Sunday Poster Session
Category: Liver
P1752 - Treponema Tricks the Liver: A Case of Reversible Cholangiopathy in Disguise
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- LG
Leslie Graus, PA-C (she/her/hers)
University of Rochester Medical Center
Rochester, NY
Presenting Author(s)
Award: ACG Presidential Poster Award
Leslie Graus, PA-C, Monica Patel, MD, Charlotte Ryan, MD, Sarah McPherson, NP, Sarah Enslin, PA, Vivek Kaul, MD, FACG, Patrick Twohig, MD, MPH
University of Rochester Medical Center, Rochester, NY
Introduction: Syphilis, a sexually transmitted infection (STI) caused by Treponema pallidum, is known for its diverse and deceptive clinical manifestations. Often presenting with cutaneous symptoms, hepatic involvement-or syphilitic hepatitis (SH)-is rare and underrecognized. SH may present with elevated liver enzymes (LFTs) and imaging suggesting biliary obstruction, mimicking other hepatobiliary diseases. We report a case of SH with complete resolution of both biochemical and radiologic abnormalities following penicillin G therapy, highlighting the reversibility of SH when promptly diagnosed and treated.
Case Description/
Methods: A 28-year-old male with a history of injection drug use and high-risk sexual behavior presented to the hospital with one-week of pruritus, dark urine, nausea, vomiting, and epigastric pain. Lab workup showed AST 72 U/L, ALT 194 U/L, alkaline phosphatase 577 U/L, total bilirubin 3 mg/dL, and direct bilirubin 2.2 mg/dL. Antimitochondrial antibody was positive, and both total IgG and IgG4 levels were elevated. MR abdomen showed a possible common hepatic duct stricture. Due to improved LFTs and overall clinical status, he was discharged on ursodiol. At his follow-up hepatology appointment 2 weeks later, he had new flat, erythematous lesions on his palms and soles. Syphilis testing was positive. Subsequent liver biopsy revealed intra-canalicular and hepatocellular cholestasis with mild bile duct proliferation, a lymphocytic portal infiltrate, and negative stains for T. pallidum (Figure 1). He was treated with Penicillin G with normalization in his LFTs. Follow-up MRCP showed resolution of the previously suspected biliary stricture.
Discussion: Our patient’s abnormal LFTs and imaging suggesting biliary stricture are more commonly seen in other hepatobiliary diseases. Current literature suggests that SH can be diagnosed based on a cholestatic pattern of LFT elevation, serologic confirmation of syphilis, exclusion of other causes, and normalization of LFTs after antimicrobial therapy. A rash on the palms and soles, as seen in our patient, is also a hallmark feature of secondary syphilis and a valuable diagnostic clue. This case reinforces the importance of considering syphilis in the differential diagnosis of unexplained liver enzyme elevations and bile duct abnormalities, particularly in patients with risk factors for STIs. Early recognition and treatment can prevent unnecessary interventions and lead to complete resolution of hepatic dysfunction.
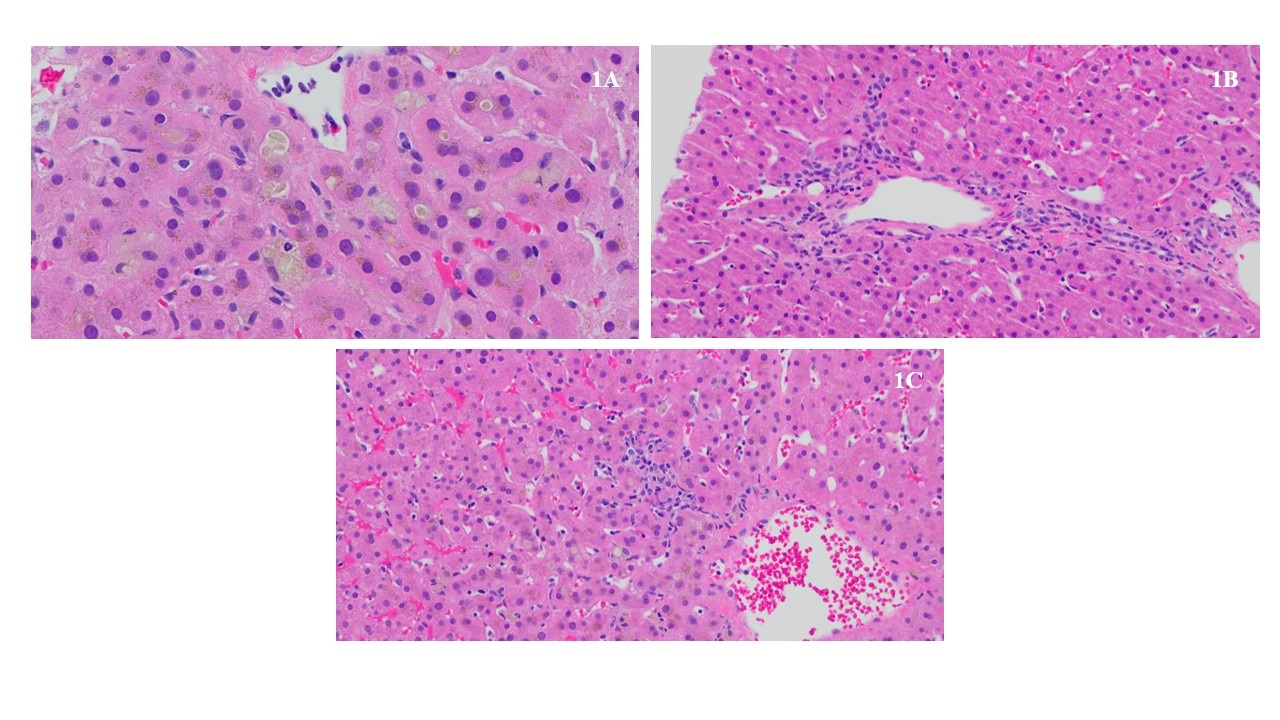
Figure: Figure 1A: High power of lobule with canalicular and hepatocellular cholestasis around a central vein.
Figure 1B: Portal tract with bile ductular proliferation and scant inflammation.
Figure 1C: Focus of lobular lymphocytic inflammation in zone 3 (centrilobular).
Disclosures:
Leslie Graus indicated no relevant financial relationships.
Monica Patel indicated no relevant financial relationships.
Charlotte Ryan indicated no relevant financial relationships.
Sarah McPherson indicated no relevant financial relationships.
Sarah Enslin: AbbVie – Consultant. Ardelyx – Consultant. Castle Biosciences – Consultant. Exact Sciences – Consultant. Ironwood Pharmaceuticals – Consultant. Johnson & Johnson – Consultant. NovoNordisk – Consultant.
Vivek Kaul indicated no relevant financial relationships.
Patrick Twohig indicated no relevant financial relationships.
Leslie Graus, PA-C, Monica Patel, MD, Charlotte Ryan, MD, Sarah McPherson, NP, Sarah Enslin, PA, Vivek Kaul, MD, FACG, Patrick Twohig, MD, MPH. P1752 - Treponema Tricks the Liver: A Case of Reversible Cholangiopathy in Disguise, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Leslie Graus, PA-C, Monica Patel, MD, Charlotte Ryan, MD, Sarah McPherson, NP, Sarah Enslin, PA, Vivek Kaul, MD, FACG, Patrick Twohig, MD, MPH
University of Rochester Medical Center, Rochester, NY
Introduction: Syphilis, a sexually transmitted infection (STI) caused by Treponema pallidum, is known for its diverse and deceptive clinical manifestations. Often presenting with cutaneous symptoms, hepatic involvement-or syphilitic hepatitis (SH)-is rare and underrecognized. SH may present with elevated liver enzymes (LFTs) and imaging suggesting biliary obstruction, mimicking other hepatobiliary diseases. We report a case of SH with complete resolution of both biochemical and radiologic abnormalities following penicillin G therapy, highlighting the reversibility of SH when promptly diagnosed and treated.
Case Description/
Methods: A 28-year-old male with a history of injection drug use and high-risk sexual behavior presented to the hospital with one-week of pruritus, dark urine, nausea, vomiting, and epigastric pain. Lab workup showed AST 72 U/L, ALT 194 U/L, alkaline phosphatase 577 U/L, total bilirubin 3 mg/dL, and direct bilirubin 2.2 mg/dL. Antimitochondrial antibody was positive, and both total IgG and IgG4 levels were elevated. MR abdomen showed a possible common hepatic duct stricture. Due to improved LFTs and overall clinical status, he was discharged on ursodiol. At his follow-up hepatology appointment 2 weeks later, he had new flat, erythematous lesions on his palms and soles. Syphilis testing was positive. Subsequent liver biopsy revealed intra-canalicular and hepatocellular cholestasis with mild bile duct proliferation, a lymphocytic portal infiltrate, and negative stains for T. pallidum (Figure 1). He was treated with Penicillin G with normalization in his LFTs. Follow-up MRCP showed resolution of the previously suspected biliary stricture.
Discussion: Our patient’s abnormal LFTs and imaging suggesting biliary stricture are more commonly seen in other hepatobiliary diseases. Current literature suggests that SH can be diagnosed based on a cholestatic pattern of LFT elevation, serologic confirmation of syphilis, exclusion of other causes, and normalization of LFTs after antimicrobial therapy. A rash on the palms and soles, as seen in our patient, is also a hallmark feature of secondary syphilis and a valuable diagnostic clue. This case reinforces the importance of considering syphilis in the differential diagnosis of unexplained liver enzyme elevations and bile duct abnormalities, particularly in patients with risk factors for STIs. Early recognition and treatment can prevent unnecessary interventions and lead to complete resolution of hepatic dysfunction.
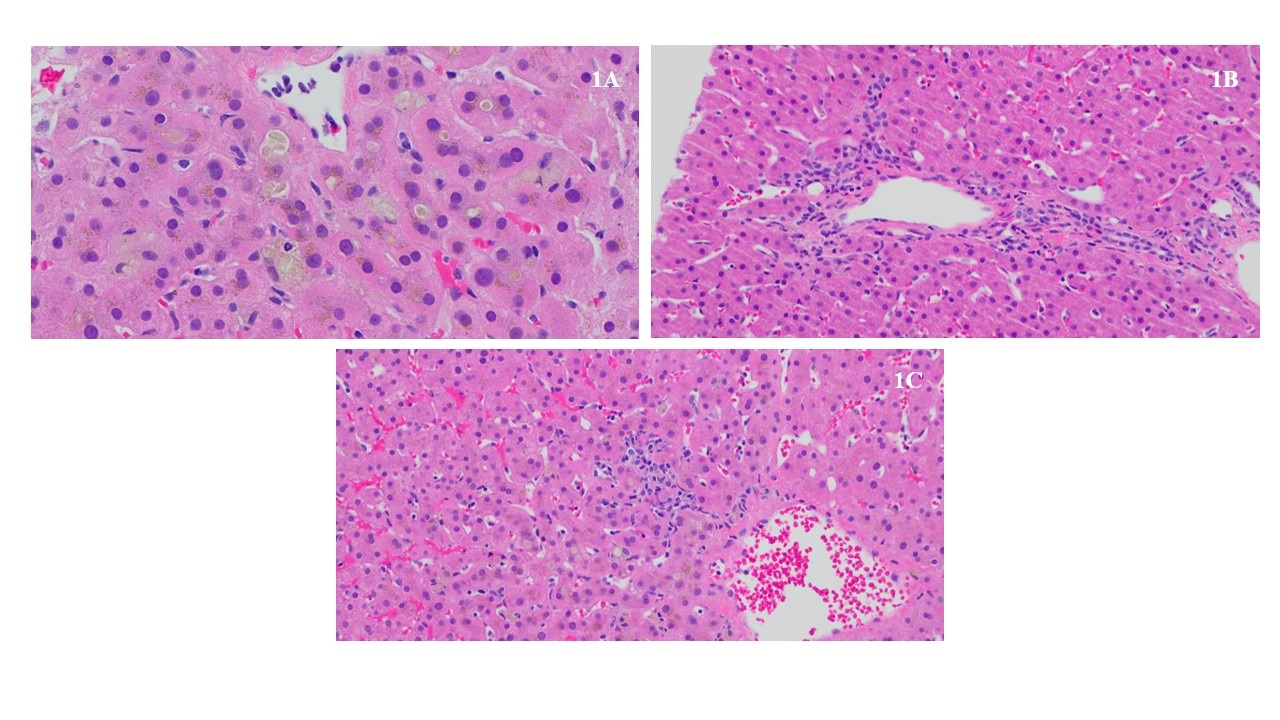
Figure: Figure 1A: High power of lobule with canalicular and hepatocellular cholestasis around a central vein.
Figure 1B: Portal tract with bile ductular proliferation and scant inflammation.
Figure 1C: Focus of lobular lymphocytic inflammation in zone 3 (centrilobular).
Disclosures:
Leslie Graus indicated no relevant financial relationships.
Monica Patel indicated no relevant financial relationships.
Charlotte Ryan indicated no relevant financial relationships.
Sarah McPherson indicated no relevant financial relationships.
Sarah Enslin: AbbVie – Consultant. Ardelyx – Consultant. Castle Biosciences – Consultant. Exact Sciences – Consultant. Ironwood Pharmaceuticals – Consultant. Johnson & Johnson – Consultant. NovoNordisk – Consultant.
Vivek Kaul indicated no relevant financial relationships.
Patrick Twohig indicated no relevant financial relationships.
Leslie Graus, PA-C, Monica Patel, MD, Charlotte Ryan, MD, Sarah McPherson, NP, Sarah Enslin, PA, Vivek Kaul, MD, FACG, Patrick Twohig, MD, MPH. P1752 - Treponema Tricks the Liver: A Case of Reversible Cholangiopathy in Disguise, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

