatomegaly with ascites is also known to increase IAP; however, isolated hepatomegaly as the primary cause of ACS is extremely rare and has not been previously implicated. In this case, massive hepatomegaly acted as a space-occupying lesion, compressing abdominal organs, reducing abdominal wall compliance, and impairing venous return. These changes led to bowel edema, progressive elevation of IAP, and multiorgan dysfunction, including reduced cardiac output, impaired intestinal perfusion, hypoxemia, and renal failure. Although decompressive laparotomy typically lowers IAP, mortality remains high, and recovery of organ function is often unpredictable. Despite prompt and repeated decompression, the patient’s pressure remained elevated and organ failure worsened, highlighting the aggressive and refractory nature of ACS secondary to massive hepatomegaly. Early recognition and intervention are critical to improving outcomes.
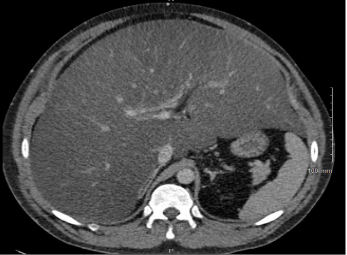
Figure: Figure 1: Demonstration of severe hepatomegaly with concomitant steatosis.

Figure: Figure 2: Re-demonstrated hepatomegaly with measurements: anterior-posterior diameter of the right hepatic lobe is 28 cm, the transverse diameter of the liver is 29 cm, and the cephalo-caudal length 33 cm.
Disclosures:
Sultan Ahmed indicated no relevant financial relationships.
Nada Saleh indicated no relevant financial relationships.
Abu Fahad Abbasi indicated no relevant financial relationships.
Ammar Aqeel indicated no relevant financial relationships.
Ediri Brume indicated no relevant financial relationships.
Thayer Hamoudah indicated no relevant financial relationships.
Sultan Ahmed, DO1, Nada Saleh, MD2, Abu Fahad Abbasi, MD3, Ammar Aqeel, MD4, Ediri Brume, MD2, Thayer Hamoudah, MD5. P1824 - The Liver That Broke the Belly: Abdominal Compartment Syndrome From Isolated Hepatomegaly, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Sultan Ahmed, DO1, Nada Saleh, MD2, Abu Fahad Abbasi, MD3, Ammar Aqeel, MD4, Ediri Brume, MD2, Thayer Hamoudah, MD5
1Mercyhealth Internal Medicine Residency, Rockford, IL; 2Mercy Health, Rockford, IL; 3Mercyhealth Gastroenterology Fellowship, Rockford, IL; 4Mercyhealth, Rockford, IL; 5Mercyhealth Gastroenterology, Rockford, IL
Introduction: Abdominal Compartment Syndrome (ACS) is defined as pressure in the abdomen > 20 mmHg, with signs of end-organ damage. Typically, this occurs due to increased intraabdominal pressure (IAP). Common culprits include massive fluid resuscitation, polytransfusion, hypothermia, coagulopathy, sepsis, and hepatic dysfunction with ascites. We present a rare case of isolated hepatomegaly resulting in devastating ACS.
Case Description/
Methods: A 26-year-old male with a history of alcohol use disorder presented with intractable, nontraumatic epistaxis and was found to have abnormal labs with AST 473 U/L, ALT 33 U/L, total bilirubin 3.3 mg/dL, ALP 372 U/L, INR 1.4, alcohol level 0.42 gm/dL, and lactic acid of 7.8 mmol/L. Exam revealed profound abdominal distension without a fluid wave. Imaging demonstrated severe hepatomegaly and steatosis with right-sided colonic thickening. Assessment of bladder pressure ranged from 15–25 mmHg, consistent with intra-abdominal hypertension and evolving ACS. The patient developed worsening lactic acidosis, hypotension requiring vasopressors, respiratory failure necessitating intubation, and renal failure requiring dialysis. Emergent decompressive laparotomy and right hemicolectomy were performed. Despite intervention, IAP remained elevated. Repeat laparotomy revealed patchy necrosis of the distal ileum and colon, prompting end ileostomy and further resection. The patient’s condition continued to deteriorate, and care was transitioned to comfort measures.
Discussion: Excessive fluid resuscitation is the most common cause of ACS. Hepatomegaly with ascites is also known to increase IAP; however, isolated hepatomegaly as the primary cause of ACS is extremely rare and has not been previously implicated. In this case, massive hepatomegaly acted as a space-occupying lesion, compressing abdominal organs, reducing abdominal wall compliance, and impairing venous return. These changes led to bowel edema, progressive elevation of IAP, and multiorgan dysfunction, including reduced cardiac output, impaired intestinal perfusion, hypoxemia, and renal failure. Although decompressive laparotomy typically lowers IAP, mortality remains high, and recovery of organ function is often unpredictable. Despite prompt and repeated decompression, the patient’s pressure remained elevated and organ failure worsened, highlighting the aggressive and refractory nature of ACS secondary to massive hepatomegaly. Early recognition and intervention are critical to improving outcomes.
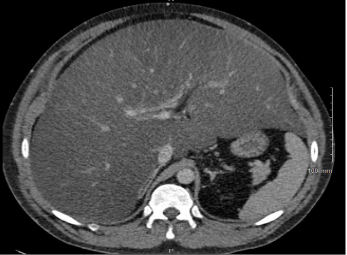
Figure: Figure 1: Demonstration of severe hepatomegaly with concomitant steatosis.

Figure: Figure 2: Re-demonstrated hepatomegaly with measurements: anterior-posterior diameter of the right hepatic lobe is 28 cm, the transverse diameter of the liver is 29 cm, and the cephalo-caudal length 33 cm.
Disclosures:
Sultan Ahmed indicated no relevant financial relationships.
Nada Saleh indicated no relevant financial relationships.
Abu Fahad Abbasi indicated no relevant financial relationships.
Ammar Aqeel indicated no relevant financial relationships.
Ediri Brume indicated no relevant financial relationships.
Thayer Hamoudah indicated no relevant financial relationships.
Sultan Ahmed, DO1, Nada Saleh, MD2, Abu Fahad Abbasi, MD3, Ammar Aqeel, MD4, Ediri Brume, MD2, Thayer Hamoudah, MD5. P1824 - The Liver That Broke the Belly: Abdominal Compartment Syndrome From Isolated Hepatomegaly, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

