Sunday Poster Session
Category: Liver
P1814 - LECT2 Be Honest: This Wasn't Cirrhosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- JR
Jarrett Rong, MD (he/him/his)
McGovern Medical School at UTHealth Houston
Houston, TX
Presenting Author(s)
Andrew T. Sullivan, MD, Jarrett Rong, MD, Eric D. Yoon, MD, Maneera T. Chopra, MD, Bihong Zhao, MD, PhD, Erin Rubin, MD, Victor I. Machicao, MD
McGovern Medical School at UTHealth Houston, Houston, TX
Introduction: LECT2 (leukocyte chemotactic factor 2) amyloidosis, a rare underrecognized form of hepatic amyloidosis, results from the misfolded LECT2 protein. Unlike other forms of amyloidosis, LECT2 is produced by the liver and tends to accumulate in the liver and kidneys, with relative sparing of the heart. Its hepatic manifestation can mimic cirrhosis or congestive hepatopathy, often leading to diagnostic uncertainty. This case highlights the crucial role of liver biopsy in distinguishing LECT2 amyloidosis from cirrhosis, a distinction that directly impacts transplant evaluation in patients with multisystem involvement.
Case Description/
Methods: The patient is a 64-year-old woman with a history of rheumatic valvular heart disease status post mechanical aortic valve replacement and mitral valve repair. She presented in cardiogenic shock, complicated by acute hepatic and renal failure. Initial labs revealed ALT 1,187 U/L, AST 550 U/L, total bilirubin 3.3 mg/dL, LDH 1,607 U/L, and INR 3.43. Transthoracic echocardiogram showed severe postcapillary pulmonary hypertension, critical aortic stenosis (mean gradient 60 mmHg), and a paravalvular mitral leak. Right heart catheterization confirmed elevated filling pressures. Abdominal CT and liver elastography demonstrated cirrhotic morphology (Metavir F3–F4). Liver biopsy revealed amyloid deposits with Congo red staining, and mass spectrometry confirmed LECT2 amyloidosis. Given her severe biventricular heart failure, biopsy-proven hepatic amyloidosis, pulmonary hypertension, and chronic kidney disease, she was referred for multi-organ transplant evaluation.
Discussion: Accurate differentiation of amyloid-related liver disease from cirrhosis is critical, as misclassification may significantly impact transplant candidacy and management. This patient was admitted for multiorgan transplant evaluation but was initially deemed ineligible due to presumed cirrhosis based on ultrasound and elastography findings. Fluctuating liver function, initially attributed to ischemic hepatitis, further complicated the clinical picture by obscuring the contribution of amyloid infiltration. However, liver biopsy revealed LECT2 amyloid deposition in the absence of cirrhosis—a diagnosis with important implications for transplant eligibility. Although LECT2 amyloidosis typically spares the heart, the potential for recurrence in transplanted organs warrants consideration and may represent an emerging area for future investigation.
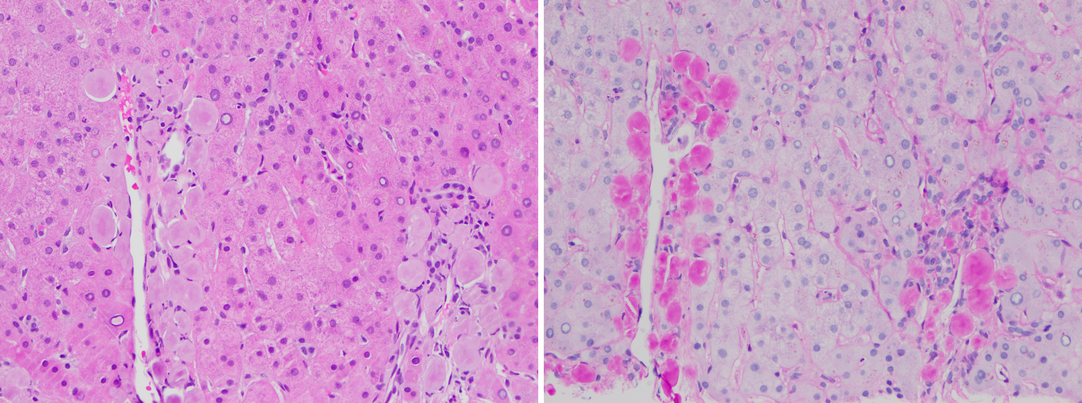
Figure: Figure 1: Histologic features of hepatic LECT2 amyloidosis (20×).
Left: H&E stain shows amorphous eosinophilic deposits within portal tracts.
Right: PAS-D stain reveals PAS-negative material with preserved basement membranes, consistent with amyloid.

Figure: Figure 2: Trichrome Stain illustrating amyloid deposition along the portal tracts.
Disclosures:
Andrew Sullivan indicated no relevant financial relationships.
Jarrett Rong indicated no relevant financial relationships.
Eric Yoon indicated no relevant financial relationships.
Maneera Chopra indicated no relevant financial relationships.
Bihong Zhao indicated no relevant financial relationships.
Erin Rubin indicated no relevant financial relationships.
Victor Machicao indicated no relevant financial relationships.
Andrew T. Sullivan, MD, Jarrett Rong, MD, Eric D. Yoon, MD, Maneera T. Chopra, MD, Bihong Zhao, MD, PhD, Erin Rubin, MD, Victor I. Machicao, MD. P1814 - LECT2 Be Honest: This Wasn't Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
McGovern Medical School at UTHealth Houston, Houston, TX
Introduction: LECT2 (leukocyte chemotactic factor 2) amyloidosis, a rare underrecognized form of hepatic amyloidosis, results from the misfolded LECT2 protein. Unlike other forms of amyloidosis, LECT2 is produced by the liver and tends to accumulate in the liver and kidneys, with relative sparing of the heart. Its hepatic manifestation can mimic cirrhosis or congestive hepatopathy, often leading to diagnostic uncertainty. This case highlights the crucial role of liver biopsy in distinguishing LECT2 amyloidosis from cirrhosis, a distinction that directly impacts transplant evaluation in patients with multisystem involvement.
Case Description/
Methods: The patient is a 64-year-old woman with a history of rheumatic valvular heart disease status post mechanical aortic valve replacement and mitral valve repair. She presented in cardiogenic shock, complicated by acute hepatic and renal failure. Initial labs revealed ALT 1,187 U/L, AST 550 U/L, total bilirubin 3.3 mg/dL, LDH 1,607 U/L, and INR 3.43. Transthoracic echocardiogram showed severe postcapillary pulmonary hypertension, critical aortic stenosis (mean gradient 60 mmHg), and a paravalvular mitral leak. Right heart catheterization confirmed elevated filling pressures. Abdominal CT and liver elastography demonstrated cirrhotic morphology (Metavir F3–F4). Liver biopsy revealed amyloid deposits with Congo red staining, and mass spectrometry confirmed LECT2 amyloidosis. Given her severe biventricular heart failure, biopsy-proven hepatic amyloidosis, pulmonary hypertension, and chronic kidney disease, she was referred for multi-organ transplant evaluation.
Discussion: Accurate differentiation of amyloid-related liver disease from cirrhosis is critical, as misclassification may significantly impact transplant candidacy and management. This patient was admitted for multiorgan transplant evaluation but was initially deemed ineligible due to presumed cirrhosis based on ultrasound and elastography findings. Fluctuating liver function, initially attributed to ischemic hepatitis, further complicated the clinical picture by obscuring the contribution of amyloid infiltration. However, liver biopsy revealed LECT2 amyloid deposition in the absence of cirrhosis—a diagnosis with important implications for transplant eligibility. Although LECT2 amyloidosis typically spares the heart, the potential for recurrence in transplanted organs warrants consideration and may represent an emerging area for future investigation.
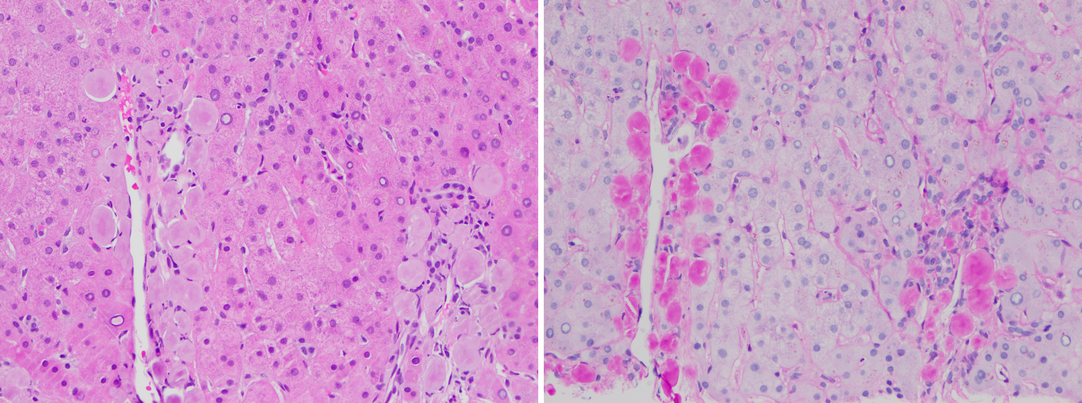
Figure: Figure 1: Histologic features of hepatic LECT2 amyloidosis (20×).
Left: H&E stain shows amorphous eosinophilic deposits within portal tracts.
Right: PAS-D stain reveals PAS-negative material with preserved basement membranes, consistent with amyloid.

Figure: Figure 2: Trichrome Stain illustrating amyloid deposition along the portal tracts.
Disclosures:
Andrew Sullivan indicated no relevant financial relationships.
Jarrett Rong indicated no relevant financial relationships.
Eric Yoon indicated no relevant financial relationships.
Maneera Chopra indicated no relevant financial relationships.
Bihong Zhao indicated no relevant financial relationships.
Erin Rubin indicated no relevant financial relationships.
Victor Machicao indicated no relevant financial relationships.
Andrew T. Sullivan, MD, Jarrett Rong, MD, Eric D. Yoon, MD, Maneera T. Chopra, MD, Bihong Zhao, MD, PhD, Erin Rubin, MD, Victor I. Machicao, MD. P1814 - LECT2 Be Honest: This Wasn't Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

