Sunday Poster Session
Category: Liver
P1810 - Refractory Status Epilepticus From Severe Hyperammonemia Following TIPS
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Varun Vemulapalli, MD
McGovern Medical School at UTHealth
Houston, TX
Presenting Author(s)
Varun Vemulapalli, MD1, Cristina Natha, MD1, Aran Farrell, MD1, Jimmy Pham, MD1, Ranya Selim, MD2
1McGovern Medical School at UTHealth, Houston, TX; 2University of Texas Health Science Center, Houston, TX
Introduction: Transjugular intrahepatic portosystemic shunt (TIPS) is a well-established intervention for managing complications of portal hypertension, including variceal bleeding. While hepatic encephalopathy is a known post-TIPS complication, seizures and status epilepticus due to hyperammonemia are exceedingly rare and remain poorly described. Increased clinical awareness of this neurologic complication is key to timely recognition and management.
Case Description/
Methods: A 59-year-old male with alcoholic cirrhosis and esophageal varices presented with massive hematemesis. Initial esophagogastroduodenoscopy (EGD) was limited by extensive clot burden. Repeat EGD revealed bleeding esophageal varices that could not be banded. Due to ongoing hemorrhage, the patient was intubated for airway protection and underwent emergent TIPS placement. Within 24 hours of the procedure, he developed generalized tonic-clonic seizures requiring re-intubation. Serum ammonia level was critically elevated at 1,049 μmol/L. CT head was unremarkable. Despite aggressive treatment—including high-dose benzodiazepines, propofol, levetiracetam, lacosamide, and eventually pentobarbital—the patient remained in refractory status epilepticus. Continuous renal replacement therapy (CRRT) was initiated for ammonia clearance, and electroencephalogram (EEG) demonstrated persistent epileptiform activity. Given the severity of neurologic injury, lack of clinical improvement, and poor prognosis, the family elected to pursue comfort care. The patient was palliatively extubated and passed away shortly thereafter.
Discussion: This case illustrates a rare and severe neurologic complication following TIPS: refractory status epilepticus secondary to hyperammonemia. While post-TIPS hepatic encephalopathy is a known risk, seizure activity is not commonly anticipated. Ammonia levels are not routinely monitored post-procedure, yet extreme elevations may result in rapid neurologic decline. Early signs of hyperammonemia may be easily overlooked or misattributed to sedation or baseline encephalopathy. Prompt recognition of severe ammonia elevation, consideration of EEG in unexplained neurologic decline, early initiation of therapies such as CRRT, and downsizing of TIPS if all else fails, may be critical in preventing irreversible outcomes. Increased awareness of this rare but potentially fatal complication is critical for early intervention and may inform future guidelines for post-TIPS monitoring.
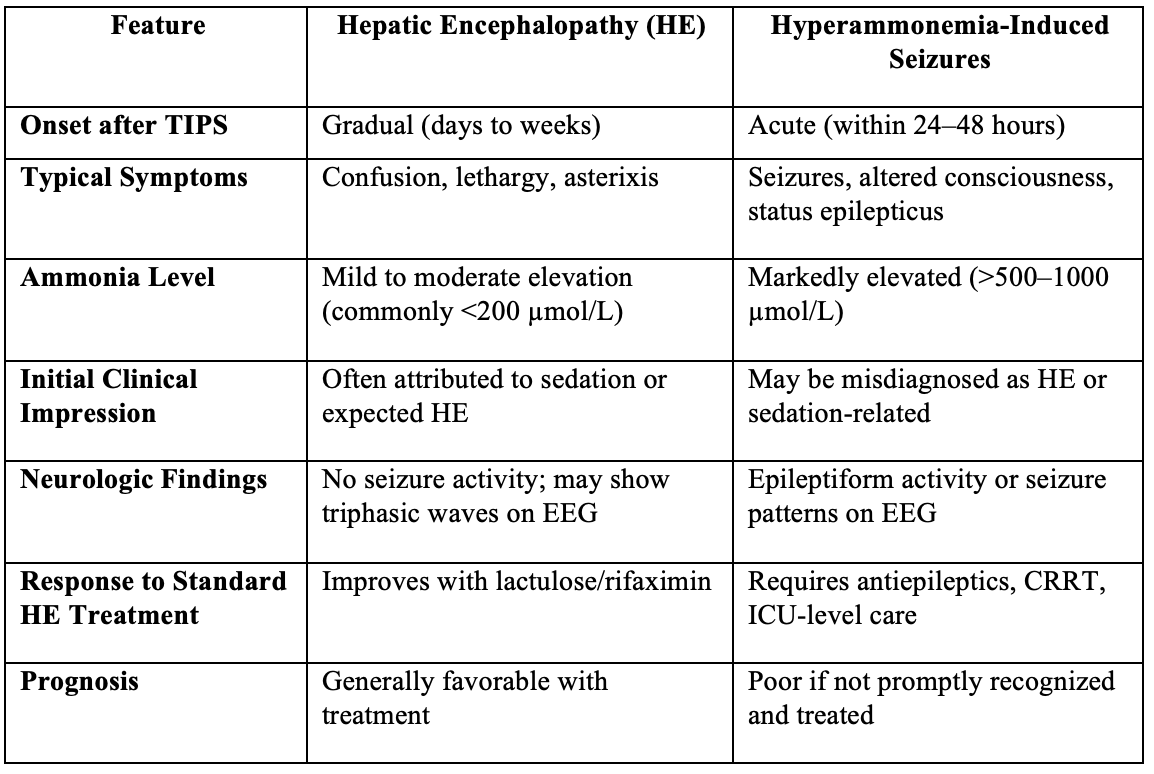
Figure: Distinguishing Hepatic Encephalopathy from Hyperammonemia-Induced Seizures After TIPS
Disclosures:
Varun Vemulapalli indicated no relevant financial relationships.
Cristina Natha indicated no relevant financial relationships.
Aran Farrell indicated no relevant financial relationships.
Jimmy Pham indicated no relevant financial relationships.
Ranya Selim indicated no relevant financial relationships.
Varun Vemulapalli, MD1, Cristina Natha, MD1, Aran Farrell, MD1, Jimmy Pham, MD1, Ranya Selim, MD2. P1810 - Refractory Status Epilepticus From Severe Hyperammonemia Following TIPS, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1McGovern Medical School at UTHealth, Houston, TX; 2University of Texas Health Science Center, Houston, TX
Introduction: Transjugular intrahepatic portosystemic shunt (TIPS) is a well-established intervention for managing complications of portal hypertension, including variceal bleeding. While hepatic encephalopathy is a known post-TIPS complication, seizures and status epilepticus due to hyperammonemia are exceedingly rare and remain poorly described. Increased clinical awareness of this neurologic complication is key to timely recognition and management.
Case Description/
Methods: A 59-year-old male with alcoholic cirrhosis and esophageal varices presented with massive hematemesis. Initial esophagogastroduodenoscopy (EGD) was limited by extensive clot burden. Repeat EGD revealed bleeding esophageal varices that could not be banded. Due to ongoing hemorrhage, the patient was intubated for airway protection and underwent emergent TIPS placement. Within 24 hours of the procedure, he developed generalized tonic-clonic seizures requiring re-intubation. Serum ammonia level was critically elevated at 1,049 μmol/L. CT head was unremarkable. Despite aggressive treatment—including high-dose benzodiazepines, propofol, levetiracetam, lacosamide, and eventually pentobarbital—the patient remained in refractory status epilepticus. Continuous renal replacement therapy (CRRT) was initiated for ammonia clearance, and electroencephalogram (EEG) demonstrated persistent epileptiform activity. Given the severity of neurologic injury, lack of clinical improvement, and poor prognosis, the family elected to pursue comfort care. The patient was palliatively extubated and passed away shortly thereafter.
Discussion: This case illustrates a rare and severe neurologic complication following TIPS: refractory status epilepticus secondary to hyperammonemia. While post-TIPS hepatic encephalopathy is a known risk, seizure activity is not commonly anticipated. Ammonia levels are not routinely monitored post-procedure, yet extreme elevations may result in rapid neurologic decline. Early signs of hyperammonemia may be easily overlooked or misattributed to sedation or baseline encephalopathy. Prompt recognition of severe ammonia elevation, consideration of EEG in unexplained neurologic decline, early initiation of therapies such as CRRT, and downsizing of TIPS if all else fails, may be critical in preventing irreversible outcomes. Increased awareness of this rare but potentially fatal complication is critical for early intervention and may inform future guidelines for post-TIPS monitoring.
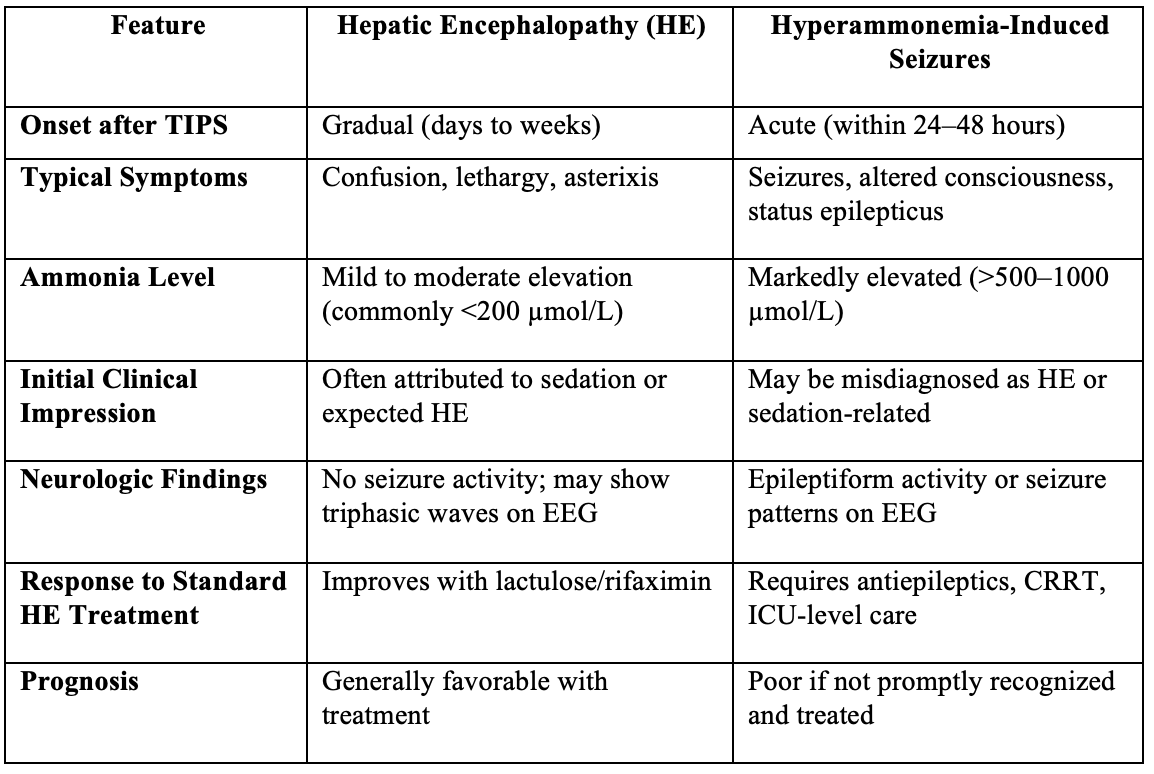
Figure: Distinguishing Hepatic Encephalopathy from Hyperammonemia-Induced Seizures After TIPS
Disclosures:
Varun Vemulapalli indicated no relevant financial relationships.
Cristina Natha indicated no relevant financial relationships.
Aran Farrell indicated no relevant financial relationships.
Jimmy Pham indicated no relevant financial relationships.
Ranya Selim indicated no relevant financial relationships.
Varun Vemulapalli, MD1, Cristina Natha, MD1, Aran Farrell, MD1, Jimmy Pham, MD1, Ranya Selim, MD2. P1810 - Refractory Status Epilepticus From Severe Hyperammonemia Following TIPS, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
