Sunday Poster Session
Category: Liver
P1823 - Ruptured Liver Abscess With Transdiaphragmatic Extension Causing Pulmonary Abscess: A Rare Complication
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Kausar Bano, MBBS (she/her/hers)
Katihar Medical College Hospital
Katihar, Bihar, India
Presenting Author(s)
Kausar Bano, MBBS1, Madiha Haseeb, MBBS2, Ujjwal Mishra, MBBS3, Nikhil Jain, MBBS3, Mahendra Kumar, MBBS4, Rohan Raj, MBBS5, Neha Boski, MD, FRCR6
1Katihar Medical College Hospital, Katihar, Bihar, India; 2SUNY Downstate Health Sciences University, Brooklyn, NY; 3Uttar Pradesh University of Medical Sciences, Saifai, Etawah, Saifai, Uttar Pradesh, India; 4Sardar Patel Medical College, Bikaner, India, Bikaner, Rajasthan, India; 5Memorial Hospital at Gulfport, Gulfport, MS; 6Apollo Radiology International, Hyderabad, India, Hyderabad, Telangana, India
Introduction: Amoebic liver abscess is a common extraintestinal manifestation of Entamoeba histolytica in endemic regions. While most cases respond well to medical therapy, complications such as abscess rupture may occur, causing significant morbidity. We present a rare case of transdiaphragmatic extension of a ruptured liver abscess into the thoracic cavity, resulting in a secondary pulmonary abscess.
Case Description/
Methods: A 45-year-old man from India with chronic alcohol use presented with 20 days of epigastric pain, low-grade fever, and persistent dry cough. Examination revealed right upper quadrant tenderness and decreased breath sounds at the right lung base. Laboratory tests showed leukocytosis and mildly elevated liver enzymes.
An abdominal ultrasound revealed a subcapsular hepatic lesion. Contrast-enhanced CT demonstrated a thick-walled, bilocular abscess in segment VII with central liquefaction and a double halo sign. A focal defect in the posterior abscess wall allowed the extension of purulent material through the diaphragm into the right subdiaphragmatic space, with a second collection at the right lung base, indicating direct transdiaphragmatic spread.
Aspiration of both hepatic and thoracic collections yielded anchovy sauce-like pus. Serology was positive for E. histolytica antibodies; bacterial cultures were sterile. The diagnosis of ruptured amoebic liver abscess with secondary pulmonary abscess was confirmed. The patient received intravenous metronidazole and a luminal agent. Pigtail catheters were inserted into the hepatic and subdiaphragmatic cavities, and the pulmonary abscess was aspirated under ultrasound guidance. The patient showed marked clinical improvement, and follow-up imaging at two weeks showed significant resolution.
Discussion: Subcapsular hepatic abscesses, particularly in the posterior segments, are vulnerable to rupture into adjacent compartments. When diaphragmatic defects are present, transdiaphragmatic spread can result in rare complications such as pulmonary abscesses. This case highlights the value of cross-sectional imaging in identifying anatomical pathways of disease extension and guiding minimally invasive interventions. From a gastroenterology perspective, high clinical suspicion, timely imaging, and early drainage in addition to anti-amoebic therapy are critical to preventing life-threatening sequelae.
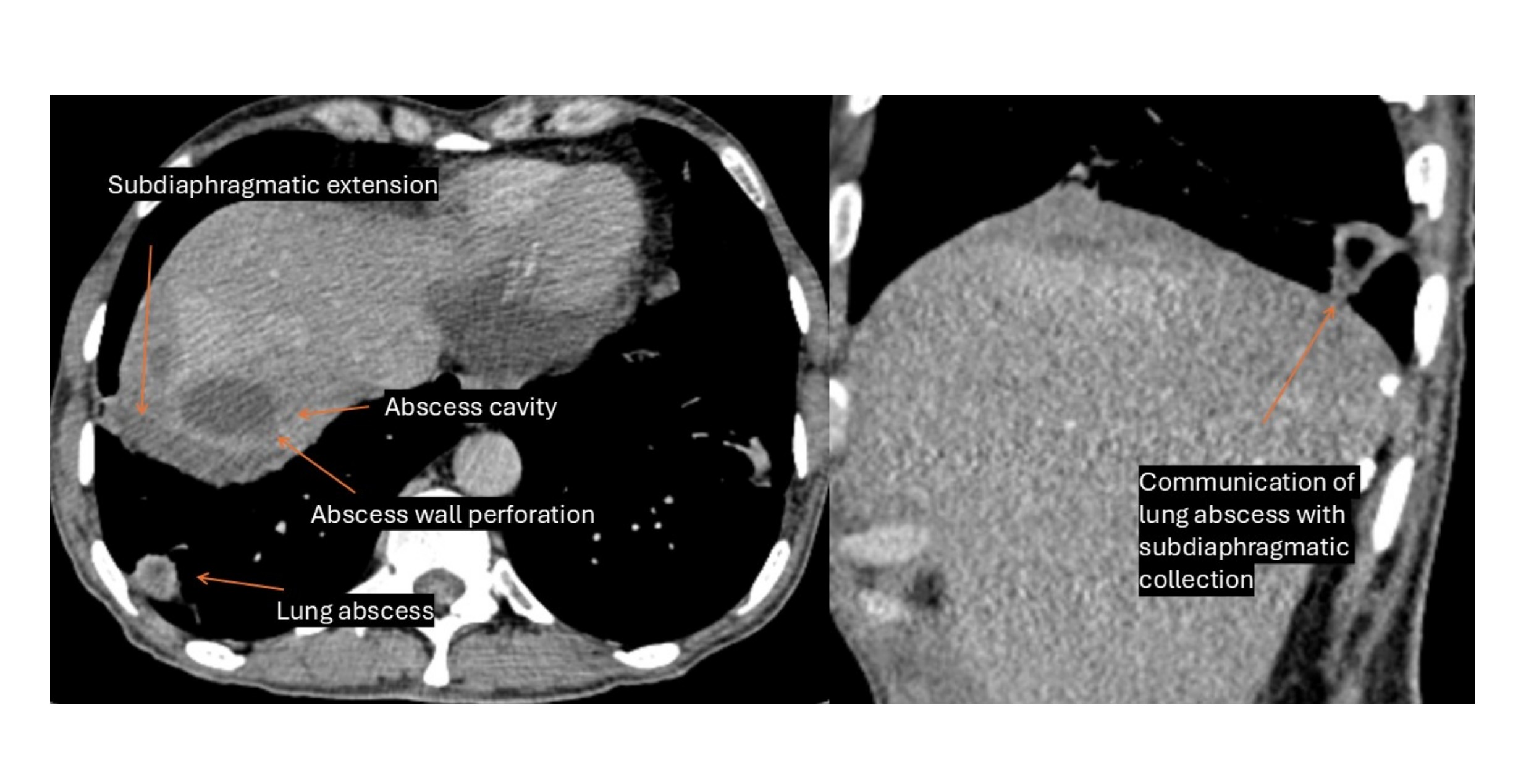
Figure: The image on the left shows a ruptured subcapsular liver abscess in segment VII, with the extension of its contents into the right subdiaphragmatic space. The image on the right demonstrates a secondary pulmonary abscess at the right lung base, in direct continuity with the subdiaphragmatic collection—indicative of transdiaphragmatic spread.
Disclosures:
Kausar Bano indicated no relevant financial relationships.
Madiha Haseeb indicated no relevant financial relationships.
Ujjwal Mishra indicated no relevant financial relationships.
Nikhil Jain indicated no relevant financial relationships.
Mahendra Kumar indicated no relevant financial relationships.
Rohan Raj indicated no relevant financial relationships.
Neha Boski indicated no relevant financial relationships.
Kausar Bano, MBBS1, Madiha Haseeb, MBBS2, Ujjwal Mishra, MBBS3, Nikhil Jain, MBBS3, Mahendra Kumar, MBBS4, Rohan Raj, MBBS5, Neha Boski, MD, FRCR6. P1823 - Ruptured Liver Abscess With Transdiaphragmatic Extension Causing Pulmonary Abscess: A Rare Complication, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Katihar Medical College Hospital, Katihar, Bihar, India; 2SUNY Downstate Health Sciences University, Brooklyn, NY; 3Uttar Pradesh University of Medical Sciences, Saifai, Etawah, Saifai, Uttar Pradesh, India; 4Sardar Patel Medical College, Bikaner, India, Bikaner, Rajasthan, India; 5Memorial Hospital at Gulfport, Gulfport, MS; 6Apollo Radiology International, Hyderabad, India, Hyderabad, Telangana, India
Introduction: Amoebic liver abscess is a common extraintestinal manifestation of Entamoeba histolytica in endemic regions. While most cases respond well to medical therapy, complications such as abscess rupture may occur, causing significant morbidity. We present a rare case of transdiaphragmatic extension of a ruptured liver abscess into the thoracic cavity, resulting in a secondary pulmonary abscess.
Case Description/
Methods: A 45-year-old man from India with chronic alcohol use presented with 20 days of epigastric pain, low-grade fever, and persistent dry cough. Examination revealed right upper quadrant tenderness and decreased breath sounds at the right lung base. Laboratory tests showed leukocytosis and mildly elevated liver enzymes.
An abdominal ultrasound revealed a subcapsular hepatic lesion. Contrast-enhanced CT demonstrated a thick-walled, bilocular abscess in segment VII with central liquefaction and a double halo sign. A focal defect in the posterior abscess wall allowed the extension of purulent material through the diaphragm into the right subdiaphragmatic space, with a second collection at the right lung base, indicating direct transdiaphragmatic spread.
Aspiration of both hepatic and thoracic collections yielded anchovy sauce-like pus. Serology was positive for E. histolytica antibodies; bacterial cultures were sterile. The diagnosis of ruptured amoebic liver abscess with secondary pulmonary abscess was confirmed. The patient received intravenous metronidazole and a luminal agent. Pigtail catheters were inserted into the hepatic and subdiaphragmatic cavities, and the pulmonary abscess was aspirated under ultrasound guidance. The patient showed marked clinical improvement, and follow-up imaging at two weeks showed significant resolution.
Discussion: Subcapsular hepatic abscesses, particularly in the posterior segments, are vulnerable to rupture into adjacent compartments. When diaphragmatic defects are present, transdiaphragmatic spread can result in rare complications such as pulmonary abscesses. This case highlights the value of cross-sectional imaging in identifying anatomical pathways of disease extension and guiding minimally invasive interventions. From a gastroenterology perspective, high clinical suspicion, timely imaging, and early drainage in addition to anti-amoebic therapy are critical to preventing life-threatening sequelae.
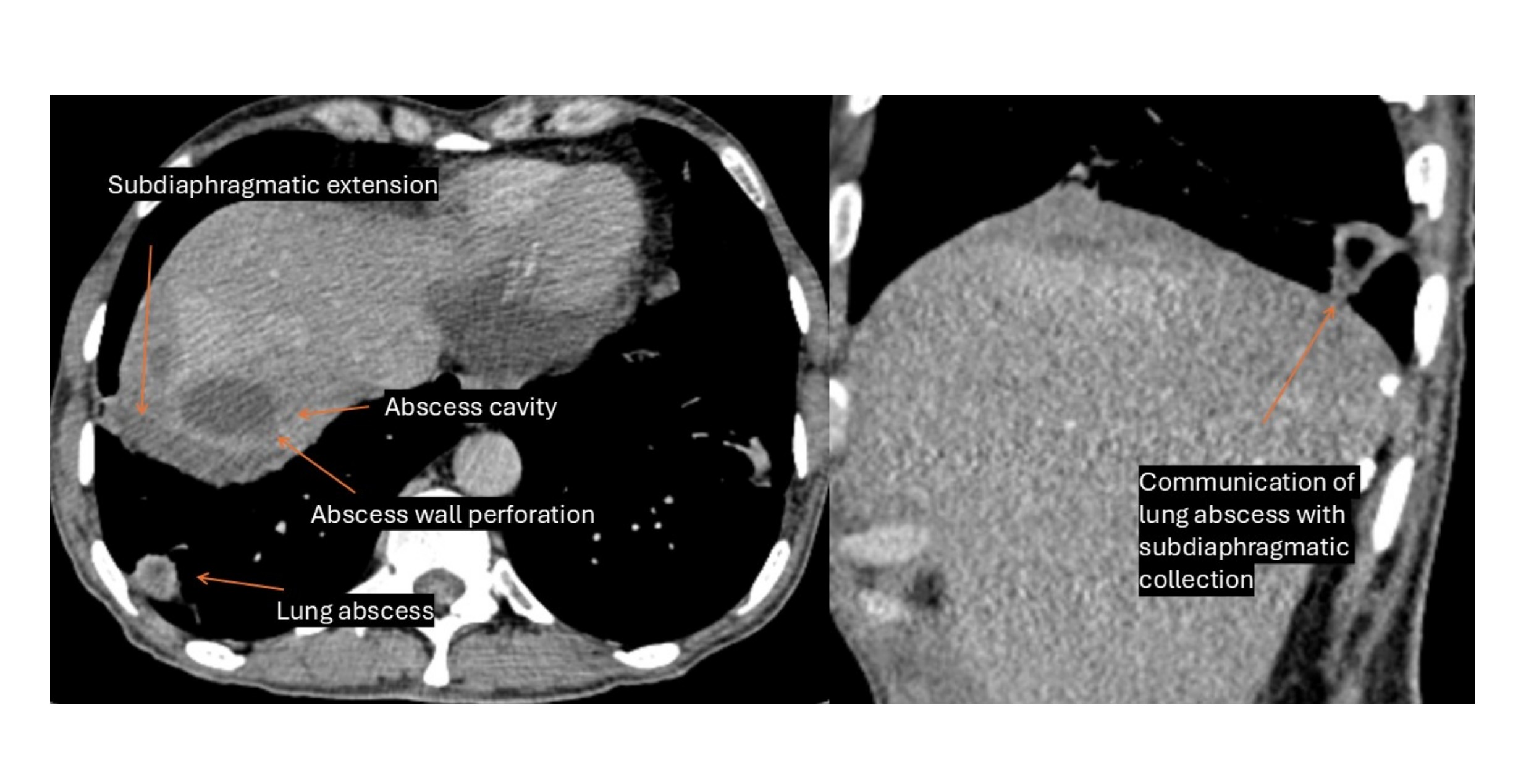
Figure: The image on the left shows a ruptured subcapsular liver abscess in segment VII, with the extension of its contents into the right subdiaphragmatic space. The image on the right demonstrates a secondary pulmonary abscess at the right lung base, in direct continuity with the subdiaphragmatic collection—indicative of transdiaphragmatic spread.
Disclosures:
Kausar Bano indicated no relevant financial relationships.
Madiha Haseeb indicated no relevant financial relationships.
Ujjwal Mishra indicated no relevant financial relationships.
Nikhil Jain indicated no relevant financial relationships.
Mahendra Kumar indicated no relevant financial relationships.
Rohan Raj indicated no relevant financial relationships.
Neha Boski indicated no relevant financial relationships.
Kausar Bano, MBBS1, Madiha Haseeb, MBBS2, Ujjwal Mishra, MBBS3, Nikhil Jain, MBBS3, Mahendra Kumar, MBBS4, Rohan Raj, MBBS5, Neha Boski, MD, FRCR6. P1823 - Ruptured Liver Abscess With Transdiaphragmatic Extension Causing Pulmonary Abscess: A Rare Complication, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
