Sunday Poster Session
Category: Liver
P1730 - Cholestatic Hepatitis in an Adult Patient off Immunosuppression: A Rare Presentation of Bartonella Henselae Infection
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Rishaan R. Sharma, MD (he/him/his)
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Rishaan R. Sharma, MD, Shilpa Junna, MD
Cleveland Clinic Foundation, Cleveland, OH
Introduction: Bartonella henselae is a facultative intracellular gram-negative bacterium most often associated with cat scratch disease. Hepatic involvement is rare and typically presents as granulomatous hepatitis or peliosis hepatis in immunocompromised hosts. We report a diagnostically challenging case of isolated cholestatic hepatitis in a patient with SLE not receiving immunosuppression, ultimately attributed to Bartonella henselae infection.
Case Description/
Methods:
A 42-year-old woman with SLE (off immunosuppressive therapy for several months) and remote alcohol use disorder presented with six weeks of right upper quadrant pain, abdominal distension, malaise, and intermittent low-grade fevers. Liver enzymes showed elevated alkaline phosphatase (peak 1,461 U/L), normal ALT/AST, and total bilirubin of 3.1 mg/dL. Imaging revealed hepatosplenomegaly without biliary obstruction. MRCP showed diffuse hepatic heterogeneity without biliary dilation or discrete lesions. Liver biopsy demonstrated lobular hepatitis with intrasinusoidal T-cell infiltration and macrovesicular steatosis, but no granulomas, bile duct injury, autoimmune hepatitis, or congestive hepatopathy. The patient had normal filling pressures on echocardiography and had not taken hepatotoxic medications for several months.
Given underlying valvular disease and prior echocardiographic evidence of endocarditis, an infectious workup was pursued. Viral hepatitis panels, HIV, and TB testing were negative. Autoimmune markers including ANA, AMA, and anti-gp210 were unrevealing, though smooth muscle antibody was positive at low titer. Serum B. henselae PCR returned positive. The patient reported frequent cat exposure. She was started on doxycycline and ceftriaxone, with rapid biochemical improvement. Aortic valve replacement revealed Bartonella microabscesses, confirming the diagnosis.
Discussion: This case illustrates a rare manifestation of Bartonella henselae as isolated cholestatic hepatitis in a patient who, despite autoimmune disease, was not on immunosuppression or hepatotoxic drugs. Classical histologic features such as granulomas or peliosis were absent. The differential included autoimmune, drug-induced, and congestive hepatopathy, but was excluded by histology and history. Clinical suspicion, exposure history, and confirmatory PCR were critical. Timely treatment led to rapid improvement. Bartonella should be considered in cholestatic hepatitis of unclear etiology in all patients, even those not traditionally considered immunocompromised.
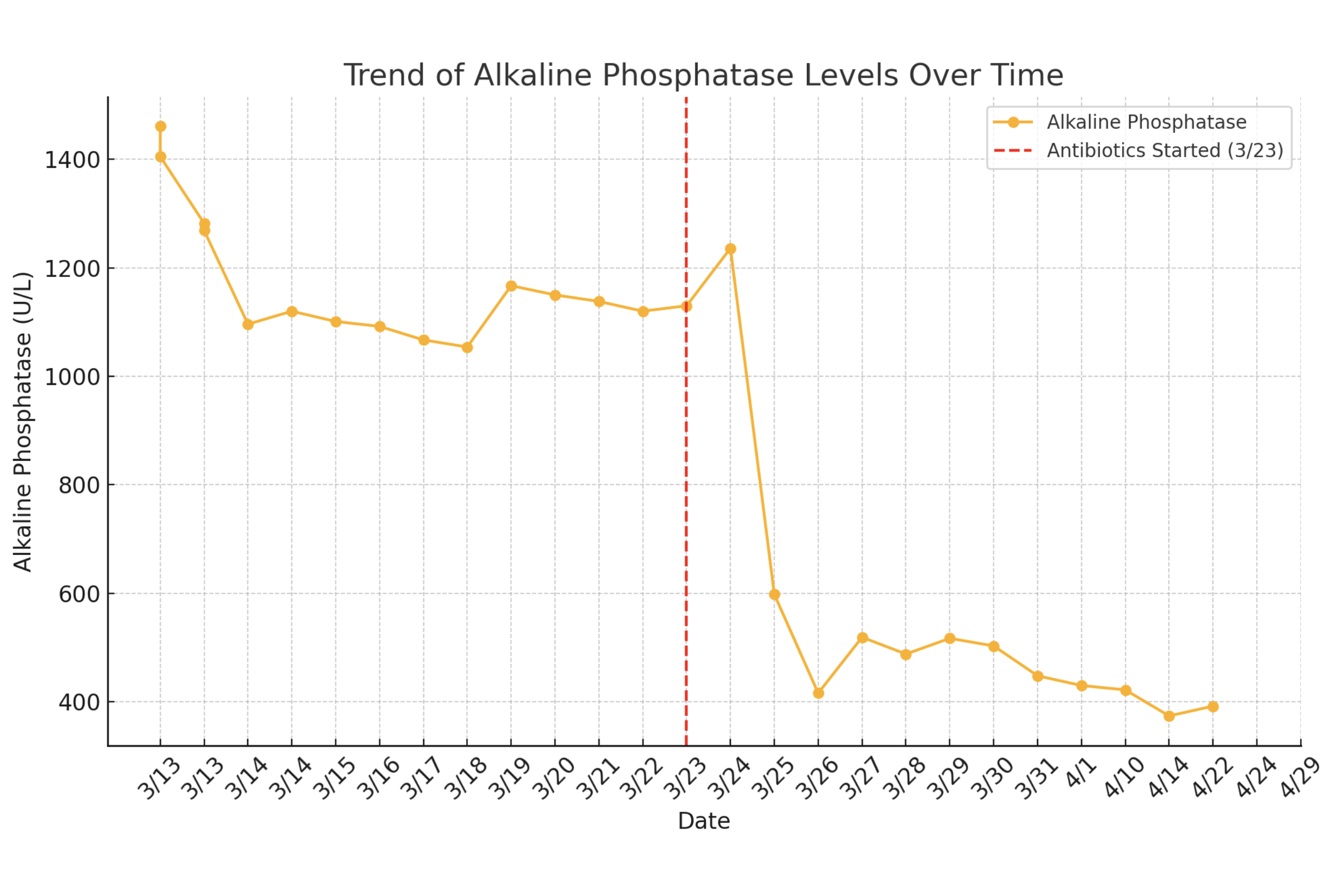
Figure: Image 1. Liver ultrasound without lesion.
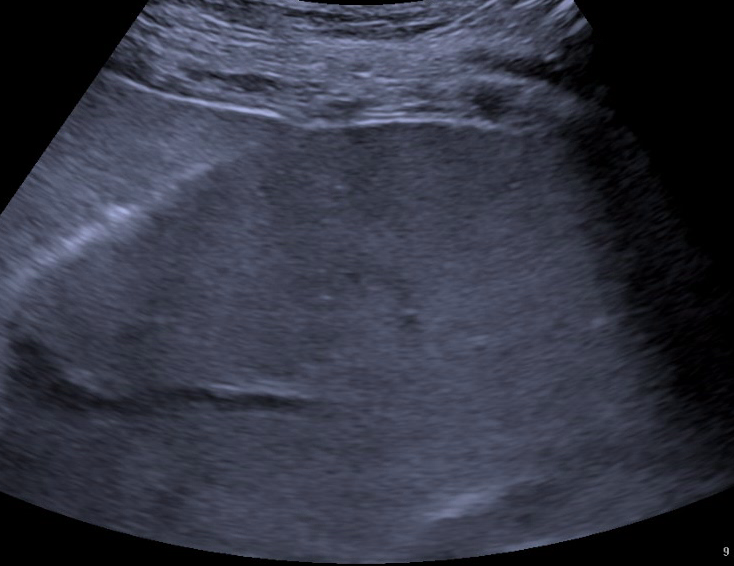
Figure: Figure 1. Alkaline Phosphatase trend.
Disclosures:
Rishaan Sharma indicated no relevant financial relationships.
Shilpa Junna indicated no relevant financial relationships.
Rishaan R. Sharma, MD, Shilpa Junna, MD. P1730 - Cholestatic Hepatitis in an Adult Patient off Immunosuppression: A Rare Presentation of Bartonella Henselae Infection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Cleveland Clinic Foundation, Cleveland, OH
Introduction: Bartonella henselae is a facultative intracellular gram-negative bacterium most often associated with cat scratch disease. Hepatic involvement is rare and typically presents as granulomatous hepatitis or peliosis hepatis in immunocompromised hosts. We report a diagnostically challenging case of isolated cholestatic hepatitis in a patient with SLE not receiving immunosuppression, ultimately attributed to Bartonella henselae infection.
Case Description/
Methods:
A 42-year-old woman with SLE (off immunosuppressive therapy for several months) and remote alcohol use disorder presented with six weeks of right upper quadrant pain, abdominal distension, malaise, and intermittent low-grade fevers. Liver enzymes showed elevated alkaline phosphatase (peak 1,461 U/L), normal ALT/AST, and total bilirubin of 3.1 mg/dL. Imaging revealed hepatosplenomegaly without biliary obstruction. MRCP showed diffuse hepatic heterogeneity without biliary dilation or discrete lesions. Liver biopsy demonstrated lobular hepatitis with intrasinusoidal T-cell infiltration and macrovesicular steatosis, but no granulomas, bile duct injury, autoimmune hepatitis, or congestive hepatopathy. The patient had normal filling pressures on echocardiography and had not taken hepatotoxic medications for several months.
Given underlying valvular disease and prior echocardiographic evidence of endocarditis, an infectious workup was pursued. Viral hepatitis panels, HIV, and TB testing were negative. Autoimmune markers including ANA, AMA, and anti-gp210 were unrevealing, though smooth muscle antibody was positive at low titer. Serum B. henselae PCR returned positive. The patient reported frequent cat exposure. She was started on doxycycline and ceftriaxone, with rapid biochemical improvement. Aortic valve replacement revealed Bartonella microabscesses, confirming the diagnosis.
Discussion: This case illustrates a rare manifestation of Bartonella henselae as isolated cholestatic hepatitis in a patient who, despite autoimmune disease, was not on immunosuppression or hepatotoxic drugs. Classical histologic features such as granulomas or peliosis were absent. The differential included autoimmune, drug-induced, and congestive hepatopathy, but was excluded by histology and history. Clinical suspicion, exposure history, and confirmatory PCR were critical. Timely treatment led to rapid improvement. Bartonella should be considered in cholestatic hepatitis of unclear etiology in all patients, even those not traditionally considered immunocompromised.
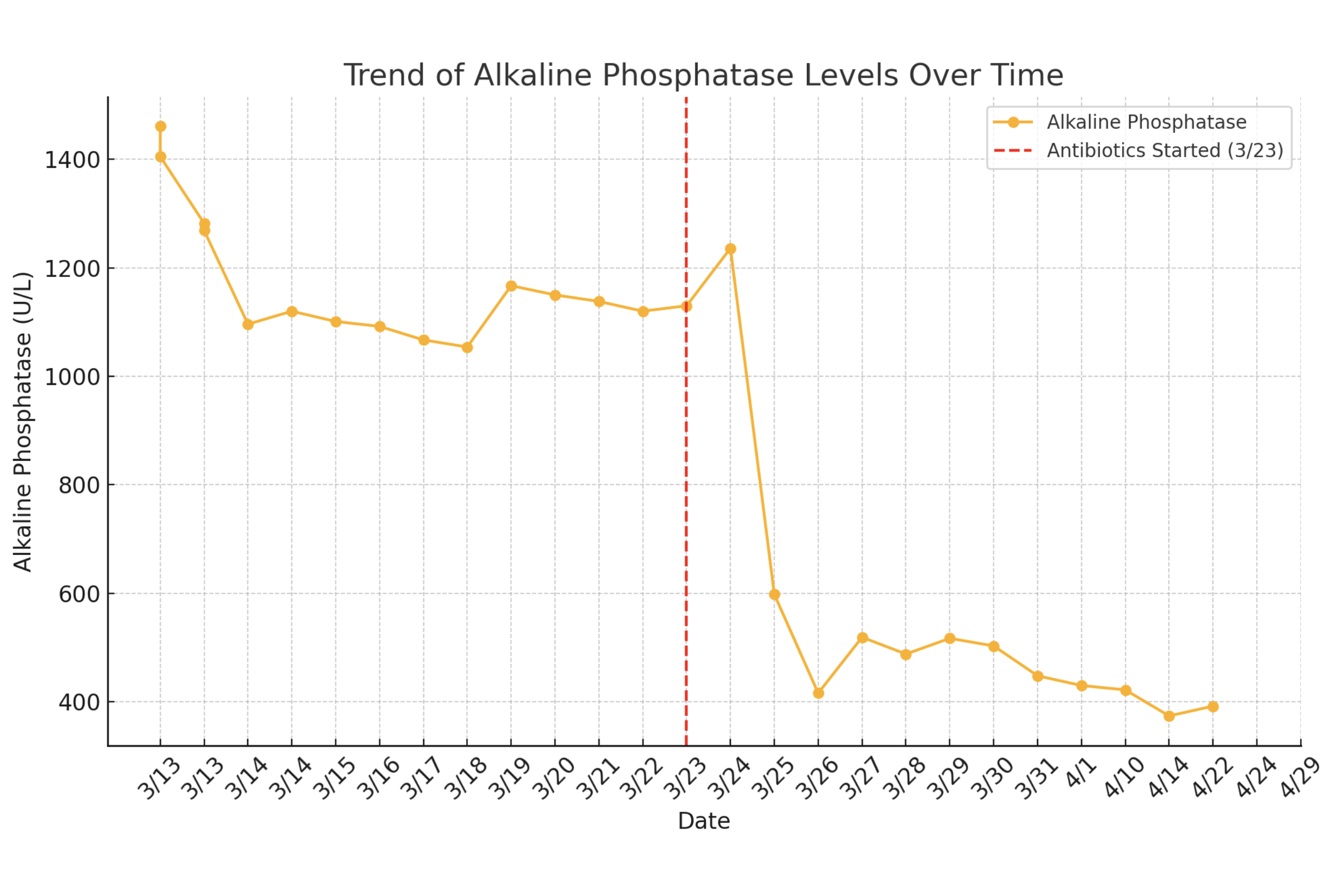
Figure: Image 1. Liver ultrasound without lesion.
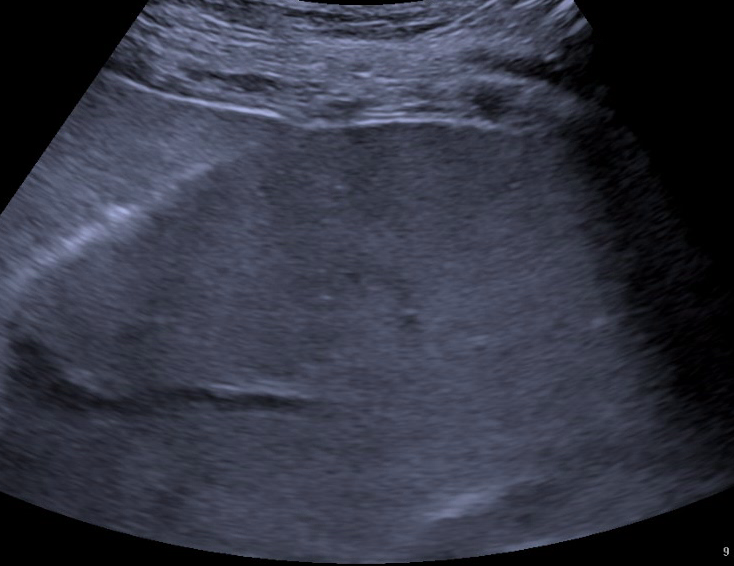
Figure: Figure 1. Alkaline Phosphatase trend.
Disclosures:
Rishaan Sharma indicated no relevant financial relationships.
Shilpa Junna indicated no relevant financial relationships.
Rishaan R. Sharma, MD, Shilpa Junna, MD. P1730 - Cholestatic Hepatitis in an Adult Patient off Immunosuppression: A Rare Presentation of Bartonella Henselae Infection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
