Sunday Poster Session
Category: Liver
P1796 - A Rare Cause of Acute Liver Failure: Diffuse Large B-Cell Lymphoma
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Rishika Trivedi, MD
DHR Health
McAllen, TX
Presenting Author(s)
Rishika Trivedi, MD1, Mahmoud Barbarawi, MD1, Laura Reyes-Uribe, MD1, Prince Shah-Riar, MD2, Henry Herrera, MD3, Asif Zamir, MD, FACG4
1DHR Health, McAllen, TX; 2DHR Health, Edinburg, Tx, McAllen, TX; 3DHR Health Gastroenterology, McAllen, TX; 4DHR Health Gastroenterology, Edinburg, TX
Introduction: Fulminant hepatic failure is a life-threatening syndrome most often caused by viral hepatitis, drug-induced liver injury, or autoimmune hepatitis. Rarely, infiltrative malignancies such as lymphoma can present with acute liver failure, often with subtle or absent radiologic findings. Diffuse large B-cell lymphoma (DLBCL) involving the liver is uncommon, and its diagnosis is frequently delayed due to nonspecific symptoms and negative imaging. Early liver biopsy is crucial for accurate diagnosis and effective management.
Case Description/
Methods:
A 76-year-old man with stage III colon cancer in remission, parkinson's disease (with cerebral neurostimulator), presented with three weeks of fatigue, night sweats, and low-grade fevers. On admission, he was jaundiced, confused, and clinically frail. Labs revealed AST 206, ALT 102, ALP 330, Total bilirubin 20.3 (direct 18.2), albumin 2.3, and ferritin >6000 ng/ml.
Abdominal CT with contrast showed hepatosplenomegaly without biliary obstruction (figure 1). MRCP was contraindicated due to the neurostimulator. The patient developed contrast-induced acute kidney injury shortly after. Autoimmune and infectious workup was negative. Gradually, he developed INR of 1.65, and worsening confusion meeting criteria for liver failure. Given the diagnostic uncertainty, an infiltrative process was suspected. The platelets decreased to 30,000, a transfusion was performed and a liver biopsy was scheduled. The biopsy revealed diffuse sinusoidal infiltration by atypical lymphocytes without steatosis and fibrosis. Concurrent peripheral smear showed atypical lymphocytes, nucleated RBC, and leukoerythroblastic reaction. Bone marrow biopsy confirmed DLBCL with 90-100% infiltration. t(14;18) IGH::BCL2 and a complex karyotype were identified. The patient progressed to metabolic acidosis and hypoxemic respiratory failure.He was deemed not a candidate for liver transplantation due to age and clinical status. Due to multi-organ failure and poor prognosis, the family opted for comfort measures.
Discussion: This case highlights DLBCL as a rare cause of fulminant hepatic failure. Imaging was non-diagnostic and diagnosis depended on liver biopsy, which revealed the classic lymphomatous infiltration. DLBCL should be considered as a cause of liver failure when common etiologies have been excluded, especially in patients with systemic symptoms. Early biopsy is necessary when imaging is inconclusive, as rapid progression may preclude timely diagnosis and treatment.
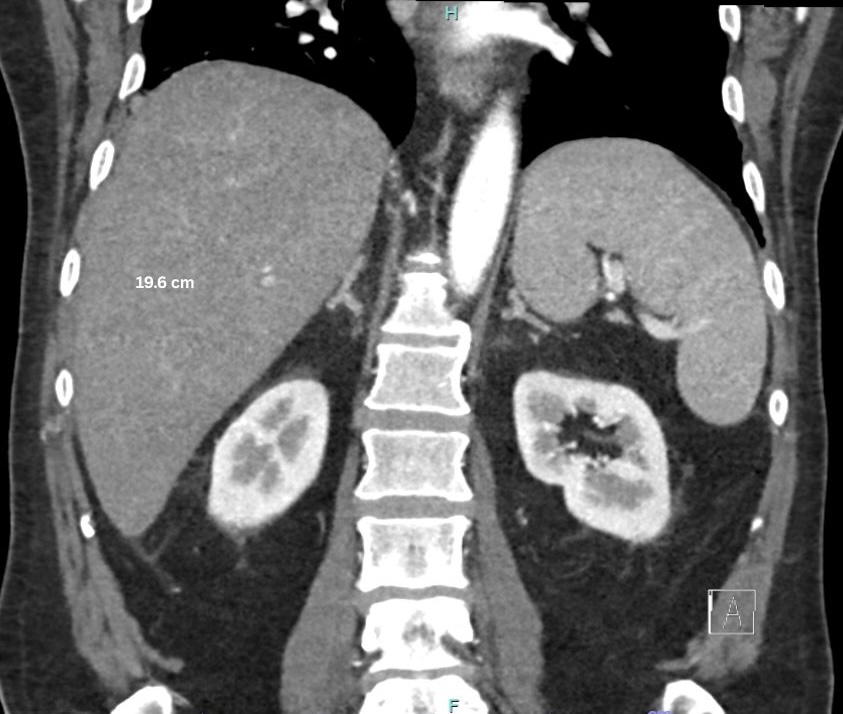
Figure: CT abdomen showed hepatomegaly with increased echotexture of the liver parenchyma, consistent with hepatic steatosis versus nonspecific hepatocellular disease. No intrahepatic bile duct dilation was seen at this time (Figure 1)
Disclosures:
Rishika Trivedi indicated no relevant financial relationships.
Mahmoud Barbarawi indicated no relevant financial relationships.
Laura Reyes-Uribe indicated no relevant financial relationships.
Prince Shah-Riar indicated no relevant financial relationships.
Henry Herrera indicated no relevant financial relationships.
Asif Zamir indicated no relevant financial relationships.
Rishika Trivedi, MD1, Mahmoud Barbarawi, MD1, Laura Reyes-Uribe, MD1, Prince Shah-Riar, MD2, Henry Herrera, MD3, Asif Zamir, MD, FACG4. P1796 - A Rare Cause of Acute Liver Failure: Diffuse Large B-Cell Lymphoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1DHR Health, McAllen, TX; 2DHR Health, Edinburg, Tx, McAllen, TX; 3DHR Health Gastroenterology, McAllen, TX; 4DHR Health Gastroenterology, Edinburg, TX
Introduction: Fulminant hepatic failure is a life-threatening syndrome most often caused by viral hepatitis, drug-induced liver injury, or autoimmune hepatitis. Rarely, infiltrative malignancies such as lymphoma can present with acute liver failure, often with subtle or absent radiologic findings. Diffuse large B-cell lymphoma (DLBCL) involving the liver is uncommon, and its diagnosis is frequently delayed due to nonspecific symptoms and negative imaging. Early liver biopsy is crucial for accurate diagnosis and effective management.
Case Description/
Methods:
A 76-year-old man with stage III colon cancer in remission, parkinson's disease (with cerebral neurostimulator), presented with three weeks of fatigue, night sweats, and low-grade fevers. On admission, he was jaundiced, confused, and clinically frail. Labs revealed AST 206, ALT 102, ALP 330, Total bilirubin 20.3 (direct 18.2), albumin 2.3, and ferritin >6000 ng/ml.
Abdominal CT with contrast showed hepatosplenomegaly without biliary obstruction (figure 1). MRCP was contraindicated due to the neurostimulator. The patient developed contrast-induced acute kidney injury shortly after. Autoimmune and infectious workup was negative. Gradually, he developed INR of 1.65, and worsening confusion meeting criteria for liver failure. Given the diagnostic uncertainty, an infiltrative process was suspected. The platelets decreased to 30,000, a transfusion was performed and a liver biopsy was scheduled. The biopsy revealed diffuse sinusoidal infiltration by atypical lymphocytes without steatosis and fibrosis. Concurrent peripheral smear showed atypical lymphocytes, nucleated RBC, and leukoerythroblastic reaction. Bone marrow biopsy confirmed DLBCL with 90-100% infiltration. t(14;18) IGH::BCL2 and a complex karyotype were identified. The patient progressed to metabolic acidosis and hypoxemic respiratory failure.He was deemed not a candidate for liver transplantation due to age and clinical status. Due to multi-organ failure and poor prognosis, the family opted for comfort measures.
Discussion: This case highlights DLBCL as a rare cause of fulminant hepatic failure. Imaging was non-diagnostic and diagnosis depended on liver biopsy, which revealed the classic lymphomatous infiltration. DLBCL should be considered as a cause of liver failure when common etiologies have been excluded, especially in patients with systemic symptoms. Early biopsy is necessary when imaging is inconclusive, as rapid progression may preclude timely diagnosis and treatment.
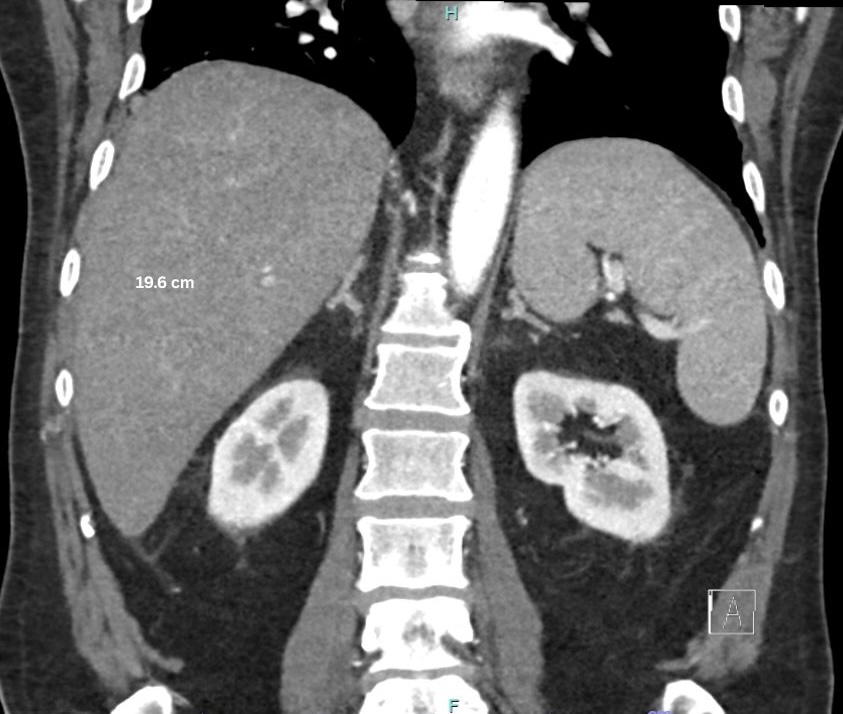
Figure: CT abdomen showed hepatomegaly with increased echotexture of the liver parenchyma, consistent with hepatic steatosis versus nonspecific hepatocellular disease. No intrahepatic bile duct dilation was seen at this time (Figure 1)
Disclosures:
Rishika Trivedi indicated no relevant financial relationships.
Mahmoud Barbarawi indicated no relevant financial relationships.
Laura Reyes-Uribe indicated no relevant financial relationships.
Prince Shah-Riar indicated no relevant financial relationships.
Henry Herrera indicated no relevant financial relationships.
Asif Zamir indicated no relevant financial relationships.
Rishika Trivedi, MD1, Mahmoud Barbarawi, MD1, Laura Reyes-Uribe, MD1, Prince Shah-Riar, MD2, Henry Herrera, MD3, Asif Zamir, MD, FACG4. P1796 - A Rare Cause of Acute Liver Failure: Diffuse Large B-Cell Lymphoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
