Sunday Poster Session
Category: Liver
P1727 - Toxins and Ticks: Acute Encephalopathy in a Farmer With Wilson Disease
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Casey Wizner, MD (she/her/hers)
Yale New Haven Hospital
New Haven, CT
Presenting Author(s)
Casey Wizner, MD1, Ysabel Ilagan-Ying, MD2
1Yale New Haven Hospital, New Haven, CT; 2Yale University, New Haven, CT
Introduction: Wilson disease is a rare autosomal recessive disorder of copper metabolism that can remain stable with chelation therapy and a low-copper diet. Acute-on-chronic liver failure (ACLF) is a rapidly progressive syndrome of acute hepatic decompensation in the setting of chronic liver disease, with high short-term mortality. Diagnosing ACLF in Wilson disease is complex due to similar presentations of hepatic encephalopathy and neurologic involvement of Wilson disease. We report the case of ACLF in a patient with stable Wilson disease, triggered by drug-induced liver injury (DILI) and acute tick-borne infections, where the New Wilson Index (NWI) guided timely transplant referral.
Case Description/
Methods: A 61-year-old male farmer with compensated Wilson disease on d-penicillamine presented with jaundice, confusion, and abdominal distention. Five weeks prior, he began daily amoxicillin for dental issues. He developed a cough, pruritus, fevers, and neuropsychiatric symptoms, prompting presentation. Two ticks were removed. Initial labs showed AST 169 U/L, ALT 167 U/L, ALP 110 U/L, total bilirubin 12.4 mg/dL, platelets 171 ×10³/µL, INR 3.2, WBC 12.6 ×10³/μL, albumin 2.2 g/dL, Lyme IgM and Coxiella burnetti Phase II IgG positive, hepatitis panel negative. A CTA abdomen/pelvis showed a nodular liver and ascites. His presentation was concerning for ACLF, and he was started on lactulose and doxycycline for Lyme infection and transferred to a tertiary academic center. His labs worsened to a peak bilirubin 51.1, INR 7.32, creatinine 4.2. He was placed on continuous dialysis for renal failure. Lumbar puncture was deferred due to coagulopathy, so doxycycline was changed to intravenous ceftriaxone for empiric CNS Lyme treatment. NWI was >11, he was listed as status 1A, and underwent liver transplantation on hospital day 17. Post-op complications included abdominal hematomas and prolonged encephalopathy. He was discharged on day 74.
Discussion: This case highlights diagnostic challenges in ACLF as neuropsychiatric symptoms—hallmarks of both hepatic encephalopathy and neurologic Wilson disease—can confound clinical assessment. In this case, decompensation was likely due to DILI and systemic Lyme disease. Broad infectious workup and detailed history were critical in identifying these triggers. The NWI facilitated urgent transplant referral, underscoring its value in prognostication. Clinicians should maintain a broad differential and consider early transplant evaluation in patients with decompensated Wilson disease.
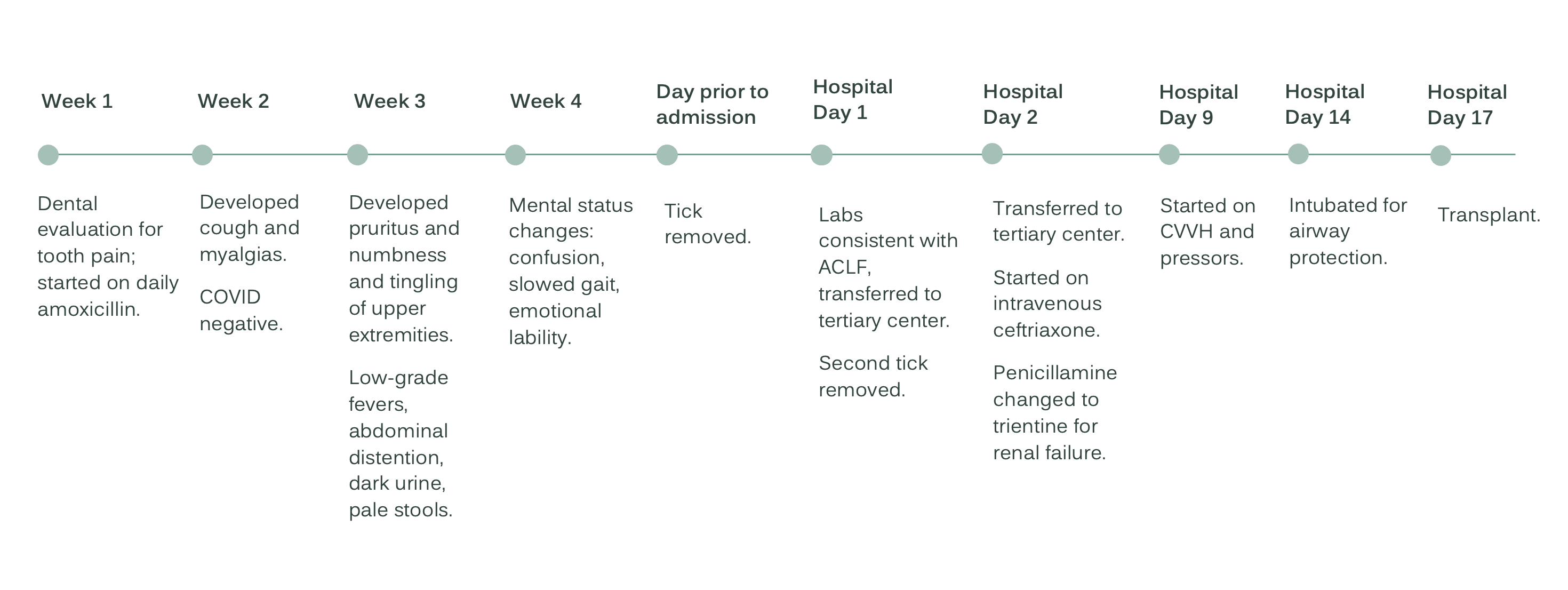
Figure: Case Timeline
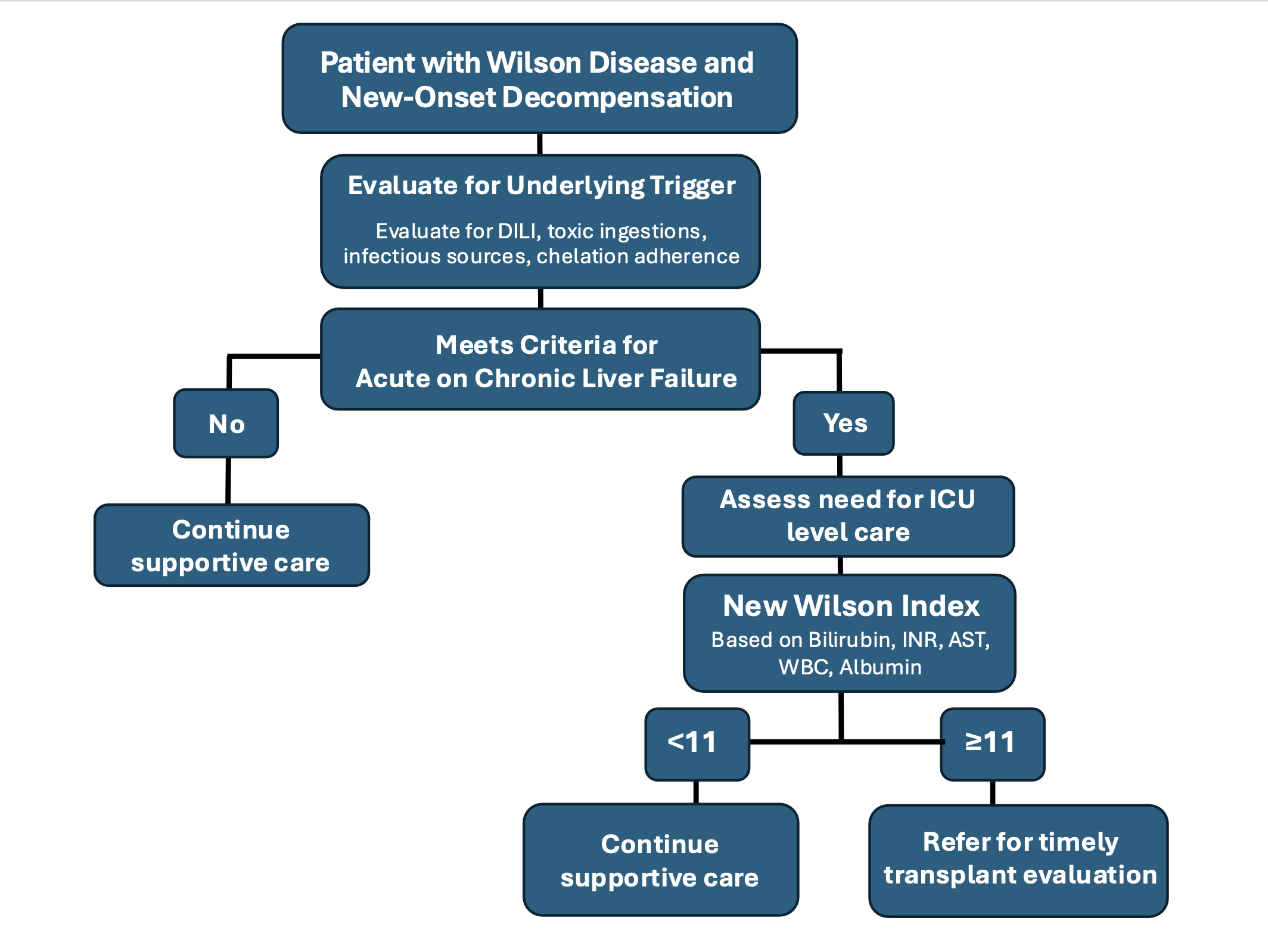
Figure: Decompensated Wilson Disease Management Pathway
Disclosures:
Casey Wizner indicated no relevant financial relationships.
Ysabel Ilagan-Ying indicated no relevant financial relationships.
Casey Wizner, MD1, Ysabel Ilagan-Ying, MD2. P1727 - Toxins and Ticks: Acute Encephalopathy in a Farmer With Wilson Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Yale New Haven Hospital, New Haven, CT; 2Yale University, New Haven, CT
Introduction: Wilson disease is a rare autosomal recessive disorder of copper metabolism that can remain stable with chelation therapy and a low-copper diet. Acute-on-chronic liver failure (ACLF) is a rapidly progressive syndrome of acute hepatic decompensation in the setting of chronic liver disease, with high short-term mortality. Diagnosing ACLF in Wilson disease is complex due to similar presentations of hepatic encephalopathy and neurologic involvement of Wilson disease. We report the case of ACLF in a patient with stable Wilson disease, triggered by drug-induced liver injury (DILI) and acute tick-borne infections, where the New Wilson Index (NWI) guided timely transplant referral.
Case Description/
Methods: A 61-year-old male farmer with compensated Wilson disease on d-penicillamine presented with jaundice, confusion, and abdominal distention. Five weeks prior, he began daily amoxicillin for dental issues. He developed a cough, pruritus, fevers, and neuropsychiatric symptoms, prompting presentation. Two ticks were removed. Initial labs showed AST 169 U/L, ALT 167 U/L, ALP 110 U/L, total bilirubin 12.4 mg/dL, platelets 171 ×10³/µL, INR 3.2, WBC 12.6 ×10³/μL, albumin 2.2 g/dL, Lyme IgM and Coxiella burnetti Phase II IgG positive, hepatitis panel negative. A CTA abdomen/pelvis showed a nodular liver and ascites. His presentation was concerning for ACLF, and he was started on lactulose and doxycycline for Lyme infection and transferred to a tertiary academic center. His labs worsened to a peak bilirubin 51.1, INR 7.32, creatinine 4.2. He was placed on continuous dialysis for renal failure. Lumbar puncture was deferred due to coagulopathy, so doxycycline was changed to intravenous ceftriaxone for empiric CNS Lyme treatment. NWI was >11, he was listed as status 1A, and underwent liver transplantation on hospital day 17. Post-op complications included abdominal hematomas and prolonged encephalopathy. He was discharged on day 74.
Discussion: This case highlights diagnostic challenges in ACLF as neuropsychiatric symptoms—hallmarks of both hepatic encephalopathy and neurologic Wilson disease—can confound clinical assessment. In this case, decompensation was likely due to DILI and systemic Lyme disease. Broad infectious workup and detailed history were critical in identifying these triggers. The NWI facilitated urgent transplant referral, underscoring its value in prognostication. Clinicians should maintain a broad differential and consider early transplant evaluation in patients with decompensated Wilson disease.
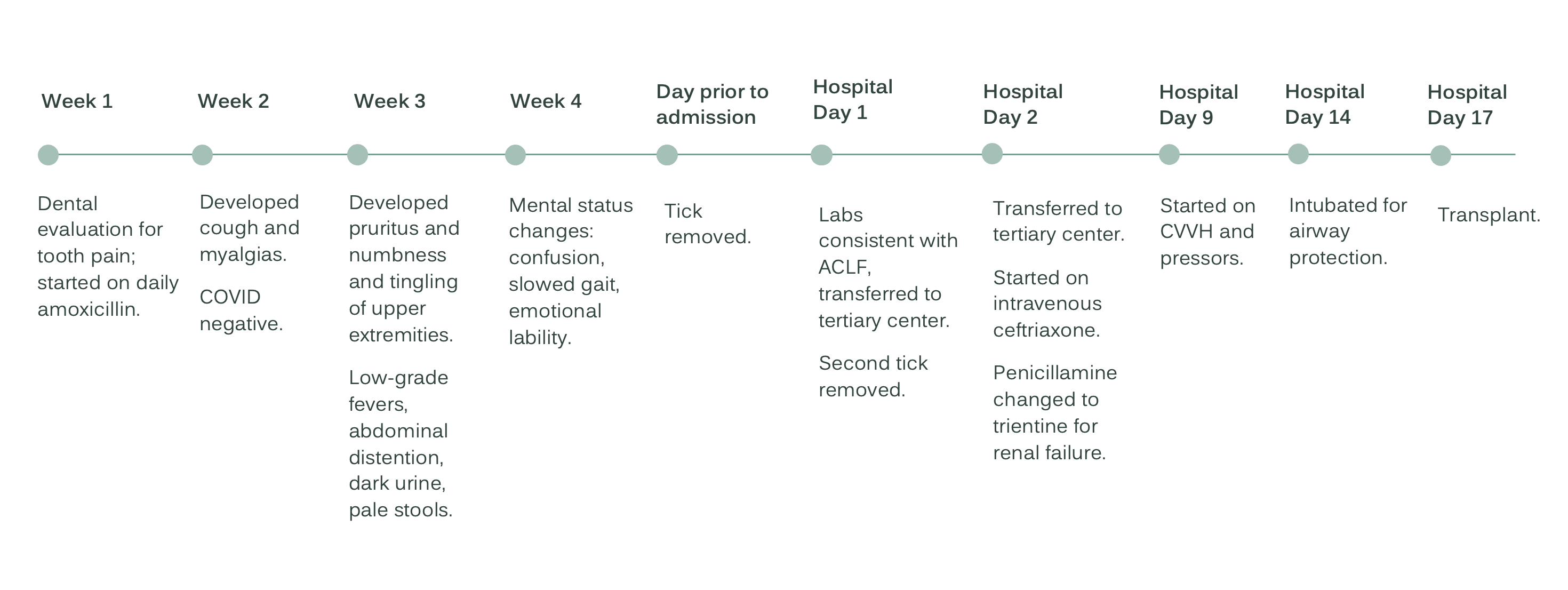
Figure: Case Timeline
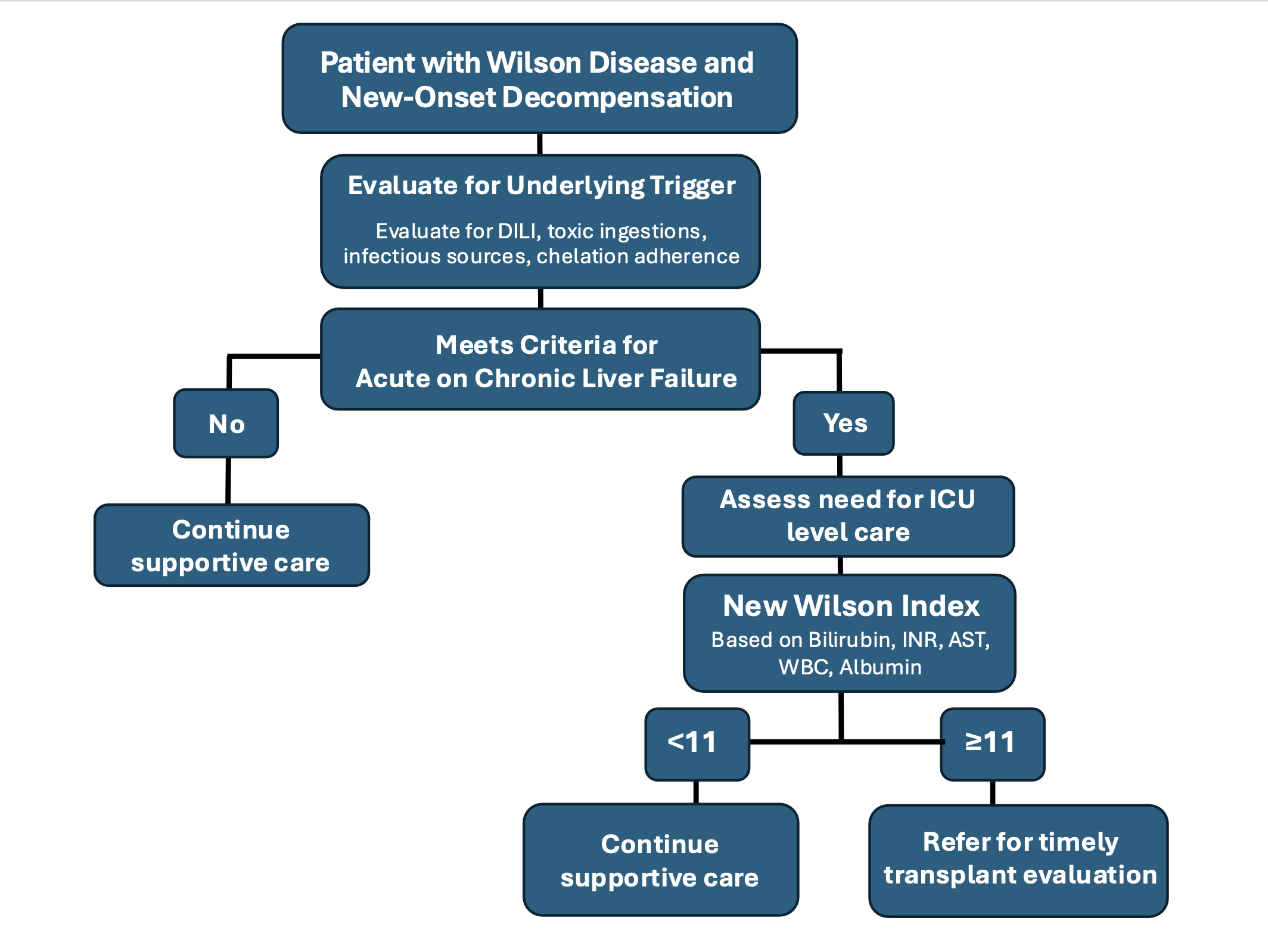
Figure: Decompensated Wilson Disease Management Pathway
Disclosures:
Casey Wizner indicated no relevant financial relationships.
Ysabel Ilagan-Ying indicated no relevant financial relationships.
Casey Wizner, MD1, Ysabel Ilagan-Ying, MD2. P1727 - Toxins and Ticks: Acute Encephalopathy in a Farmer With Wilson Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
