Sunday Poster Session
Category: Liver
P1689 - Hepatitis E Virus: An Unexpected Culprit of Extreme Hyperferritinemia
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Ghattas Malki, MD
David Geffen School of Medicine at UCLA
Los Angeles, CA
Presenting Author(s)
Award: ACG Presidential Poster Award
Ghattas Malki, MD1, Jeemin Kwon, MD1, Hongying Tan, MD, PhD2, Shaun Chandna, DO2
1David Geffen School of Medicine at UCLA, Los Angeles, CA; 2Olive View-UCLA Medical Center, Los Angeles, CA
Introduction: Extreme hyperferritinemia refers to severely elevated serum ferritin levels, typically above 10,000 ng/mL. This indicator of severe systemic inflammation and critical illness is associated with high rates of morbidity and mortality. Differential includes hemophagocytic lymphohistiocytosis (HLH), macrophage activation syndrome, Still’s disease, infection and malignancy. We present a case of extreme hyperferritinemia due to acute hepatitis E virus (HEV)-induced acute liver injury.
Case Description/
Methods: 55-year-old female with gastric ulcer history, visiting from Nigeria, admitted with 3 days of nausea, dark emesis, poor intake and subjective fevers. Labs revealed WBC 14.9K/µL, Hb 10.7 g/dL, Plt 220K/µL, BUN 42 mg/dL, Cr 1.21 mg/dL, lactate 6.8 mmol/L, and acute liver injury (AST >4440 U/L, ALT 3440 U/L, total bilirubin 19.3 mg/dL, INR 1.65). No encephalopathy was present. Serum ferritin exceeded 40,000 ng/mL. Haptoglobin < 15 mg/dL. LDH 2126 U/L. CT abdomen/pelvis revealed a tiny calcification and small hypodensity in the liver. Liver ultrasound was negative. Serologic work up was negative other than mild IgG elevation, H63D carrier, and prior exposures (HbcAb total, EBV IgG, CMV IgG). Respiratory virus panel and Bartonella negative. Hemoglobin H variant present, otherwise smear, direct antibody, G6PD, flow cytometry, PNH testing negative. Suspicion for HLH was low; triglycerides 197 mg/dL and soluble IL-2 receptor antibody (sIL-2Rα) sent. Liver biopsy was obtained. Liver tests, INR, and ferritin were improving upon discharge. Resulting labs revealed sIL-2Rα mild elevation (2124 pg/mL), Dengue IgG+, HSV2 DNA low positive, leptospira and alpha thalassemia negative, and positive Hepatitis E IgM and IgG serologies. Liver biopsy showed acute hepatitis compatible with HEV infection.
Discussion: Severe hyperferritinemia is associated with a narrow spectrum of conditions, often from HLH, though acute liver disease (acute hepatitis, liver injury, liver failure) is another known cause. Though acute hepatitis can be associated with hyperferritinemia >100K, to our knowledge, this is the first reported case specific to HEV of acute HEV-induced acute liver injury with ferritin levels exceeding 40,000 ng/mL. While there have been reports of HEV-induced HLH, our patient did not meet HLH diagnostic criteria. This case underscores the need for a broadened workup in patients to include HEV, particularly in travelers from sub-Saharan Africa and Asia, presenting with acute hepatitis and extreme hyperferritinemia.
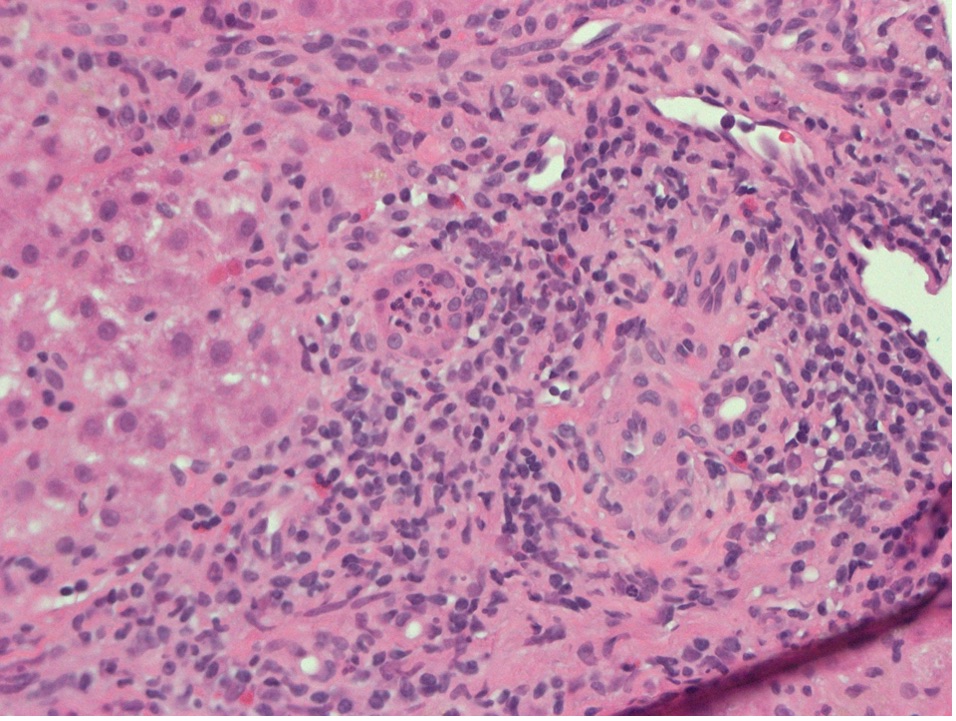
Figure: Hematoxylin and Eosin stain of liver biopsy. Portal zone with mild lymphocytic infiltrates with occasional plasma cells, eosinophils and neutrophils. Interphase activity is present. Focal neutrophilic accumulation in the lumen of a ductule is noted. Bile ducts are present. Original magnifications x400.
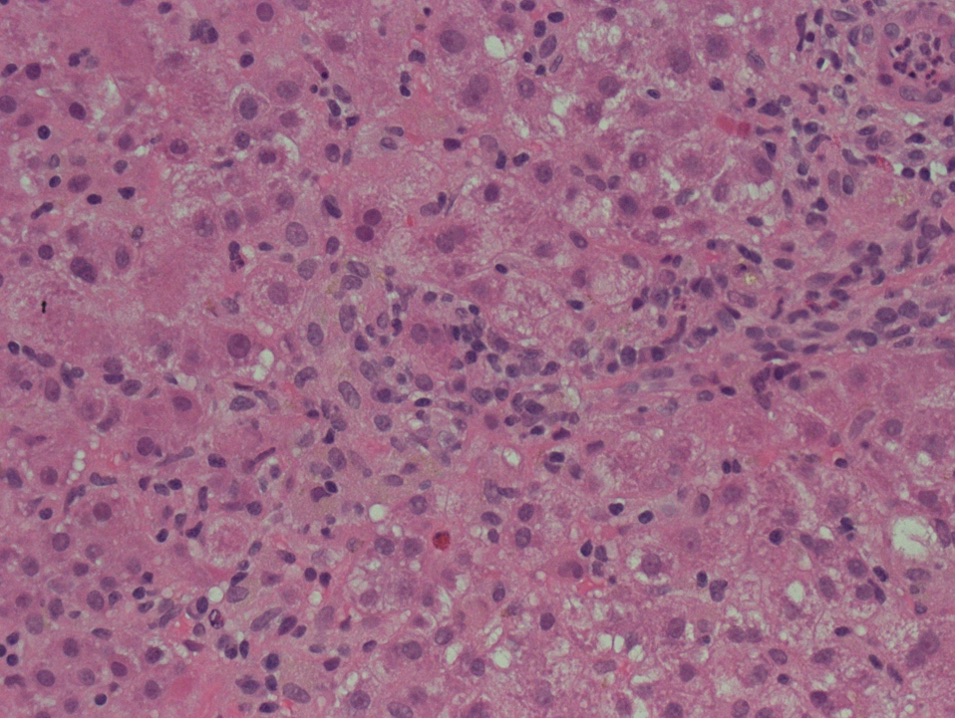
Figure: Hematoxylin and Eosin stain of liver biopsy showing hepatocyte swelling and lymphocytic infiltration of lobules with occasional plasma cells and rare eosinophils. Focal cytoplasmic cholestasis is noted. Original magnifications x400
Disclosures:
Ghattas Malki indicated no relevant financial relationships.
Jeemin Kwon indicated no relevant financial relationships.
Hongying Tan indicated no relevant financial relationships.
Shaun Chandna: Arrowhead Pharmaceuticals – Grant/Research Support. Calliditas Therapeutics (formerly Genkyotex) – Grant/Research Support. Ipsen – Consultant. Lipocine – Grant/Research Support. Mirum Pharmaceuticals – Consultant, Grant/Research Support.
Ghattas Malki, MD1, Jeemin Kwon, MD1, Hongying Tan, MD, PhD2, Shaun Chandna, DO2. P1689 - Hepatitis E Virus: An Unexpected Culprit of Extreme Hyperferritinemia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Ghattas Malki, MD1, Jeemin Kwon, MD1, Hongying Tan, MD, PhD2, Shaun Chandna, DO2
1David Geffen School of Medicine at UCLA, Los Angeles, CA; 2Olive View-UCLA Medical Center, Los Angeles, CA
Introduction: Extreme hyperferritinemia refers to severely elevated serum ferritin levels, typically above 10,000 ng/mL. This indicator of severe systemic inflammation and critical illness is associated with high rates of morbidity and mortality. Differential includes hemophagocytic lymphohistiocytosis (HLH), macrophage activation syndrome, Still’s disease, infection and malignancy. We present a case of extreme hyperferritinemia due to acute hepatitis E virus (HEV)-induced acute liver injury.
Case Description/
Methods: 55-year-old female with gastric ulcer history, visiting from Nigeria, admitted with 3 days of nausea, dark emesis, poor intake and subjective fevers. Labs revealed WBC 14.9K/µL, Hb 10.7 g/dL, Plt 220K/µL, BUN 42 mg/dL, Cr 1.21 mg/dL, lactate 6.8 mmol/L, and acute liver injury (AST >4440 U/L, ALT 3440 U/L, total bilirubin 19.3 mg/dL, INR 1.65). No encephalopathy was present. Serum ferritin exceeded 40,000 ng/mL. Haptoglobin < 15 mg/dL. LDH 2126 U/L. CT abdomen/pelvis revealed a tiny calcification and small hypodensity in the liver. Liver ultrasound was negative. Serologic work up was negative other than mild IgG elevation, H63D carrier, and prior exposures (HbcAb total, EBV IgG, CMV IgG). Respiratory virus panel and Bartonella negative. Hemoglobin H variant present, otherwise smear, direct antibody, G6PD, flow cytometry, PNH testing negative. Suspicion for HLH was low; triglycerides 197 mg/dL and soluble IL-2 receptor antibody (sIL-2Rα) sent. Liver biopsy was obtained. Liver tests, INR, and ferritin were improving upon discharge. Resulting labs revealed sIL-2Rα mild elevation (2124 pg/mL), Dengue IgG+, HSV2 DNA low positive, leptospira and alpha thalassemia negative, and positive Hepatitis E IgM and IgG serologies. Liver biopsy showed acute hepatitis compatible with HEV infection.
Discussion: Severe hyperferritinemia is associated with a narrow spectrum of conditions, often from HLH, though acute liver disease (acute hepatitis, liver injury, liver failure) is another known cause. Though acute hepatitis can be associated with hyperferritinemia >100K, to our knowledge, this is the first reported case specific to HEV of acute HEV-induced acute liver injury with ferritin levels exceeding 40,000 ng/mL. While there have been reports of HEV-induced HLH, our patient did not meet HLH diagnostic criteria. This case underscores the need for a broadened workup in patients to include HEV, particularly in travelers from sub-Saharan Africa and Asia, presenting with acute hepatitis and extreme hyperferritinemia.
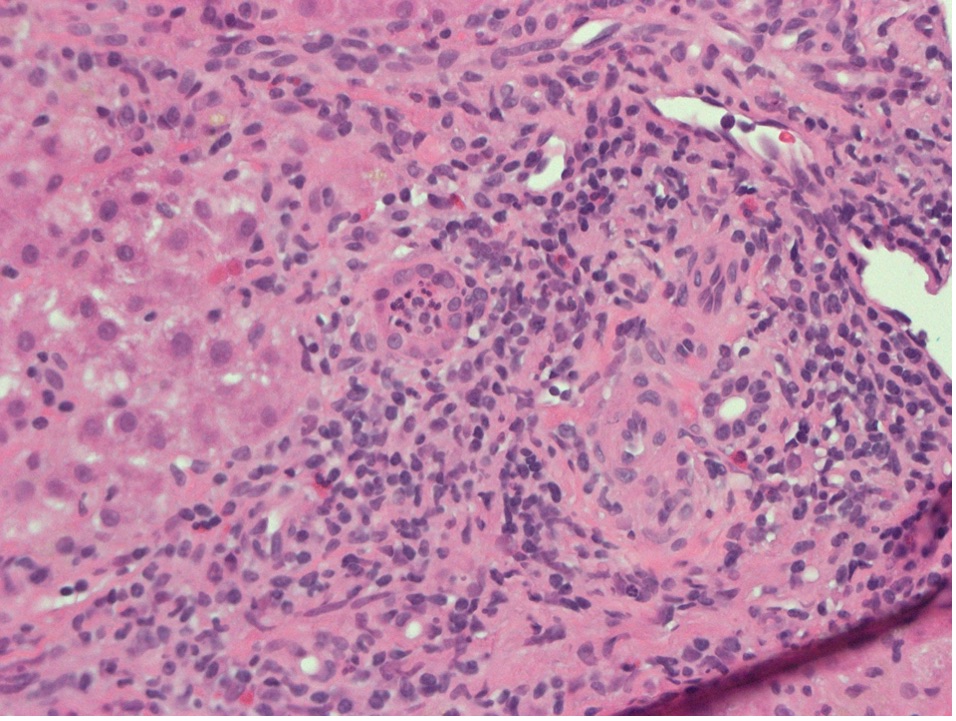
Figure: Hematoxylin and Eosin stain of liver biopsy. Portal zone with mild lymphocytic infiltrates with occasional plasma cells, eosinophils and neutrophils. Interphase activity is present. Focal neutrophilic accumulation in the lumen of a ductule is noted. Bile ducts are present. Original magnifications x400.
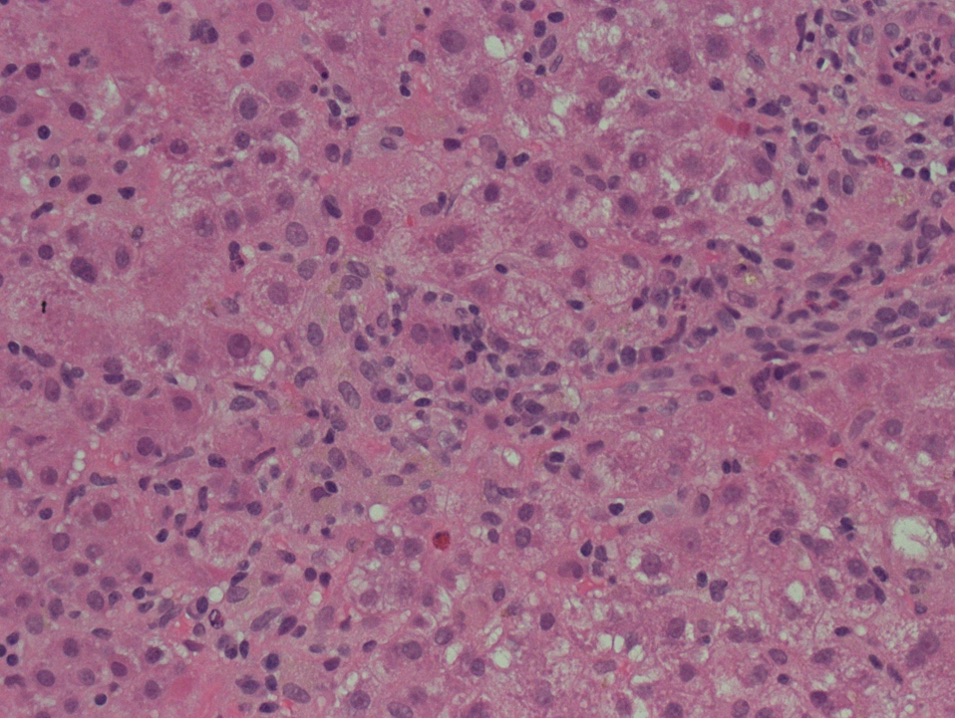
Figure: Hematoxylin and Eosin stain of liver biopsy showing hepatocyte swelling and lymphocytic infiltration of lobules with occasional plasma cells and rare eosinophils. Focal cytoplasmic cholestasis is noted. Original magnifications x400
Disclosures:
Ghattas Malki indicated no relevant financial relationships.
Jeemin Kwon indicated no relevant financial relationships.
Hongying Tan indicated no relevant financial relationships.
Shaun Chandna: Arrowhead Pharmaceuticals – Grant/Research Support. Calliditas Therapeutics (formerly Genkyotex) – Grant/Research Support. Ipsen – Consultant. Lipocine – Grant/Research Support. Mirum Pharmaceuticals – Consultant, Grant/Research Support.
Ghattas Malki, MD1, Jeemin Kwon, MD1, Hongying Tan, MD, PhD2, Shaun Chandna, DO2. P1689 - Hepatitis E Virus: An Unexpected Culprit of Extreme Hyperferritinemia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

