Sunday Poster Session
Category: Liver
P1822 - A Case of Atypical Amoebic Liver Abscess With Negative Serologies
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Rebhi Rabah, MD (he/him/his)
SUNY Downstate Health Sciences University
Brooklyn, NY
Presenting Author(s)
Rebhi Rabah, MD1, Fariha Chowdhury, MD2, Ekenedilichukwu Nnadi, MD1, Kevin Han, MD3, Viknesh Baskar, BA1, Olusegun Bankole, MD4
1SUNY Downstate Health Sciences University, Brooklyn, NY; 2Garnet Health Medical Center, Brooklyn, NY; 3SUNY Downstate Health Sciences University, New York, NY; 4NYC Health + Hospitals/Kings County, Brooklyn, NY
Introduction: Entamoeba histolytica (E. histolytica) is protozoal parasite that causes amoebiasis, which is an enteric infection with a wide variety of presentations. The infection is transmitted fecal-orally when the organism is in cystic form. Once ingested it takes the form of an invasive trophozoite, which can invade the colonic mucosa and spread to other organs through portal circulation. Amoebiasis is most prevalent in developing countries with poor sanitation. We present a case of a 62-year-old man diagnosed with amoebic liver abscess despite no travel history in 3 years and negative initial serology for E. histolytica.
Case Description/
Methods: A 62-year-old Nigerian American male with history of type 2 diabetes, hypertension, stage 3 chronic kidney disease presented endorsing intermittent fever, malaise, diarrhea, and abdominal pain for the last 10-days. Vitals revealed a fever of 101.3° F. Physical exam was significant for pleuritic right upper quadrant pain. Chart review revealed 12 pounds of weight loss since last clinic visit 3 weeks ago. Patient denied any recent travel over the last 3 years, alcohol use, or high-risk sexual behaviors. Labs were significant for leukocytosis to 26,000 cells/µL with neutrophil predominance. Liver enzymes were mildly elevated with normal total bilirubin. Stool studies were negative for signs of active infections. E. histolytica serology was negative. Blood cultures grew Klebsiella pneumoniae, prompting empiric ceftriaxone. CT of the abdomen revealed a heterogenous 8.5 cm mass in the right lobe of the liver. Percutaneous biopsy showed necrotic debris and inflammatory cells but no malignant cells. The patient continued to spike fevers despite therapy. Ultrasound-guided drainage yielded 200 mL of anchovy paste like pus. PCR testing of aspirate confirmed E. histolytica, overriding negative serology. Therapy was adjusted to metronidazole and patient recovered.
Discussion: In developed countries, amoebiasis is generally seen in travelers from endemic areas. However, our patient had not travelled outside of the country in over 3 years, raising concern for delayed clinical manifestation or local transmission. This case also exemplifies how negative initial stool, and serologic test can create a diagnostic challenge. Though rare, false negatives serologic testing for E. histolytica can occur in immunocompromised patients. This case highlights the importance of maintaining a high index of suspicion for amebiasis in the absence of recent travel or positive serologies.
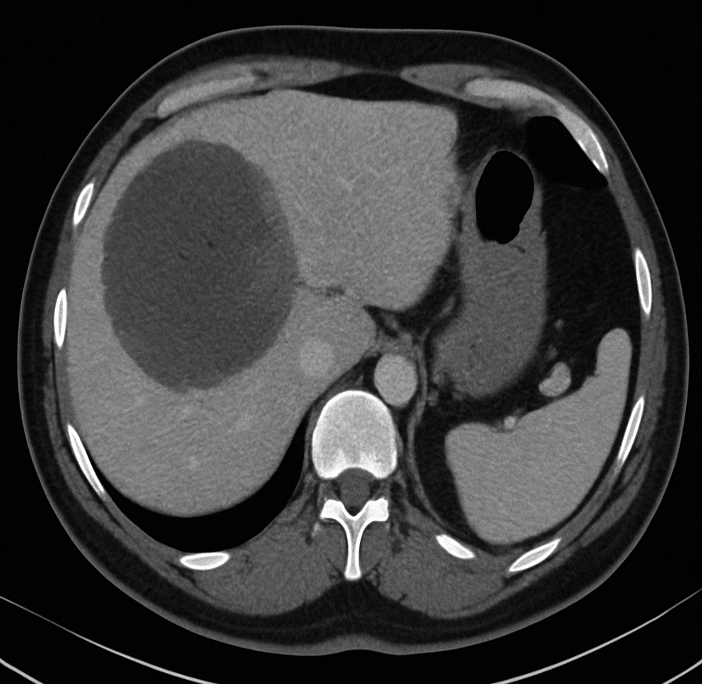
Figure: Figure 1. CT Abdomen revealing a 8.5 cm mass in the right lobe of the liver.
Disclosures:
Rebhi Rabah indicated no relevant financial relationships.
Fariha Chowdhury indicated no relevant financial relationships.
Ekenedilichukwu Nnadi indicated no relevant financial relationships.
Kevin Han indicated no relevant financial relationships.
Viknesh Baskar indicated no relevant financial relationships.
Olusegun Bankole indicated no relevant financial relationships.
Rebhi Rabah, MD1, Fariha Chowdhury, MD2, Ekenedilichukwu Nnadi, MD1, Kevin Han, MD3, Viknesh Baskar, BA1, Olusegun Bankole, MD4. P1822 - A Case of Atypical Amoebic Liver Abscess With Negative Serologies, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SUNY Downstate Health Sciences University, Brooklyn, NY; 2Garnet Health Medical Center, Brooklyn, NY; 3SUNY Downstate Health Sciences University, New York, NY; 4NYC Health + Hospitals/Kings County, Brooklyn, NY
Introduction: Entamoeba histolytica (E. histolytica) is protozoal parasite that causes amoebiasis, which is an enteric infection with a wide variety of presentations. The infection is transmitted fecal-orally when the organism is in cystic form. Once ingested it takes the form of an invasive trophozoite, which can invade the colonic mucosa and spread to other organs through portal circulation. Amoebiasis is most prevalent in developing countries with poor sanitation. We present a case of a 62-year-old man diagnosed with amoebic liver abscess despite no travel history in 3 years and negative initial serology for E. histolytica.
Case Description/
Methods: A 62-year-old Nigerian American male with history of type 2 diabetes, hypertension, stage 3 chronic kidney disease presented endorsing intermittent fever, malaise, diarrhea, and abdominal pain for the last 10-days. Vitals revealed a fever of 101.3° F. Physical exam was significant for pleuritic right upper quadrant pain. Chart review revealed 12 pounds of weight loss since last clinic visit 3 weeks ago. Patient denied any recent travel over the last 3 years, alcohol use, or high-risk sexual behaviors. Labs were significant for leukocytosis to 26,000 cells/µL with neutrophil predominance. Liver enzymes were mildly elevated with normal total bilirubin. Stool studies were negative for signs of active infections. E. histolytica serology was negative. Blood cultures grew Klebsiella pneumoniae, prompting empiric ceftriaxone. CT of the abdomen revealed a heterogenous 8.5 cm mass in the right lobe of the liver. Percutaneous biopsy showed necrotic debris and inflammatory cells but no malignant cells. The patient continued to spike fevers despite therapy. Ultrasound-guided drainage yielded 200 mL of anchovy paste like pus. PCR testing of aspirate confirmed E. histolytica, overriding negative serology. Therapy was adjusted to metronidazole and patient recovered.
Discussion: In developed countries, amoebiasis is generally seen in travelers from endemic areas. However, our patient had not travelled outside of the country in over 3 years, raising concern for delayed clinical manifestation or local transmission. This case also exemplifies how negative initial stool, and serologic test can create a diagnostic challenge. Though rare, false negatives serologic testing for E. histolytica can occur in immunocompromised patients. This case highlights the importance of maintaining a high index of suspicion for amebiasis in the absence of recent travel or positive serologies.
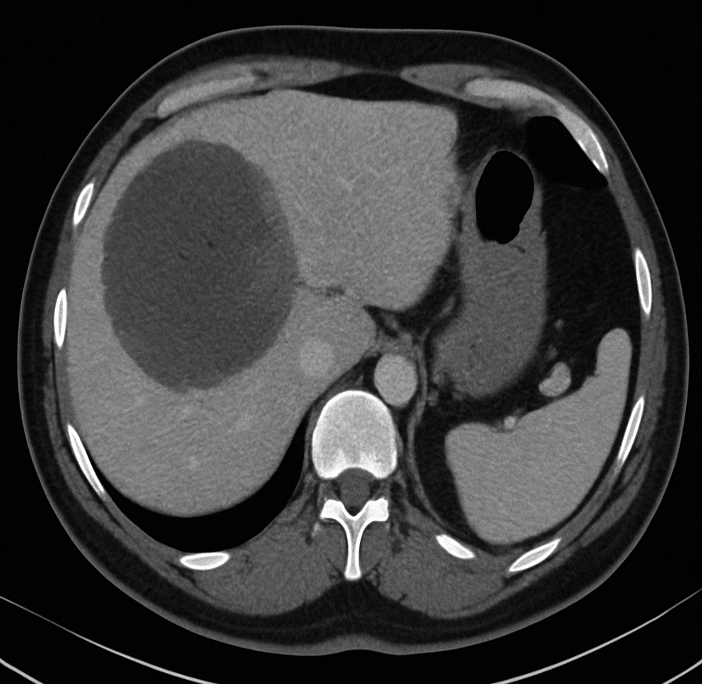
Figure: Figure 1. CT Abdomen revealing a 8.5 cm mass in the right lobe of the liver.
Disclosures:
Rebhi Rabah indicated no relevant financial relationships.
Fariha Chowdhury indicated no relevant financial relationships.
Ekenedilichukwu Nnadi indicated no relevant financial relationships.
Kevin Han indicated no relevant financial relationships.
Viknesh Baskar indicated no relevant financial relationships.
Olusegun Bankole indicated no relevant financial relationships.
Rebhi Rabah, MD1, Fariha Chowdhury, MD2, Ekenedilichukwu Nnadi, MD1, Kevin Han, MD3, Viknesh Baskar, BA1, Olusegun Bankole, MD4. P1822 - A Case of Atypical Amoebic Liver Abscess With Negative Serologies, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
