Sunday Poster Session
Category: Liver
P1749 - Acute Hepatic Decompensation After Medication Cessation in a Patient With Previously Well-Controlled Chronic Hepatitis B
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- SA
Saeed Ahmad, MBBS, MD
Beth Israel Deaconess Medical Center, Harvard Medical School
Brookline, MA
Presenting Author(s)
Saeed Ahmad, MBBS, MD1, Syed Bilal Shah, MD2, Sadia Paracha, MD3, Ashraf Ullah, MD3, Rahmat Ali, MD3, Daryl T.Y. Lau, MD3
1Beth Israel Deaconess Medical Center, Harvard Medical School, Brookline, MA; 2Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, Boston, MA; 3Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA
Introduction: Non-compliance to nucleos(t)side (NUC) therapy even after long-term HBV DNA suppression is an important cause of severe HBV reactivation. We present a patient with hepatic decompensation requiring hospitalization after treatment discontinuation.
Case Description/
Methods: The patient is a 58-year-old Asian male with HBeAg negative chronic hepatitis B (CHB). He had immune-active CHB 12 years ago with significant viremia (HBV DNA: 7.4 log IU/ml) and elevated serum aminotransferases (ALT: 173; AST 98 U/l). The baseline liver biopsy reported moderate inflammation, and stage 4 fibrosis (cirrhosis). His hepatic synthetic function was normal. Abdominal ultrasound and EGD did not show signs of portal hypertension. With entecavir 0.5 mg daily, his ALT and AST normalized with undetectable HBV DNA. After 10 years of continuous NUC treatment, he had fibrosis regression to stage 0-1 by Fibroscan. Approximately 1 year ago, he self-stopped entecavir and was lost to follow-up. About 9 months later, he developed profound fatigue with yellowing of skin and sclera within 1-2 weeks. In the hospital, he was found to have severe hepatitis B with ALT peaked at 4,127 U/L, and HBV DNA at 8.5 log IU/ml [Figure]. There were signs of hepatic failure with bilirubin increased to 30.0 mg/dl, high INR at 2.2, and low albumin of 3.1 g/dL. He had mild hepatic encephalopathy and MELD score was up to 30. Liver transplantation work up was initiated but his liver condition gradually improved within 7-10 days on Tenofovir (TDF). At discharge, his liver function improved. He remained weak with poor appetite and required nutritional supplement. About 4 weeks after returning home, his liver function further improved with bilirubin down to 8.0mg/dl, INR 1.2 and albumin 3.7 g/dL. Despite resolving hepatitis with HBV DNA reduced to 2.9 log IU/ml and ALT < 200 U/L, his AFP remained high at 1,790 ng/mL with no concerning liver lesion. AFP decreased to 183 ng/mL 4 weeks later and the AFP-L3 was within normal. He was able to tolerate normal diet and stayed compliant in taking NUC therapy.
Discussion: This case highlights the importance of medication compliance in managing patients with chronic hepatitis B. This is particularly crucial for those with pre-existing advanced fibrosis. Despite prolonged viral suppression and fibrosis regression, severe HBV reactivation leading to hepatic decompensation remains a concern with NUC cessation. Of note, AFP can be significantly elevated during acute inflammation with hepatic regeneration.
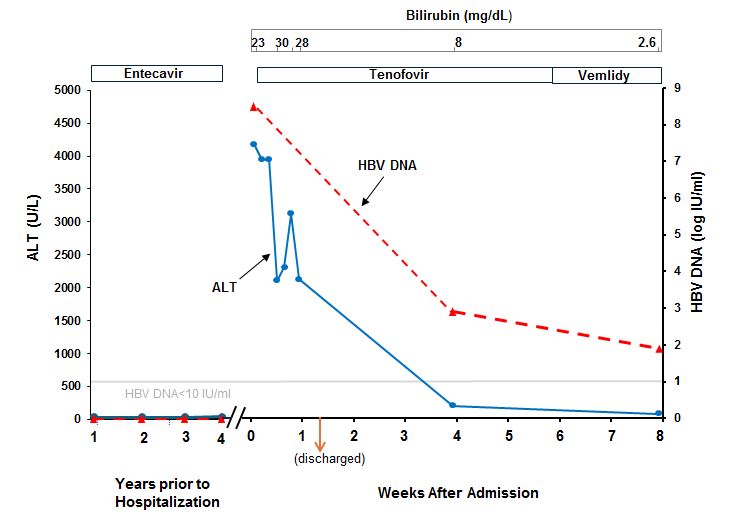
Figure: Clinical course of the patient with acute hepatic decompensation and recovery
Disclosures:
Saeed Ahmad indicated no relevant financial relationships.
Syed Bilal Shah indicated no relevant financial relationships.
Sadia Paracha indicated no relevant financial relationships.
Ashraf Ullah indicated no relevant financial relationships.
Rahmat Ali indicated no relevant financial relationships.
Daryl T.Y. Lau indicated no relevant financial relationships.
Saeed Ahmad, MBBS, MD1, Syed Bilal Shah, MD2, Sadia Paracha, MD3, Ashraf Ullah, MD3, Rahmat Ali, MD3, Daryl T.Y. Lau, MD3. P1749 - Acute Hepatic Decompensation After Medication Cessation in a Patient With Previously Well-Controlled Chronic Hepatitis B, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Beth Israel Deaconess Medical Center, Harvard Medical School, Brookline, MA; 2Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, Boston, MA; 3Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA
Introduction: Non-compliance to nucleos(t)side (NUC) therapy even after long-term HBV DNA suppression is an important cause of severe HBV reactivation. We present a patient with hepatic decompensation requiring hospitalization after treatment discontinuation.
Case Description/
Methods: The patient is a 58-year-old Asian male with HBeAg negative chronic hepatitis B (CHB). He had immune-active CHB 12 years ago with significant viremia (HBV DNA: 7.4 log IU/ml) and elevated serum aminotransferases (ALT: 173; AST 98 U/l). The baseline liver biopsy reported moderate inflammation, and stage 4 fibrosis (cirrhosis). His hepatic synthetic function was normal. Abdominal ultrasound and EGD did not show signs of portal hypertension. With entecavir 0.5 mg daily, his ALT and AST normalized with undetectable HBV DNA. After 10 years of continuous NUC treatment, he had fibrosis regression to stage 0-1 by Fibroscan. Approximately 1 year ago, he self-stopped entecavir and was lost to follow-up. About 9 months later, he developed profound fatigue with yellowing of skin and sclera within 1-2 weeks. In the hospital, he was found to have severe hepatitis B with ALT peaked at 4,127 U/L, and HBV DNA at 8.5 log IU/ml [Figure]. There were signs of hepatic failure with bilirubin increased to 30.0 mg/dl, high INR at 2.2, and low albumin of 3.1 g/dL. He had mild hepatic encephalopathy and MELD score was up to 30. Liver transplantation work up was initiated but his liver condition gradually improved within 7-10 days on Tenofovir (TDF). At discharge, his liver function improved. He remained weak with poor appetite and required nutritional supplement. About 4 weeks after returning home, his liver function further improved with bilirubin down to 8.0mg/dl, INR 1.2 and albumin 3.7 g/dL. Despite resolving hepatitis with HBV DNA reduced to 2.9 log IU/ml and ALT < 200 U/L, his AFP remained high at 1,790 ng/mL with no concerning liver lesion. AFP decreased to 183 ng/mL 4 weeks later and the AFP-L3 was within normal. He was able to tolerate normal diet and stayed compliant in taking NUC therapy.
Discussion: This case highlights the importance of medication compliance in managing patients with chronic hepatitis B. This is particularly crucial for those with pre-existing advanced fibrosis. Despite prolonged viral suppression and fibrosis regression, severe HBV reactivation leading to hepatic decompensation remains a concern with NUC cessation. Of note, AFP can be significantly elevated during acute inflammation with hepatic regeneration.
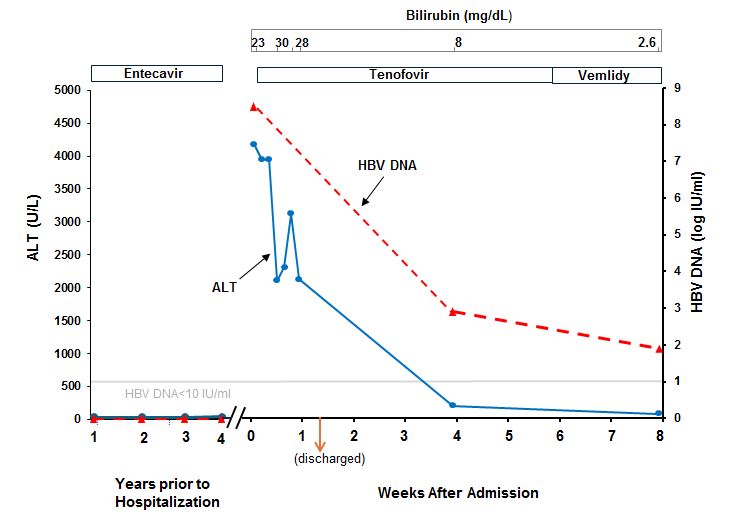
Figure: Clinical course of the patient with acute hepatic decompensation and recovery
Disclosures:
Saeed Ahmad indicated no relevant financial relationships.
Syed Bilal Shah indicated no relevant financial relationships.
Sadia Paracha indicated no relevant financial relationships.
Ashraf Ullah indicated no relevant financial relationships.
Rahmat Ali indicated no relevant financial relationships.
Daryl T.Y. Lau indicated no relevant financial relationships.
Saeed Ahmad, MBBS, MD1, Syed Bilal Shah, MD2, Sadia Paracha, MD3, Ashraf Ullah, MD3, Rahmat Ali, MD3, Daryl T.Y. Lau, MD3. P1749 - Acute Hepatic Decompensation After Medication Cessation in a Patient With Previously Well-Controlled Chronic Hepatitis B, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
