Sunday Poster Session
Category: Liver
P1697 - Idiopathic HLH Presenting as Acute Liver Failure: A Challenging Diagnostic and Management Dilemma
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- MP
Manish Paranjpe, MD
Stanford University School of Medicine
Stanford, CA
Presenting Author(s)
Manish Paranjpe, MD1, Paul Kwo, MD2, Nikki Duong, MD3
1Stanford University School of Medicine, Stanford, CA; 2Stanford Health Care, Stanford, CA; 3Stanford University, Stanford, CA
Introduction: Hemophagocytic lymphohistiocytosis (HLH) is a cytokine-mediated hyperinflammatory syndrome often resulting in multiorgan failure and death. We present a rare case of idiopathic HLH resulting in acute liver failure, following an extensive etiologic workup.
Case Description/
Methods: A 25-year-old female with no significant past medical history developed abdominal pain, non-bloody diarrhea, fatigue, jaundice, right upper quadrant abdominal pain, and severely elevated liver enzymes following a trip to Mexico.
She then presented to our hospital with worsening fevers and abdominal pain. On admission, she was hypotensive, tachycardic and febrile. Labs showed anemia (Hgb 8.4g/dL), thrombocytopenia (platelets 119x109/L), elevated aminotransferases (AST 646 U/L, ALT 666 U/L, ALP 187 U/L), hyperbilirubinemia (total bilirubin 16 mg/dL), INR 2.4, hyperferritinemia (51,664 ng/mL), hypofibrinogenemia (162 mg/dL), elevated CXCL9 of 191,053 pg/mL and elevated soluble IL-2R 30,535 pg/mL (Table 1).
Liver biopsy demonstrated severe active hepatitis with extensive hepatocyte necrosis. Bone marrow biopsy revealed normocellular marrow with infrequent hemophagocytosis. Flow cytometry was immunophenotypically normal. Sequencing was negative for primary HLH mutations and hematologic malignancy mutations. Infectious and autoimmune workup was negative including blood cultures, dengue virus, Syphilis, adenovirus, parvovirus, C. diff,, leptospira, EBV, CMV, Influenza A/B, coccidioidomycosis, histoplasma, HSV, VZV, SARS-CoV-2 malaria, chikungunya, West Nile, HAV, HBV, HCV, HIV, ANCAs, rheumatoid factor, ASMA Ab, LKM Ab, AMA Ab.
She then developed rapidly progressive encephalopathy, worsening liver synthetic function and refractory shock, despite empiric broad-spectrum antibiotics, stress-dose steroids and ruxolitinib and anakinra for presumed HLH. An liver transplant evaluation was initiated, but she continued to worsen[pp1] , and was made comfort care. Autopsy revealed macrophage hemophagocytosis in the spleen.
Discussion: This case highlights the diagnostic challenges and rapid progression of idiopathic HLH presenting as ALF. Our patient met 6 out of 8 criteria for HLH, including bicytopenia, fever, hypofibrinogenemia, low NK cell activity, hemophagocytosis, elevated ferritin and elevated sIL-2R. A did not reveal an etiology. The lack of a clear trigger underscores the importance of the need for a high index of suspicion and prompt treatment since HLH can be life-threatening.
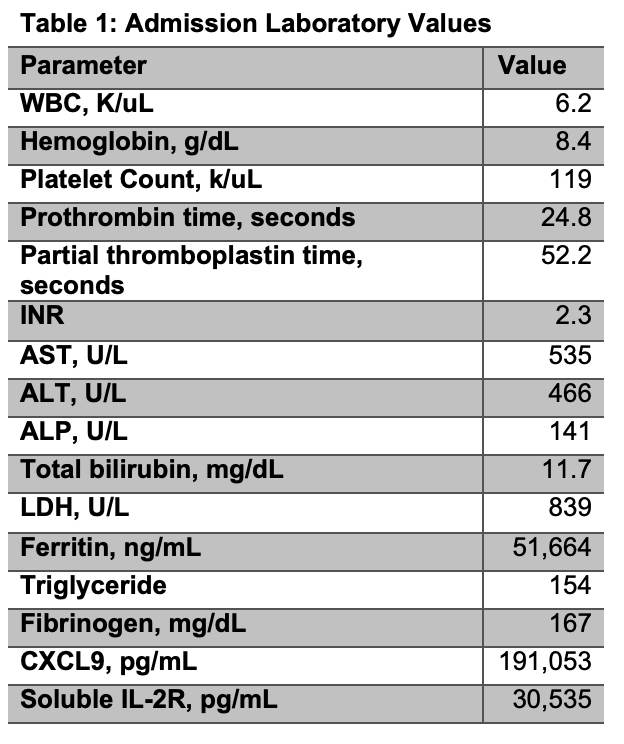
Figure: Table 1: Admission laboratory values
Disclosures:
Manish Paranjpe indicated no relevant financial relationships.
Paul Kwo: 89Bio – Grant/Research Support. Akero – Grant/Research Support. Aligos – Consultant. Arbutus – Consultant. Ausper Bio – Consultant, Grant/Research Support. Durect – Consultant, Stock Options. Gilead – Consultant, Grant/Research Support. Glaxo Smith Kline – Consultant. Inventiva – Consultant, Grant/Research Support. Madrigal – Grant/Research Support. Mallinckrodt – Consultant. Novo Nordisk – Consultant, Grant/Research Support. Precision Biosciences – Consultant. Salix – Consultant, Grant/Research Support. Takeda – Grant/Research Support. Tune Therapeutics – Consultant. Ultragenyx – Grant/Research Support.
Nikki Duong indicated no relevant financial relationships.
Manish Paranjpe, MD1, Paul Kwo, MD2, Nikki Duong, MD3. P1697 - Idiopathic HLH Presenting as Acute Liver Failure: A Challenging Diagnostic and Management Dilemma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Stanford University School of Medicine, Stanford, CA; 2Stanford Health Care, Stanford, CA; 3Stanford University, Stanford, CA
Introduction: Hemophagocytic lymphohistiocytosis (HLH) is a cytokine-mediated hyperinflammatory syndrome often resulting in multiorgan failure and death. We present a rare case of idiopathic HLH resulting in acute liver failure, following an extensive etiologic workup.
Case Description/
Methods: A 25-year-old female with no significant past medical history developed abdominal pain, non-bloody diarrhea, fatigue, jaundice, right upper quadrant abdominal pain, and severely elevated liver enzymes following a trip to Mexico.
She then presented to our hospital with worsening fevers and abdominal pain. On admission, she was hypotensive, tachycardic and febrile. Labs showed anemia (Hgb 8.4g/dL), thrombocytopenia (platelets 119x109/L), elevated aminotransferases (AST 646 U/L, ALT 666 U/L, ALP 187 U/L), hyperbilirubinemia (total bilirubin 16 mg/dL), INR 2.4, hyperferritinemia (51,664 ng/mL), hypofibrinogenemia (162 mg/dL), elevated CXCL9 of 191,053 pg/mL and elevated soluble IL-2R 30,535 pg/mL (Table 1).
Liver biopsy demonstrated severe active hepatitis with extensive hepatocyte necrosis. Bone marrow biopsy revealed normocellular marrow with infrequent hemophagocytosis. Flow cytometry was immunophenotypically normal. Sequencing was negative for primary HLH mutations and hematologic malignancy mutations. Infectious and autoimmune workup was negative including blood cultures, dengue virus, Syphilis, adenovirus, parvovirus, C. diff,, leptospira, EBV, CMV, Influenza A/B, coccidioidomycosis, histoplasma, HSV, VZV, SARS-CoV-2 malaria, chikungunya, West Nile, HAV, HBV, HCV, HIV, ANCAs, rheumatoid factor, ASMA Ab, LKM Ab, AMA Ab.
She then developed rapidly progressive encephalopathy, worsening liver synthetic function and refractory shock, despite empiric broad-spectrum antibiotics, stress-dose steroids and ruxolitinib and anakinra for presumed HLH. An liver transplant evaluation was initiated, but she continued to worsen[pp1] , and was made comfort care. Autopsy revealed macrophage hemophagocytosis in the spleen.
Discussion: This case highlights the diagnostic challenges and rapid progression of idiopathic HLH presenting as ALF. Our patient met 6 out of 8 criteria for HLH, including bicytopenia, fever, hypofibrinogenemia, low NK cell activity, hemophagocytosis, elevated ferritin and elevated sIL-2R. A did not reveal an etiology. The lack of a clear trigger underscores the importance of the need for a high index of suspicion and prompt treatment since HLH can be life-threatening.
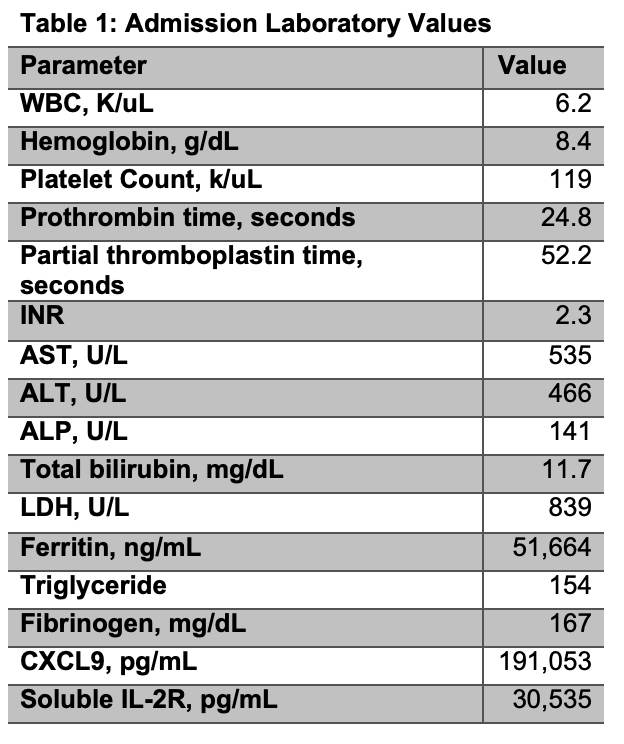
Figure: Table 1: Admission laboratory values
Disclosures:
Manish Paranjpe indicated no relevant financial relationships.
Paul Kwo: 89Bio – Grant/Research Support. Akero – Grant/Research Support. Aligos – Consultant. Arbutus – Consultant. Ausper Bio – Consultant, Grant/Research Support. Durect – Consultant, Stock Options. Gilead – Consultant, Grant/Research Support. Glaxo Smith Kline – Consultant. Inventiva – Consultant, Grant/Research Support. Madrigal – Grant/Research Support. Mallinckrodt – Consultant. Novo Nordisk – Consultant, Grant/Research Support. Precision Biosciences – Consultant. Salix – Consultant, Grant/Research Support. Takeda – Grant/Research Support. Tune Therapeutics – Consultant. Ultragenyx – Grant/Research Support.
Nikki Duong indicated no relevant financial relationships.
Manish Paranjpe, MD1, Paul Kwo, MD2, Nikki Duong, MD3. P1697 - Idiopathic HLH Presenting as Acute Liver Failure: A Challenging Diagnostic and Management Dilemma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
