Sunday Poster Session
Category: Liver
P1740 - Hemorrhagic Hepatic Adenoma in a Young Obese Female on Long-Term Oral Contraceptives
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- JA
John K. Appiah, MD
Geisinger Wyoming Valley Medical Center
Wilkes-Barre, PA
Presenting Author(s)
John K. Appiah, MD1, Danial Nadeem, MD1, Nikita Garg, MD1, Edward A. Danso, MD2, Shivam Patel, MD1
1Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 2Korle-Bu Teaching Hospital, Accra, Greater Accra, Ghana
Introduction: Hepatic adenomas are rare, benign liver tumors primarily affecting women of reproductive age. These tumors are usually asymptomatic but may hemorrhage, rupture, or, rarely, undergo malignant transformation. Hemorrhage is the most common and potentially life-threatening complication. Prompt recognition is essential in young women presenting with abdominal pain and relevant risk factors.
Case Description/
Methods: A 36-year-old obese female (BMI 39.7 kg/m²) with a 16-year history of norethindrone-ethinyl estradiol use presented with sudden, severe epigastric pain following exercise. She was hypertensive and tachycardic on arrival. Laboratory evaluation showed elevated liver enzymes (AST 152 U/L, ALT 525 U/L), mild anemia (Hb 10.6 g/dL), but otherwise unremarkable findings. Non-contrast computed tomography (CT) of the abdomen demonstrated an ill-defined left hepatic mass with hyperdense areas suggestive of hemorrhage (Figure 1A). Magnetic resonance imaging (MRI) confirmed the presence of at least eight hepatic adenomas, the largest measuring 11.4 cm, with evidence of intralesional and subcapsular hemorrhage (Figure 1B).
The patient underwent successful transarterial embolization of the dominant left lobe adenoma by interventional radiology. She was discharged on hospital day 4, and her estrogen containing oral contraceptive was discontinued.
Two months later, she returned with recurrent abdominal pain. Surgical consultation was obtained, and she underwent laparoscopic hand-assisted left lateral segmentectomy, partial right lobe resection (segments VI/VII), and cholecystectomy. Histopathology confirmed hepatic adenomas. Her postoperative course was uneventful, and she remained asymptomatic at the one-month follow-up.
Discussion: This case highlights the hemorrhagic risk associated with multiple hepatic adenomas in the setting of long-term estrogen exposure and obesity. Hemorrhage occurs in up to 30% of cases and is the most common serious complication. MRI remains the preferred imaging modality for diagnosis and surveillance. While transarterial embolization is an effective initial intervention for hemodynamically stable patients with active bleeding, recurrent symptoms and high lesion burden may necessitate surgical resection for definitive management.
This case reinforces the importance of early cessation of hormonal therapy and the role of a multidisciplinary team, including hepatology, radiology, and surgery, in optimizing outcomes for high-risk patients.
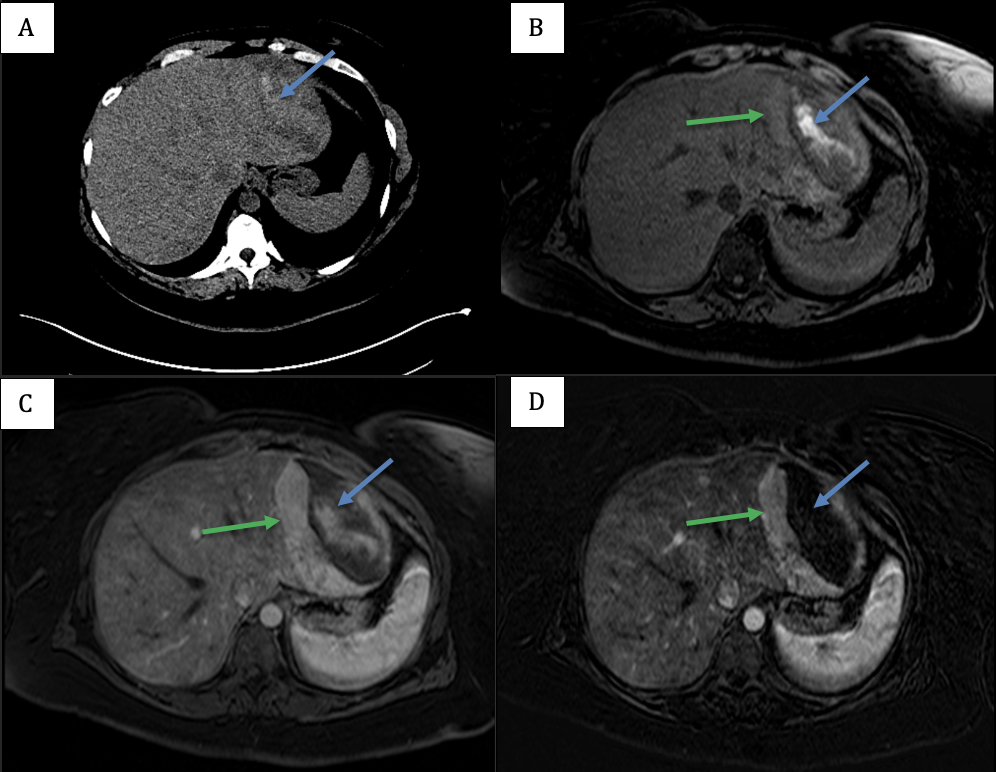
Figure: Figure 1; A-Axial image from a noncontrast CT demonstrates a large left hepatic lobe heterogeneous mass containing hyperdense components from hemorrhage (blue arrow).
B-Axial T1 fat-saturated precontrast MRI sequence demonstrates the hyperdense areas on CT to be T1 hyperintense (blue arrow), confirming hemorrhage. Note that the medial component of the mass (green arrow) has intrinsic mild T1 hyperintense signal, characteristic of an adenoma.
C-Axial T1 fat-saturated postcontrast arterial phase MRI sequence shows avid enhancement of the mass (green arrow) as would be expected in an adenoma, and no enhancement of the hemorrhagic component (blue arrow), as confirmed on the corresponding subtraction image D.
Disclosures:
John Appiah indicated no relevant financial relationships.
Danial Nadeem indicated no relevant financial relationships.
Nikita Garg indicated no relevant financial relationships.
Edward Danso indicated no relevant financial relationships.
Shivam Patel indicated no relevant financial relationships.
John K. Appiah, MD1, Danial Nadeem, MD1, Nikita Garg, MD1, Edward A. Danso, MD2, Shivam Patel, MD1. P1740 - Hemorrhagic Hepatic Adenoma in a Young Obese Female on Long-Term Oral Contraceptives, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 2Korle-Bu Teaching Hospital, Accra, Greater Accra, Ghana
Introduction: Hepatic adenomas are rare, benign liver tumors primarily affecting women of reproductive age. These tumors are usually asymptomatic but may hemorrhage, rupture, or, rarely, undergo malignant transformation. Hemorrhage is the most common and potentially life-threatening complication. Prompt recognition is essential in young women presenting with abdominal pain and relevant risk factors.
Case Description/
Methods: A 36-year-old obese female (BMI 39.7 kg/m²) with a 16-year history of norethindrone-ethinyl estradiol use presented with sudden, severe epigastric pain following exercise. She was hypertensive and tachycardic on arrival. Laboratory evaluation showed elevated liver enzymes (AST 152 U/L, ALT 525 U/L), mild anemia (Hb 10.6 g/dL), but otherwise unremarkable findings. Non-contrast computed tomography (CT) of the abdomen demonstrated an ill-defined left hepatic mass with hyperdense areas suggestive of hemorrhage (Figure 1A). Magnetic resonance imaging (MRI) confirmed the presence of at least eight hepatic adenomas, the largest measuring 11.4 cm, with evidence of intralesional and subcapsular hemorrhage (Figure 1B).
The patient underwent successful transarterial embolization of the dominant left lobe adenoma by interventional radiology. She was discharged on hospital day 4, and her estrogen containing oral contraceptive was discontinued.
Two months later, she returned with recurrent abdominal pain. Surgical consultation was obtained, and she underwent laparoscopic hand-assisted left lateral segmentectomy, partial right lobe resection (segments VI/VII), and cholecystectomy. Histopathology confirmed hepatic adenomas. Her postoperative course was uneventful, and she remained asymptomatic at the one-month follow-up.
Discussion: This case highlights the hemorrhagic risk associated with multiple hepatic adenomas in the setting of long-term estrogen exposure and obesity. Hemorrhage occurs in up to 30% of cases and is the most common serious complication. MRI remains the preferred imaging modality for diagnosis and surveillance. While transarterial embolization is an effective initial intervention for hemodynamically stable patients with active bleeding, recurrent symptoms and high lesion burden may necessitate surgical resection for definitive management.
This case reinforces the importance of early cessation of hormonal therapy and the role of a multidisciplinary team, including hepatology, radiology, and surgery, in optimizing outcomes for high-risk patients.
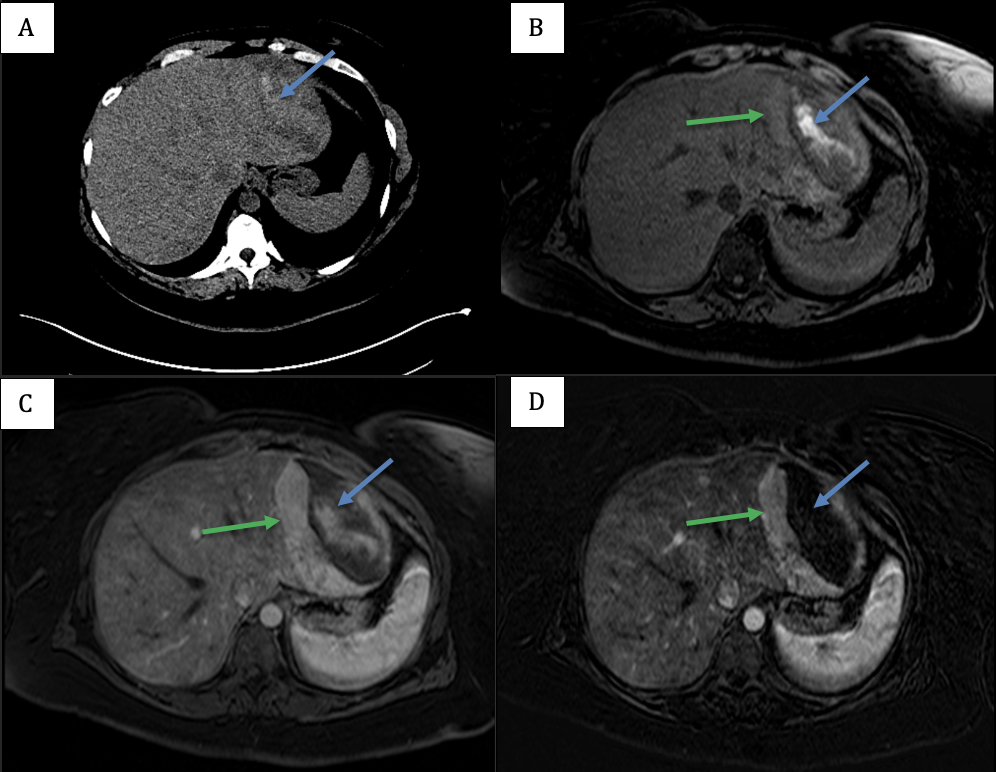
Figure: Figure 1; A-Axial image from a noncontrast CT demonstrates a large left hepatic lobe heterogeneous mass containing hyperdense components from hemorrhage (blue arrow).
B-Axial T1 fat-saturated precontrast MRI sequence demonstrates the hyperdense areas on CT to be T1 hyperintense (blue arrow), confirming hemorrhage. Note that the medial component of the mass (green arrow) has intrinsic mild T1 hyperintense signal, characteristic of an adenoma.
C-Axial T1 fat-saturated postcontrast arterial phase MRI sequence shows avid enhancement of the mass (green arrow) as would be expected in an adenoma, and no enhancement of the hemorrhagic component (blue arrow), as confirmed on the corresponding subtraction image D.
Disclosures:
John Appiah indicated no relevant financial relationships.
Danial Nadeem indicated no relevant financial relationships.
Nikita Garg indicated no relevant financial relationships.
Edward Danso indicated no relevant financial relationships.
Shivam Patel indicated no relevant financial relationships.
John K. Appiah, MD1, Danial Nadeem, MD1, Nikita Garg, MD1, Edward A. Danso, MD2, Shivam Patel, MD1. P1740 - Hemorrhagic Hepatic Adenoma in a Young Obese Female on Long-Term Oral Contraceptives, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
