Sunday Poster Session
Category: Liver
P1801 - Liver Caught in the Storm: A Relapsing Case of HLH-Associated Severe Acute Liver Injury
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- EJ
Efan Jawad, MD (she/her/hers)
UT Health Science Center San Antonio
San Antonio, TX
Presenting Author(s)
Owais Syed, MD1, Efan Jawad, MD1, Courtney Thomas, DO2, Eugenia Tsai, MD3, Lisa D. Pedicone, PhD3, Fabian Rodas, MD2, Carmen Landaverde, MD3, Andres Gomez-Aldana, MD2, Eric Lawitz, MD2, Fred Poordad, MD3, Jan Petrasek, MD, PhD3
1UT Health Science Center San Antonio, San Antonio, TX; 2University of Texas Health San Antonio, San Antonio, TX; 3Texas Liver Institute, Austin, TX
Introduction: Hemophagocytic lymphohistiocytosis (HLH) is a rare and life-threatening hyperinflammatory syndrome characterized by uncontrolled cytokine release and multi-organ dysfunction. We present a challenging case of acute liver injury in a patient with relapsing HLH.
Case Description/
Methods: A 72-year-old female presented with fevers, jaundice and pancytopenia. Initial labs revealed AST 1361 U/L, ALT 587 U/L and total bilirubin (TB) 17.8 mg/dL and ALP 429 U/L. Ferritin was markedly elevated at 11,221 ng/mL. Imaging showed splenomegaly, and her soluble CD25 level was 35,000 U/mL. Liver biopsy demonstrated features consistent with HLH. She was treated with etoposide and dexamethasone with improvement of symptoms and normalization of liver enzymes. Four months later, she returned with arthralgias, myalgias and recurrent elevation of liver enzymes with AST 1554 U/L, ALT >3500 U/L and TB 5.9 mg/dL. Repeat liver biopsy demonstrated small clusters of histiocytes and portal/lobular changes consistent with HLH relapse (Figure 1, 2). She was retreated with etoposide, dexamethasone and cyclosporine with resolution of symptoms and biochemical improvement. Maintenance therapy was initiated with cyclosporine, dexamethasone and etoposide. However, one month later she presented with worsening liver tests (AST 1547 U/L, ALT 2316 U/L, TB 16 mg/dL), developed septic shock secondary from E. Coli bacteremia, and passed away during the hospitalization.
Discussion: Liver involvement in HLH is multifactorial, driven by cytokine-mediated injury, hemophagocytosis, and systemic inflammation. This case highlights the diagnostic and therapeutic complexities of HLH with liver involvement. The patient met six of the eight diagnostic criteria, including fever >38.5°C, splenomegaly, cytopenias in ≥2 cell lines, elevated ferritin, hypertriglyceridemia, and elevated soluble CD25. Liver biopsy revealed classic features of HLH, including histiocytic infiltrates and portal tract injury. Despite initial improvement with treatment, her subsequent relapses and eventual death emphasize the aggressive nature of HLH and the challenges of long-term management. This case underscores the importance of early recognition, prompt intervention, and continued investigation into effective maintenance strategies, particularly in older patients.
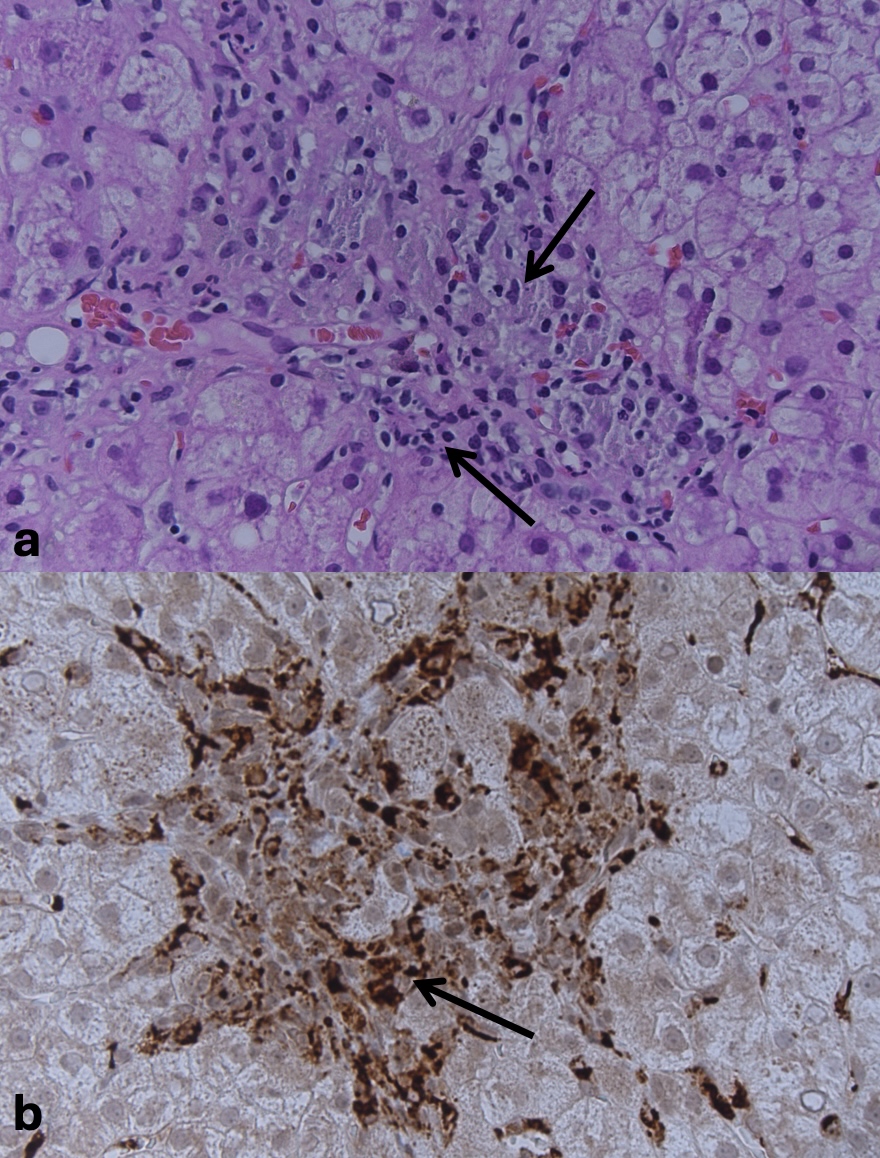
Figure: Liver biopsy demonstrated (a) Clusters of macrophages with two types of nuclei: smaller condensed lymphocyte nuclei and larger irregular macrophage nuclei on H&E stain (200X magnification) (b) CD68 stain highlights macrophages (200X magnification)
Disclosures:
Owais Syed indicated no relevant financial relationships.
Efan Jawad indicated no relevant financial relationships.
Courtney Thomas indicated no relevant financial relationships.
Eugenia Tsai indicated no relevant financial relationships.
Lisa D. Pedicone indicated no relevant financial relationships.
Fabian Rodas indicated no relevant financial relationships.
Carmen Landaverde indicated no relevant financial relationships.
Andres Gomez-Aldana indicated no relevant financial relationships.
Eric Lawitz indicated no relevant financial relationships.
Fred Poordad indicated no relevant financial relationships.
Jan Petrasek indicated no relevant financial relationships.
Owais Syed, MD1, Efan Jawad, MD1, Courtney Thomas, DO2, Eugenia Tsai, MD3, Lisa D. Pedicone, PhD3, Fabian Rodas, MD2, Carmen Landaverde, MD3, Andres Gomez-Aldana, MD2, Eric Lawitz, MD2, Fred Poordad, MD3, Jan Petrasek, MD, PhD3. P1801 - Liver Caught in the Storm: A Relapsing Case of HLH-Associated Severe Acute Liver Injury, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1UT Health Science Center San Antonio, San Antonio, TX; 2University of Texas Health San Antonio, San Antonio, TX; 3Texas Liver Institute, Austin, TX
Introduction: Hemophagocytic lymphohistiocytosis (HLH) is a rare and life-threatening hyperinflammatory syndrome characterized by uncontrolled cytokine release and multi-organ dysfunction. We present a challenging case of acute liver injury in a patient with relapsing HLH.
Case Description/
Methods: A 72-year-old female presented with fevers, jaundice and pancytopenia. Initial labs revealed AST 1361 U/L, ALT 587 U/L and total bilirubin (TB) 17.8 mg/dL and ALP 429 U/L. Ferritin was markedly elevated at 11,221 ng/mL. Imaging showed splenomegaly, and her soluble CD25 level was 35,000 U/mL. Liver biopsy demonstrated features consistent with HLH. She was treated with etoposide and dexamethasone with improvement of symptoms and normalization of liver enzymes. Four months later, she returned with arthralgias, myalgias and recurrent elevation of liver enzymes with AST 1554 U/L, ALT >3500 U/L and TB 5.9 mg/dL. Repeat liver biopsy demonstrated small clusters of histiocytes and portal/lobular changes consistent with HLH relapse (Figure 1, 2). She was retreated with etoposide, dexamethasone and cyclosporine with resolution of symptoms and biochemical improvement. Maintenance therapy was initiated with cyclosporine, dexamethasone and etoposide. However, one month later she presented with worsening liver tests (AST 1547 U/L, ALT 2316 U/L, TB 16 mg/dL), developed septic shock secondary from E. Coli bacteremia, and passed away during the hospitalization.
Discussion: Liver involvement in HLH is multifactorial, driven by cytokine-mediated injury, hemophagocytosis, and systemic inflammation. This case highlights the diagnostic and therapeutic complexities of HLH with liver involvement. The patient met six of the eight diagnostic criteria, including fever >38.5°C, splenomegaly, cytopenias in ≥2 cell lines, elevated ferritin, hypertriglyceridemia, and elevated soluble CD25. Liver biopsy revealed classic features of HLH, including histiocytic infiltrates and portal tract injury. Despite initial improvement with treatment, her subsequent relapses and eventual death emphasize the aggressive nature of HLH and the challenges of long-term management. This case underscores the importance of early recognition, prompt intervention, and continued investigation into effective maintenance strategies, particularly in older patients.
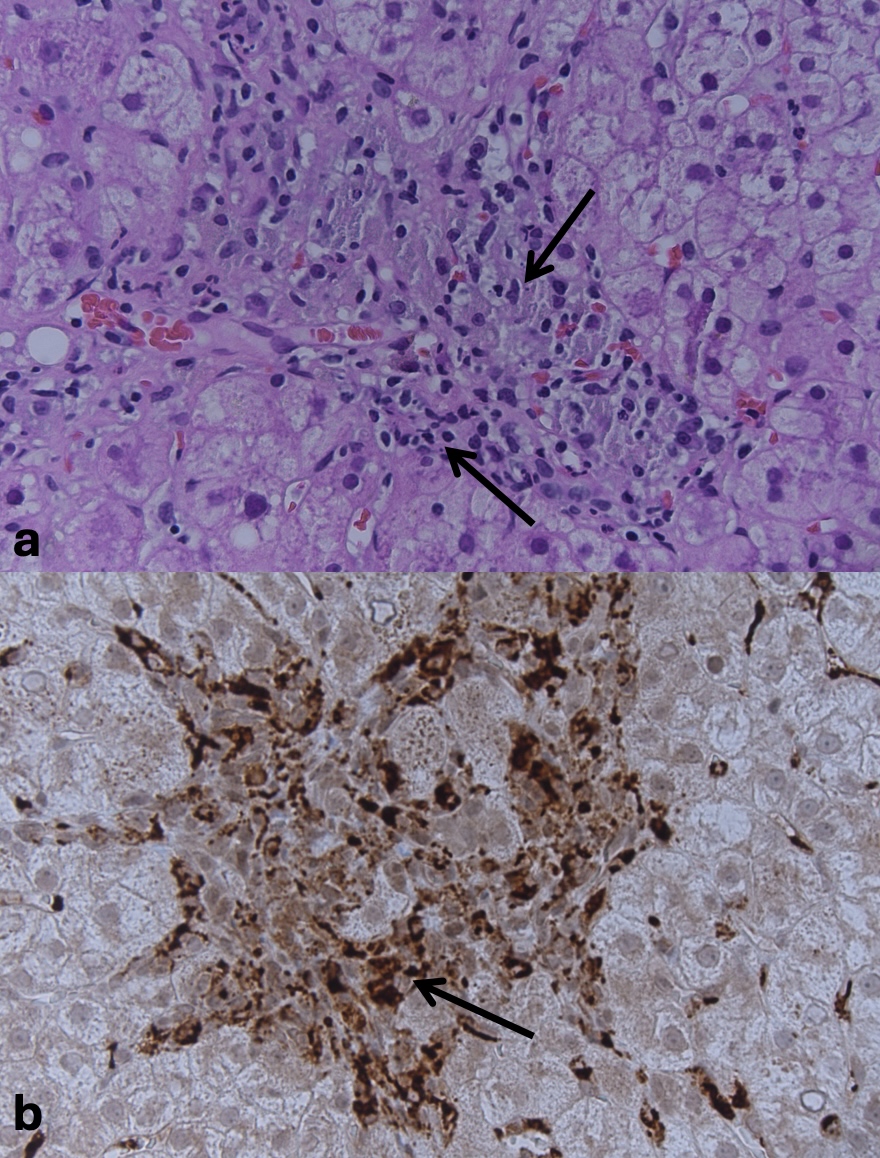
Figure: Liver biopsy demonstrated (a) Clusters of macrophages with two types of nuclei: smaller condensed lymphocyte nuclei and larger irregular macrophage nuclei on H&E stain (200X magnification) (b) CD68 stain highlights macrophages (200X magnification)
Disclosures:
Owais Syed indicated no relevant financial relationships.
Efan Jawad indicated no relevant financial relationships.
Courtney Thomas indicated no relevant financial relationships.
Eugenia Tsai indicated no relevant financial relationships.
Lisa D. Pedicone indicated no relevant financial relationships.
Fabian Rodas indicated no relevant financial relationships.
Carmen Landaverde indicated no relevant financial relationships.
Andres Gomez-Aldana indicated no relevant financial relationships.
Eric Lawitz indicated no relevant financial relationships.
Fred Poordad indicated no relevant financial relationships.
Jan Petrasek indicated no relevant financial relationships.
Owais Syed, MD1, Efan Jawad, MD1, Courtney Thomas, DO2, Eugenia Tsai, MD3, Lisa D. Pedicone, PhD3, Fabian Rodas, MD2, Carmen Landaverde, MD3, Andres Gomez-Aldana, MD2, Eric Lawitz, MD2, Fred Poordad, MD3, Jan Petrasek, MD, PhD3. P1801 - Liver Caught in the Storm: A Relapsing Case of HLH-Associated Severe Acute Liver Injury, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
