Sunday Poster Session
Category: Liver
P1702 - NASH Cirrhosis, a Risk Factor for Disseminated Cryptococcus: Expanding the Non-HIV Spectrum
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Joshika Agarwal, MD (she/her/hers)
Mercy Catholic Medical Center
Darby, PA
Presenting Author(s)
Joshika Agarwal, MD, Rabia Naseem, MD, Darsh Tusharbhai. Patel, MD, Dhruvan Patel, MD
Mercy Catholic Medical Center, Darby, PA
Introduction: Cryptococcus can cause invasive fungal infection in patients who are immunocompromised, classically associated with HIV/AIDS. Nonalcoholic steatohepatitis (NASH) associated cirrhosis has an uncommon association with disseminated cryptococcal infection, hence recognition and timely intervention becomes crucial for improving patient outcomes.
Case Description/
Methods: A 59-year-old male with a past medical history of NASH cirrhosis, portal hypertension, esophageal varices, recurrent ascites requiring frequent paracentesis, and prior trans jugular intrahepatic portosystemic shunt (TIPS) for hepatic encephalopathy, residing in unsanitary conditions, presented with worsening shortness of breath post-recent paracentesis. Initially, his vitals were stable. However, later he developed fever, hypoxia, and hypotension, requiring supplemental oxygen and ICU admission. Labs showed an elevated white blood cell count and a positive Legionella urine antigen test, for which he was initiated on a 10-day course of azithromycin. His mentation altered and he became drowsy and lethargic over the hospital course with an MRI of the brain revealing leptomeningeal enhancement and basal ganglia nodular lesions consistent with cryptococcal meningoencephalitis. Positive blood cultures from admission confirmed disseminated cryptococcal infection. Chest imaging revealed pulmonary nodules which were suspicious for cryptococcosis. It was difficult to rule out peritoneal involvement as well due to a lack of fluid studies from admission. Notably, HIV testing was negative, and no prior immunosuppressive therapy was reported. The patient was treated with a prolonged antifungal regimen of amphotericin B plus flucytosine, followed by fluconazole consolidation and maintenance therapy. After significant improvement, he was discharged on oral fluconazole maintenance for one year.
Discussion: This case highlights the importance of recognizing cirrhosis particularly secondary to NASH as a significant risk factor for disseminated cryptococcal infection. A high index of suspicion should be maintained for cryptococcal infection in such patients presenting with symptoms such as dyspnea and altered mental status. Early diagnosis and aggressive treatment with antifungal is of paramount importance to prevent mortality. This case also highlights a new avenue of research on the treatment guidelines for non-HIV-positive patients with NASH cirrhosis diagnosed with disseminated cryptococcosis.
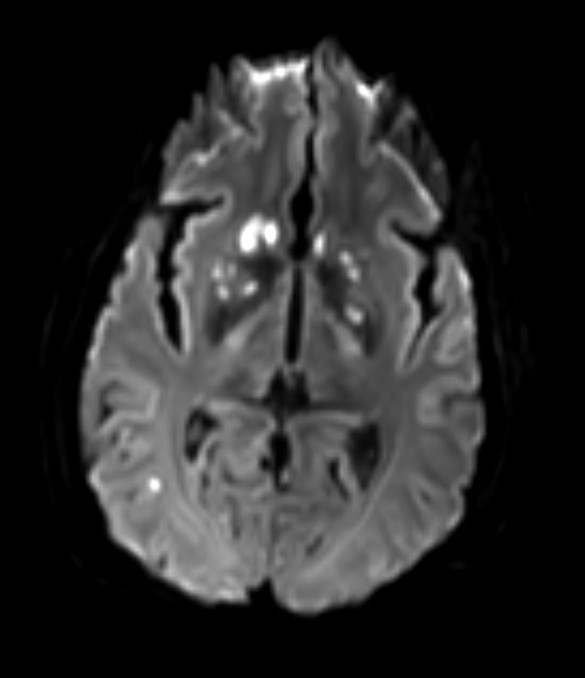
Figure: MRI Brain showing Bilateral nodular lesions involving bilateral basal ganglia, right corona radiata, right centrum semiovale, and right occipital lobe. There is subtle leptomeningeal enhancement in the basal cisterns. Findings are suggestive of central nervous system cryptococcal meningoencephalitis
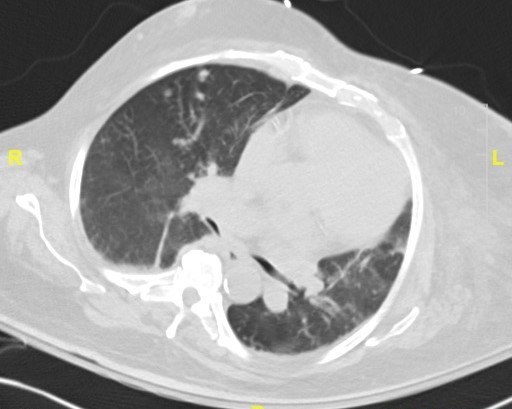
Figure: CT Chest showing Progressive bilateral solitary pulmonary nodules
Disclosures:
Joshika Agarwal indicated no relevant financial relationships.
Rabia Naseem indicated no relevant financial relationships.
Darsh Patel indicated no relevant financial relationships.
Dhruvan Patel indicated no relevant financial relationships.
Joshika Agarwal, MD, Rabia Naseem, MD, Darsh Tusharbhai. Patel, MD, Dhruvan Patel, MD. P1702 - NASH Cirrhosis, a Risk Factor for Disseminated Cryptococcus: Expanding the Non-HIV Spectrum, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Mercy Catholic Medical Center, Darby, PA
Introduction: Cryptococcus can cause invasive fungal infection in patients who are immunocompromised, classically associated with HIV/AIDS. Nonalcoholic steatohepatitis (NASH) associated cirrhosis has an uncommon association with disseminated cryptococcal infection, hence recognition and timely intervention becomes crucial for improving patient outcomes.
Case Description/
Methods: A 59-year-old male with a past medical history of NASH cirrhosis, portal hypertension, esophageal varices, recurrent ascites requiring frequent paracentesis, and prior trans jugular intrahepatic portosystemic shunt (TIPS) for hepatic encephalopathy, residing in unsanitary conditions, presented with worsening shortness of breath post-recent paracentesis. Initially, his vitals were stable. However, later he developed fever, hypoxia, and hypotension, requiring supplemental oxygen and ICU admission. Labs showed an elevated white blood cell count and a positive Legionella urine antigen test, for which he was initiated on a 10-day course of azithromycin. His mentation altered and he became drowsy and lethargic over the hospital course with an MRI of the brain revealing leptomeningeal enhancement and basal ganglia nodular lesions consistent with cryptococcal meningoencephalitis. Positive blood cultures from admission confirmed disseminated cryptococcal infection. Chest imaging revealed pulmonary nodules which were suspicious for cryptococcosis. It was difficult to rule out peritoneal involvement as well due to a lack of fluid studies from admission. Notably, HIV testing was negative, and no prior immunosuppressive therapy was reported. The patient was treated with a prolonged antifungal regimen of amphotericin B plus flucytosine, followed by fluconazole consolidation and maintenance therapy. After significant improvement, he was discharged on oral fluconazole maintenance for one year.
Discussion: This case highlights the importance of recognizing cirrhosis particularly secondary to NASH as a significant risk factor for disseminated cryptococcal infection. A high index of suspicion should be maintained for cryptococcal infection in such patients presenting with symptoms such as dyspnea and altered mental status. Early diagnosis and aggressive treatment with antifungal is of paramount importance to prevent mortality. This case also highlights a new avenue of research on the treatment guidelines for non-HIV-positive patients with NASH cirrhosis diagnosed with disseminated cryptococcosis.
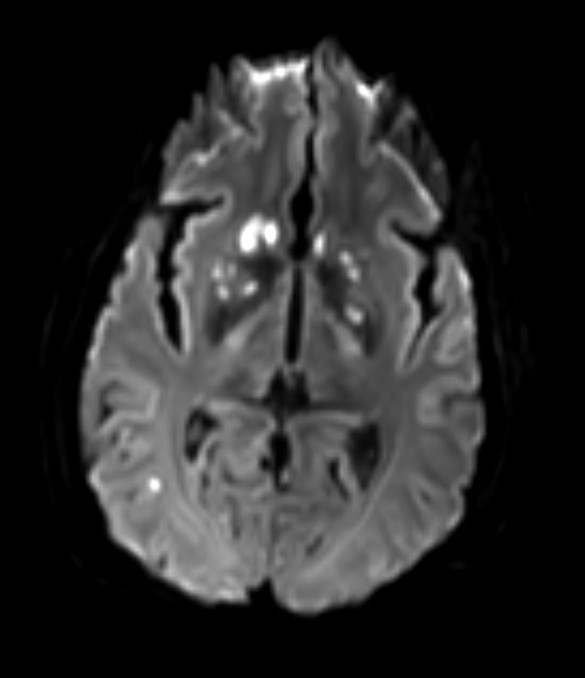
Figure: MRI Brain showing Bilateral nodular lesions involving bilateral basal ganglia, right corona radiata, right centrum semiovale, and right occipital lobe. There is subtle leptomeningeal enhancement in the basal cisterns. Findings are suggestive of central nervous system cryptococcal meningoencephalitis
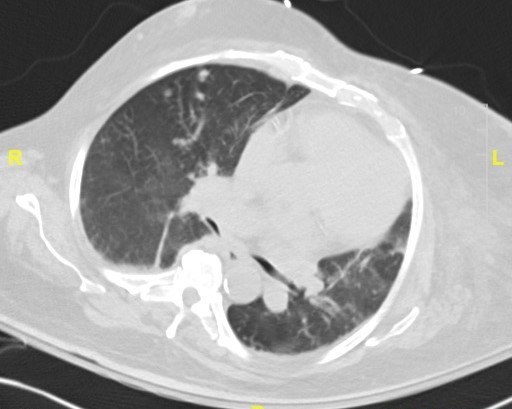
Figure: CT Chest showing Progressive bilateral solitary pulmonary nodules
Disclosures:
Joshika Agarwal indicated no relevant financial relationships.
Rabia Naseem indicated no relevant financial relationships.
Darsh Patel indicated no relevant financial relationships.
Dhruvan Patel indicated no relevant financial relationships.
Joshika Agarwal, MD, Rabia Naseem, MD, Darsh Tusharbhai. Patel, MD, Dhruvan Patel, MD. P1702 - NASH Cirrhosis, a Risk Factor for Disseminated Cryptococcus: Expanding the Non-HIV Spectrum, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
