Sunday Poster Session
Category: Liver
P1769 - When Noninvasive Tests Clash: Magnetic Resonance Elastography (MRE) as the Tie-breaker in Liver Fibrosis Staging
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Theja V. Channapragada, DO, MBA, MS (he/him/his)
Penn State Health Milton S. Hershey Medical Center
Hershey, PA
Presenting Author(s)
Theja V. Channapragada, DO, MBA, MS1, Vishal Patel, MD2, Srinivas Channapragada, MD3
1Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 2St. Luke's University Health Network, Merion Station, PA; 3Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ
Introduction: Metabolic-Dysfunction Associated Steatotic Liver Disease (MASLD) is characterized by hepatic steatosis in the presence of cardiometabolic risk factors and affects approximately 25% of the global population. MASLD can progress into metabolic dysfunction-associated steatohepatitis (MASH) and cirrhosis, with the fibrosis stage as the strongest predictor of liver-related outcomes. While noninvasive tests (NITs) like Fibrosis-4, Enhanced Liver Fibrosis (ELF) Score, Fibrosure, Vibration-Controlled Transient Elastography, and Ultrasound Elastography are widely used to assess fibrosis and potentially replace liver biopsy, significant discordance often exists between these tests. Each test also has unique therapeutic thresholds, further complicating management. MR elastography (MRE) is widely considered one of the most reliable and accurate noninvasive methods for evaluating liver fibrosis. The sensitivity and specificity of Magnetic Resonance Elastography (MRE) in differentiating significant fibrosis (≥F2) from F0 to F1 stages are in the range of 79–94% and 86–97% respectively. We present a community-based case series where MRE resolved discordant NIT results and guided management.
Case Description/
Methods: Three patients with MASLD at a community gastroenterology-hepatology clinic underwent evaluation with standard NITs and MRE. All tests were done within a one-year time frame. Initially, all 3 patients were considered candidates for Resmetirom, recently FDA-approved for treatment of non-cirrhotic MASH with significant fibrosis, based on at least one NIT showing Stage 2 to 3 fibrosis. MRE ruled out advanced fibrosis and spared all 3 patients from undergoing biopsy or initiation of resmetirom. All patients were consulted on lifestyle management, specifically exercise and dieting. See Table 1.
Discussion: MRE reclassified fibrosis staging in all three patients with discordant NITs, helping avoid liver biopsy, guiding accurate risk stratification, and reducing unnecessary initiation of long-term pharmacological therapy. Recent studies have shown that MRE outperforms FIB-4 and VCTE (AUC 0.85 vs. 0.66 and 0.63), and current AASLD and AGA guidelines recommend MRE when NITs are inconclusive. Our case series emphasizes the role of MRE as an important tool in MASLD/MASH management bridging the gap between guideline recommendations and real-world practice in the community setting.
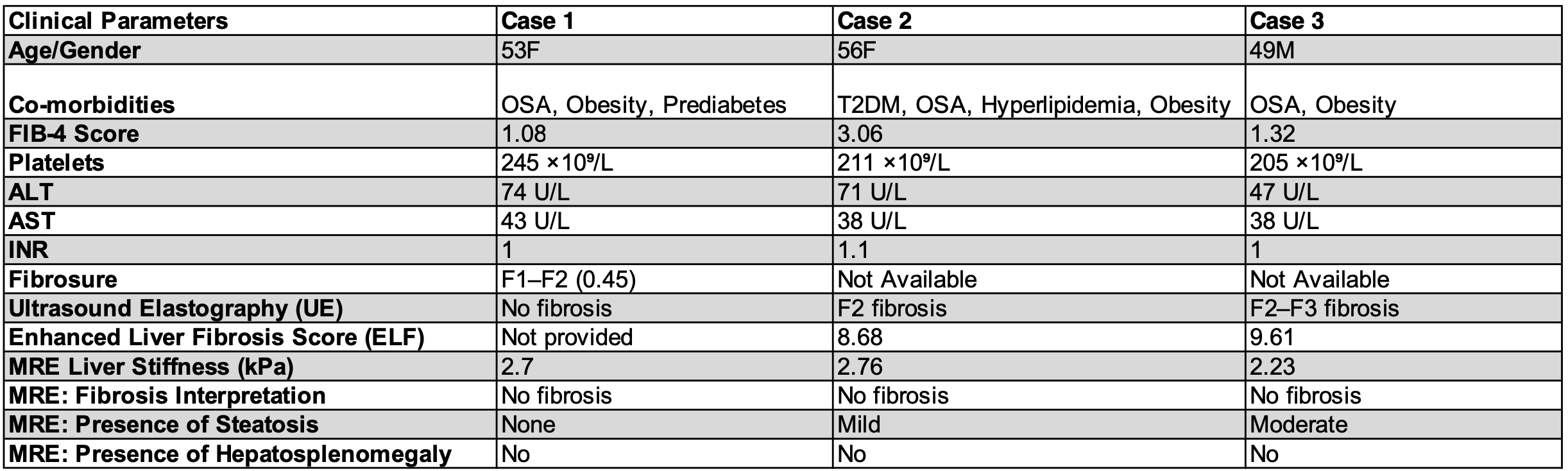
Figure: Table 1: Summary of Clinical Parameters and Noninvasive tests (NITs) in Three MASLD Patients with Discordant Test Results Resolved by MR Elastography
Disclosures:
Theja Channapragada indicated no relevant financial relationships.
Vishal Patel indicated no relevant financial relationships.
Srinivas Channapragada indicated no relevant financial relationships.
Theja V. Channapragada, DO, MBA, MS1, Vishal Patel, MD2, Srinivas Channapragada, MD3. P1769 - When Noninvasive Tests Clash: Magnetic Resonance Elastography (MRE) as the Tie-breaker in Liver Fibrosis Staging, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 2St. Luke's University Health Network, Merion Station, PA; 3Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ
Introduction: Metabolic-Dysfunction Associated Steatotic Liver Disease (MASLD) is characterized by hepatic steatosis in the presence of cardiometabolic risk factors and affects approximately 25% of the global population. MASLD can progress into metabolic dysfunction-associated steatohepatitis (MASH) and cirrhosis, with the fibrosis stage as the strongest predictor of liver-related outcomes. While noninvasive tests (NITs) like Fibrosis-4, Enhanced Liver Fibrosis (ELF) Score, Fibrosure, Vibration-Controlled Transient Elastography, and Ultrasound Elastography are widely used to assess fibrosis and potentially replace liver biopsy, significant discordance often exists between these tests. Each test also has unique therapeutic thresholds, further complicating management. MR elastography (MRE) is widely considered one of the most reliable and accurate noninvasive methods for evaluating liver fibrosis. The sensitivity and specificity of Magnetic Resonance Elastography (MRE) in differentiating significant fibrosis (≥F2) from F0 to F1 stages are in the range of 79–94% and 86–97% respectively. We present a community-based case series where MRE resolved discordant NIT results and guided management.
Case Description/
Methods: Three patients with MASLD at a community gastroenterology-hepatology clinic underwent evaluation with standard NITs and MRE. All tests were done within a one-year time frame. Initially, all 3 patients were considered candidates for Resmetirom, recently FDA-approved for treatment of non-cirrhotic MASH with significant fibrosis, based on at least one NIT showing Stage 2 to 3 fibrosis. MRE ruled out advanced fibrosis and spared all 3 patients from undergoing biopsy or initiation of resmetirom. All patients were consulted on lifestyle management, specifically exercise and dieting. See Table 1.
Discussion: MRE reclassified fibrosis staging in all three patients with discordant NITs, helping avoid liver biopsy, guiding accurate risk stratification, and reducing unnecessary initiation of long-term pharmacological therapy. Recent studies have shown that MRE outperforms FIB-4 and VCTE (AUC 0.85 vs. 0.66 and 0.63), and current AASLD and AGA guidelines recommend MRE when NITs are inconclusive. Our case series emphasizes the role of MRE as an important tool in MASLD/MASH management bridging the gap between guideline recommendations and real-world practice in the community setting.
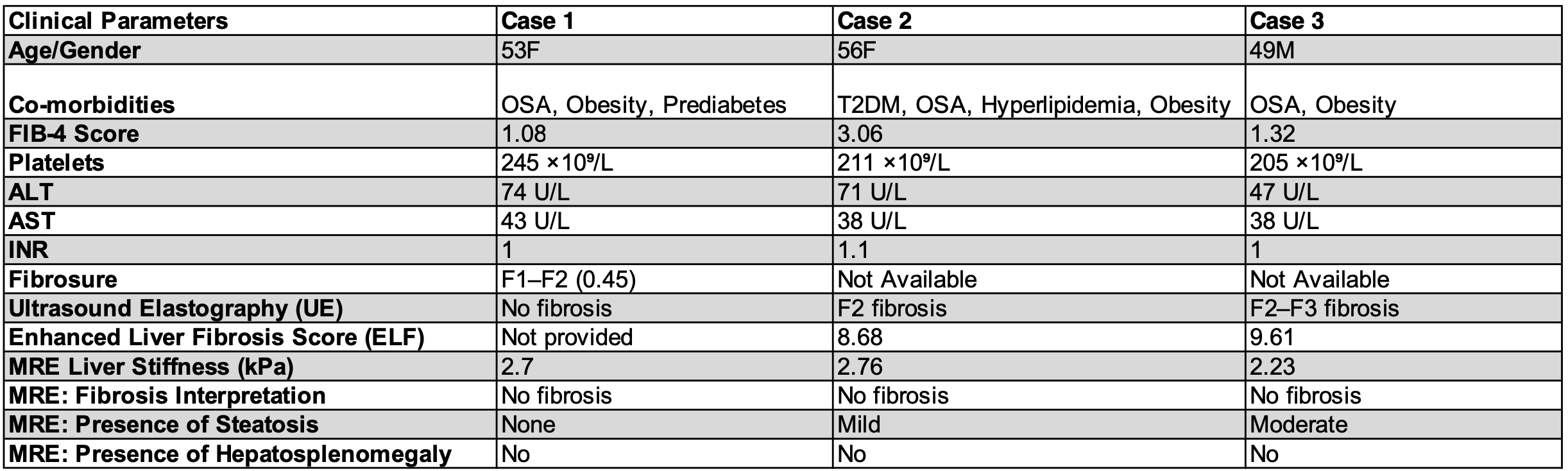
Figure: Table 1: Summary of Clinical Parameters and Noninvasive tests (NITs) in Three MASLD Patients with Discordant Test Results Resolved by MR Elastography
Disclosures:
Theja Channapragada indicated no relevant financial relationships.
Vishal Patel indicated no relevant financial relationships.
Srinivas Channapragada indicated no relevant financial relationships.
Theja V. Channapragada, DO, MBA, MS1, Vishal Patel, MD2, Srinivas Channapragada, MD3. P1769 - When Noninvasive Tests Clash: Magnetic Resonance Elastography (MRE) as the Tie-breaker in Liver Fibrosis Staging, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
