Sunday Poster Session
Category: Liver
P1772 - Tripping Over Trypsin: How Coexistent Inflammatory States Can Trip up Healthcare Providers in the Diagnosis of Alpha-1 Antitrypsin Deficiency
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Alarica Dietzen, MD, MPH
Emory University School of Medicine
Atlanta, GA
Presenting Author(s)
Alarica Dietzen, MD, MPH1, Felix Saladin, MD1, Jigna C. Jani, MD2, Thuy-Van Hang, MD1
1Emory University School of Medicine, Atlanta, GA; 2Joseph Maxwell Cleland Atlanta Veteran Affairs Medical Center, Decatur, GA
Introduction: Alpha-1 antitrypsin deficiency (AATD) is an autosomal, codominant disorder characterized by decreased functionality of alpha-1 antitrypsin (AAT), a protein that inhibits human neutrophil elastase. AATD is typically associated with Pi*ZZ homozygotes but also occurs in Pi*MZ and the Pi*SZ heterozygotes, affecting both lung and liver function.
Case Description/
Methods: A 48-year-old man living with controlled HIV, chronic hepatitis B, and chronic cholestasis thought to be from antiretrovirals, presented with one month of recurrent right upper quadrant (RUQ) pain, fatigue, nausea, and vomiting. Initial evaluation was remarkable for scleral icterus and RUQ tenderness, as well as total bilirubin (Tbili) 7.7 mg/dL (from baseline 4.2 mg/dL), ALP 403 U/L, AST 201 U/L, and ALT 142 U/L. MRI Abdomen confirmed liver cirrhosis without biliary ductal dilatation, masses, or venous occlusions. By day four, his symptoms improved. Tbili peaked at 10.9 mg/dL. He was discharged with plans for outpatient liver biopsy. He returned five days later with worsening RUQ pain, myalgias, chills, night sweats, dyspnea, and a Tbili of 13.1 mg/dL. A liver biopsy was performed, and he was discharged once Tbili stabilized at 11.9 mg/dL. Pathology revealed cholestatic hepatitis, stage III/IV fibrosis, chronic portal inflammation, and scattered Periodic Acid-Schiff (PAS)-positive globules. Stains for Epstein-Barr virus, cytomegalovirus, and herpes simplex viruses were negative. Autoimmune workup was negative. AAT level was mildly elevated to 216 mg/dL, decreasing initial concern for AATD. Drug-induced liver injury was favored, but due to PAS+ globules, AAT genotyping was ordered and revealed a Pi*MZ genotype. Over the next five months, the patient’s Tbili rose to 26.3. He ultimately was felt to have cirrhosis and severe cholestatic injury due to his AAT PI*MZ phenotype compounded by chronic HIV and HBV, despite viral suppression. Six months later, he received a liver transplant. His explant demonstrated an incidental < 1 cm hepatocellular carcinoma.
Discussion: AAT is an acute phase reactant that can be elevated, even in the setting of AATD. In patients with progressively worsening liver injury and proinflammatory states, AATD should remain on the differential despite an elevated AAT level, and genotyping should be pursued. Heterozygous Pi*MZ patients may be at increased risk for chronic liver disease progression if they have comorbid conditions, such as chronic viral infections. Generative AI was used to condense this abstract.
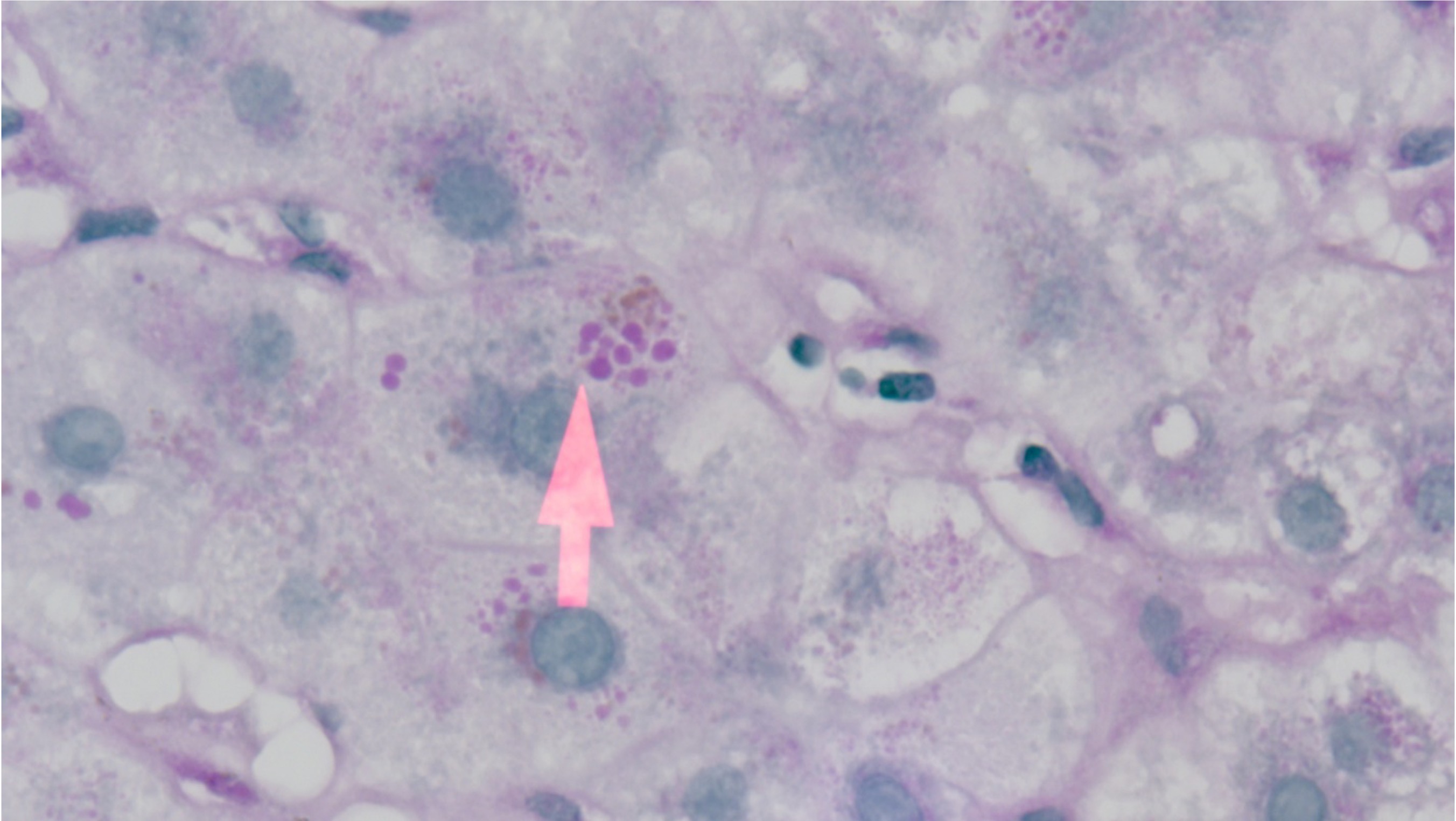
Figure: Alpha-1 antitrypsin globules within the cytoplasm of a hepatocyte that has stained positive (magenta) using Periodic acid Shiff-Diastase (PAS-D) stain.
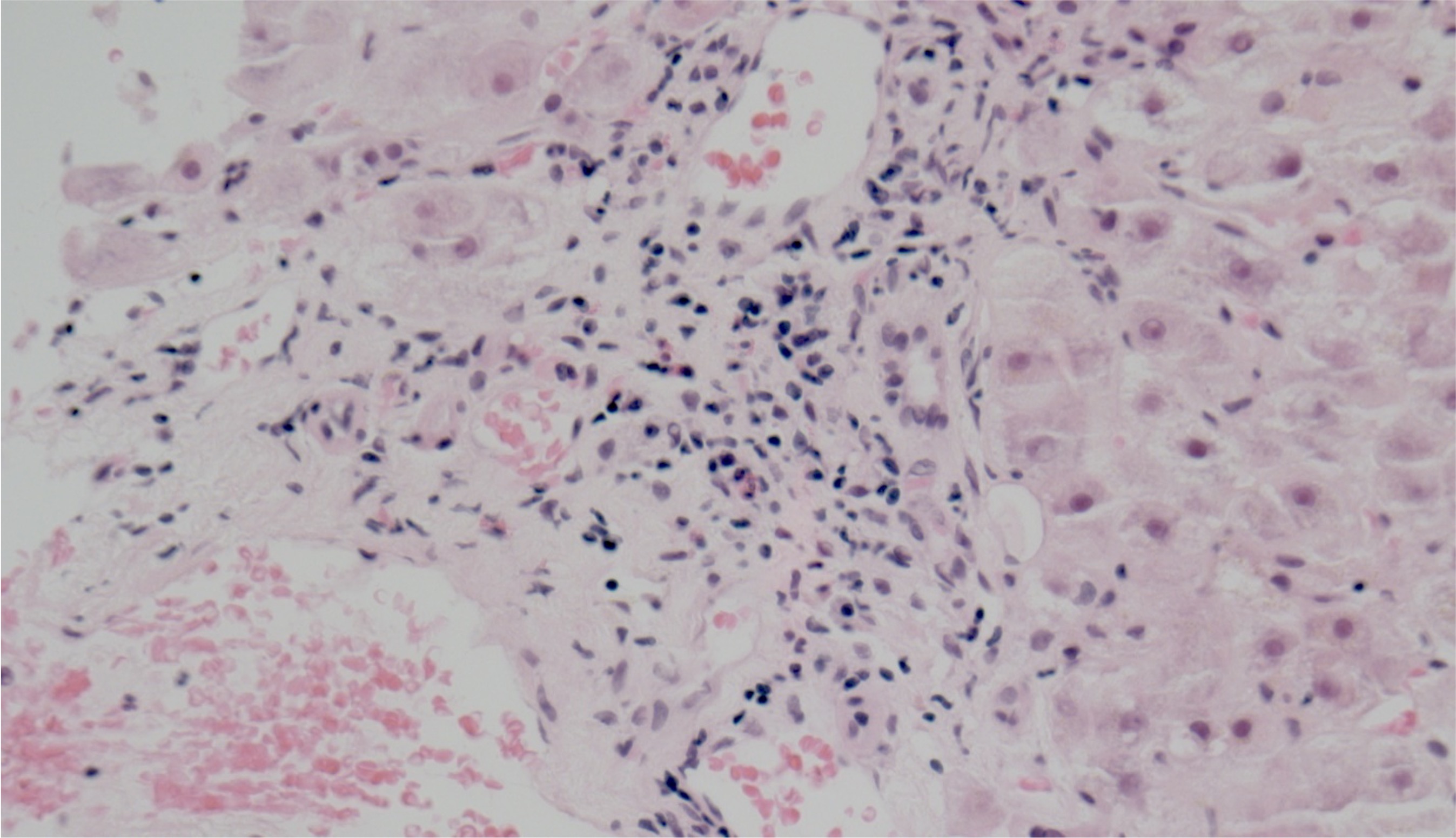
Figure: H&E stain of portal tract inflammation at 20x magnification.
Disclosures:
Alarica Dietzen indicated no relevant financial relationships.
Felix Saladin indicated no relevant financial relationships.
Jigna Jani indicated no relevant financial relationships.
Thuy-Van Hang indicated no relevant financial relationships.
Alarica Dietzen, MD, MPH1, Felix Saladin, MD1, Jigna C. Jani, MD2, Thuy-Van Hang, MD1. P1772 - Tripping Over Trypsin: How Coexistent Inflammatory States Can Trip up Healthcare Providers in the Diagnosis of Alpha-1 Antitrypsin Deficiency, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Emory University School of Medicine, Atlanta, GA; 2Joseph Maxwell Cleland Atlanta Veteran Affairs Medical Center, Decatur, GA
Introduction: Alpha-1 antitrypsin deficiency (AATD) is an autosomal, codominant disorder characterized by decreased functionality of alpha-1 antitrypsin (AAT), a protein that inhibits human neutrophil elastase. AATD is typically associated with Pi*ZZ homozygotes but also occurs in Pi*MZ and the Pi*SZ heterozygotes, affecting both lung and liver function.
Case Description/
Methods: A 48-year-old man living with controlled HIV, chronic hepatitis B, and chronic cholestasis thought to be from antiretrovirals, presented with one month of recurrent right upper quadrant (RUQ) pain, fatigue, nausea, and vomiting. Initial evaluation was remarkable for scleral icterus and RUQ tenderness, as well as total bilirubin (Tbili) 7.7 mg/dL (from baseline 4.2 mg/dL), ALP 403 U/L, AST 201 U/L, and ALT 142 U/L. MRI Abdomen confirmed liver cirrhosis without biliary ductal dilatation, masses, or venous occlusions. By day four, his symptoms improved. Tbili peaked at 10.9 mg/dL. He was discharged with plans for outpatient liver biopsy. He returned five days later with worsening RUQ pain, myalgias, chills, night sweats, dyspnea, and a Tbili of 13.1 mg/dL. A liver biopsy was performed, and he was discharged once Tbili stabilized at 11.9 mg/dL. Pathology revealed cholestatic hepatitis, stage III/IV fibrosis, chronic portal inflammation, and scattered Periodic Acid-Schiff (PAS)-positive globules. Stains for Epstein-Barr virus, cytomegalovirus, and herpes simplex viruses were negative. Autoimmune workup was negative. AAT level was mildly elevated to 216 mg/dL, decreasing initial concern for AATD. Drug-induced liver injury was favored, but due to PAS+ globules, AAT genotyping was ordered and revealed a Pi*MZ genotype. Over the next five months, the patient’s Tbili rose to 26.3. He ultimately was felt to have cirrhosis and severe cholestatic injury due to his AAT PI*MZ phenotype compounded by chronic HIV and HBV, despite viral suppression. Six months later, he received a liver transplant. His explant demonstrated an incidental < 1 cm hepatocellular carcinoma.
Discussion: AAT is an acute phase reactant that can be elevated, even in the setting of AATD. In patients with progressively worsening liver injury and proinflammatory states, AATD should remain on the differential despite an elevated AAT level, and genotyping should be pursued. Heterozygous Pi*MZ patients may be at increased risk for chronic liver disease progression if they have comorbid conditions, such as chronic viral infections. Generative AI was used to condense this abstract.
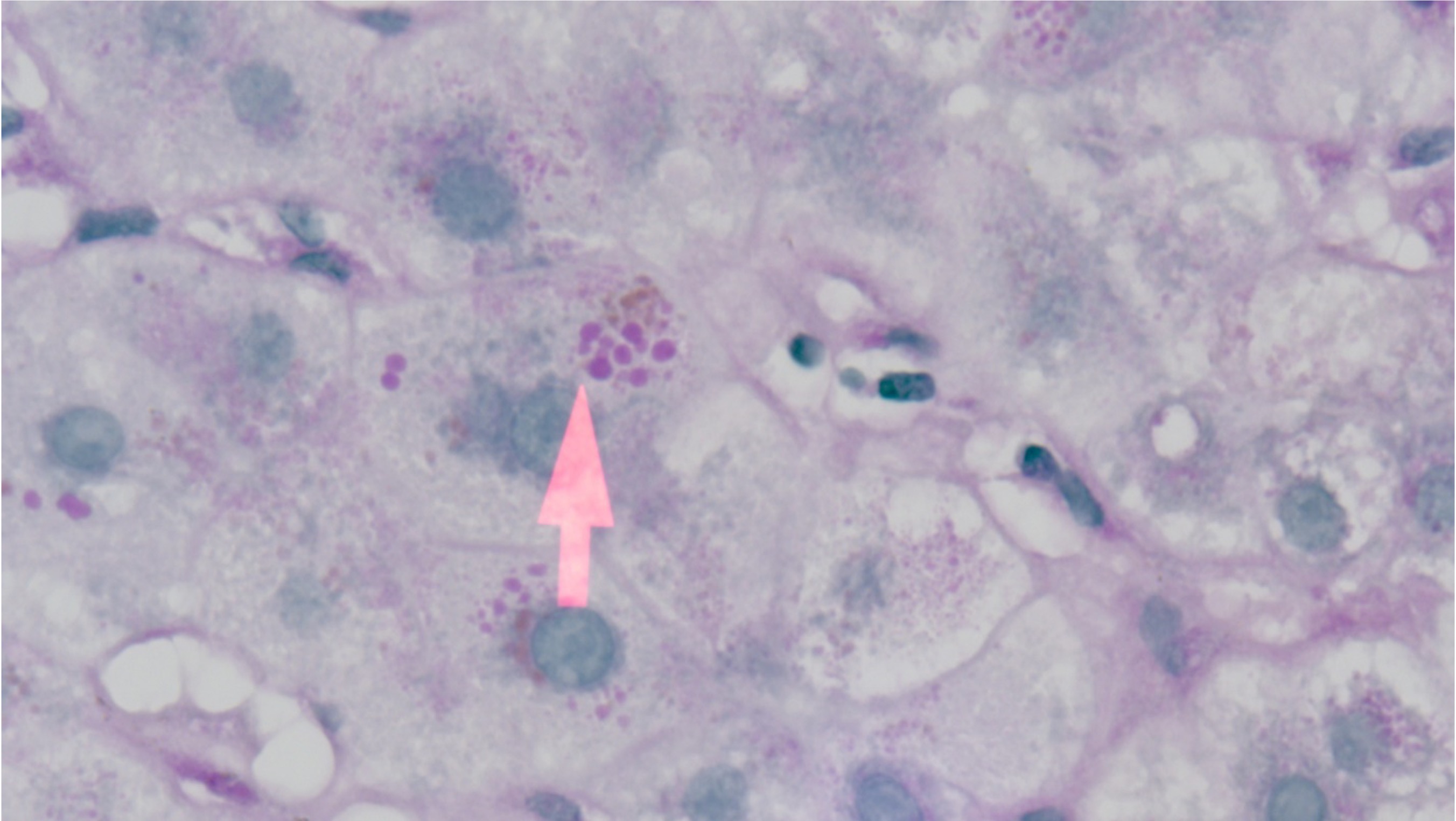
Figure: Alpha-1 antitrypsin globules within the cytoplasm of a hepatocyte that has stained positive (magenta) using Periodic acid Shiff-Diastase (PAS-D) stain.
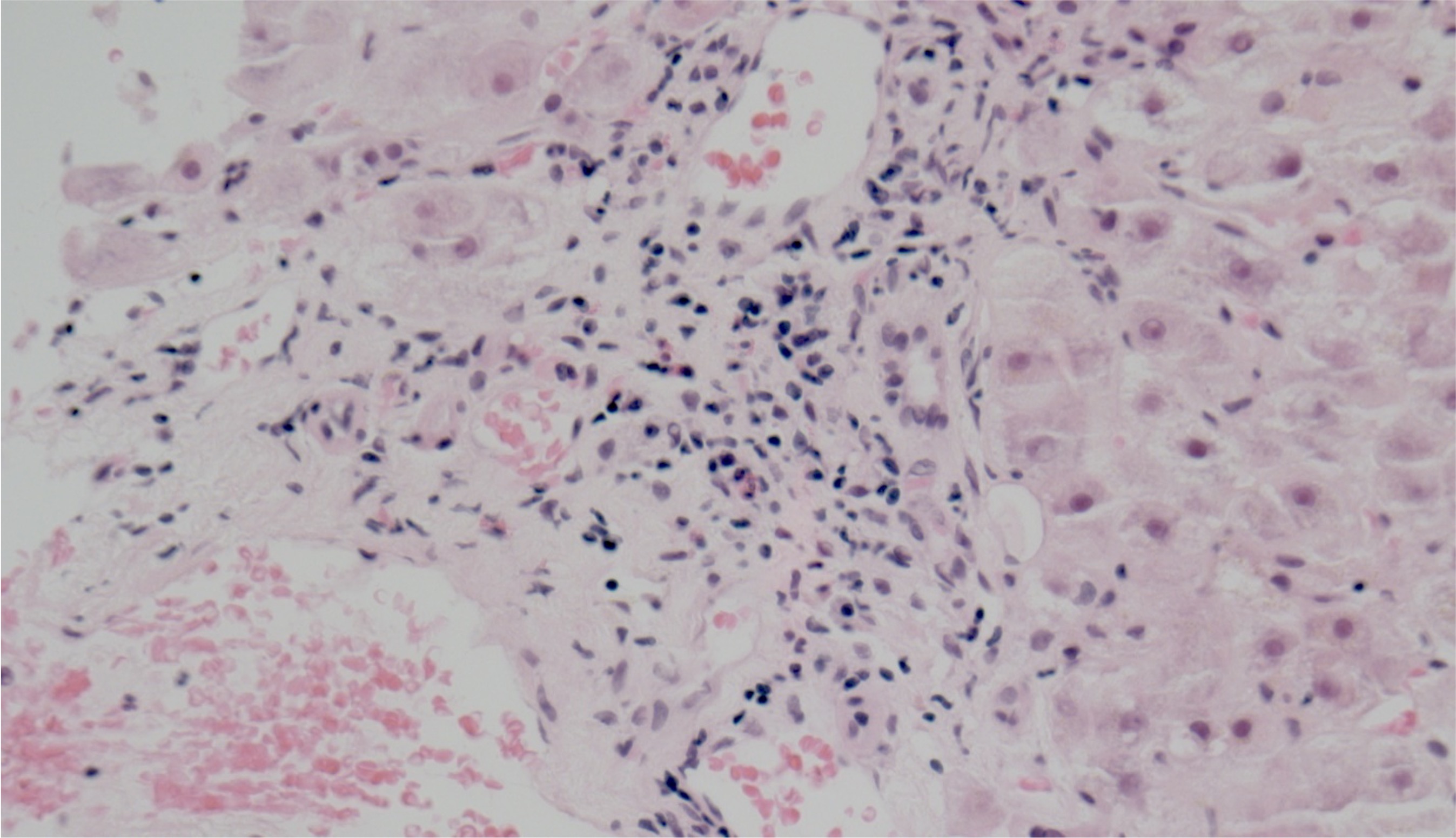
Figure: H&E stain of portal tract inflammation at 20x magnification.
Disclosures:
Alarica Dietzen indicated no relevant financial relationships.
Felix Saladin indicated no relevant financial relationships.
Jigna Jani indicated no relevant financial relationships.
Thuy-Van Hang indicated no relevant financial relationships.
Alarica Dietzen, MD, MPH1, Felix Saladin, MD1, Jigna C. Jani, MD2, Thuy-Van Hang, MD1. P1772 - Tripping Over Trypsin: How Coexistent Inflammatory States Can Trip up Healthcare Providers in the Diagnosis of Alpha-1 Antitrypsin Deficiency, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
