Sunday Poster Session
Category: Liver
P1678 - Improving Care Pathways for Ascites: A Process Improvement Initiative to Reduce Short-Stay Admissions for Therapeutic Paracentesis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- JC
John Cooper, MD
University of Alabama at Birmingham Heersink School of Medicine
Birmingham, AL
Presenting Author(s)
Malcolm B. Chapman, MD, MBA1, John Cooper, MD1, Crystal Knox, MSN, RN2, Kyndal McKnight, MD1, Laine McDonald, MD1, Lauren Epp, CRNP1, Paige Culp, BSN1, Benjamin von Schweinitz, MD1, James Crosby, MD1, Molly Miller, PA-C1, Sujan Ravi, MD, MPH3
1University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL; 2University of Alabama at Birmingham Hospital, Birmingham, AL; 3Basil I. Hirschowitz Endoscopic Center of Excellence, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL
Introduction: Patients with ascites are often admitted for inpatient care to undergo therapeutic paracentesis. While many present with other problems that necessitate acute care, a subset are otherwise stable for outpatient management. Hospitalization solely for paracentesis strains limited inpatient resources. Furthermore, it is important to address underlying drivers leading patients to seek care in the emergency department (ED).
We launched a multidisciplinary quality improvement collaborative to identify stable patients with ascites presenting to the ED and redirect them to same-day or next-day outpatient paracentesis. We also aimed to establish timely outpatient follow-up to prevent avoidable return visits to the ED.
Methods: The electronic health record was queried for hospital admissions 48 hours or less in duration during which a paracentesis was performed. A multidisciplinary team was formed from representatives of emergency medicine, hepatology, inpatient procedure team, radiology, outpatient paracentesis clinic, ambulatory intermediate care clinic, and post-discharge clinic. We used the Plan-Do-Study-Act methodology to guide our intervention. A clinical pathway (Figure 1) was created to coordinate same-day or next-day paracentesis after ED discharge. Patients deemed stable who did not warrant admission for other reasons were routed to radiology for outpatient paracentesis. Afterward, radiology providers communicated with the outpatient paracentesis clinic and hepatology team to establish follow-up.
Results: Prior to implementation of the clinical pathway, an average of 9.5 patients monthly were admitted for less than 48 hours and underwent paracentesis from November 2023 to 2024. Post-implementation, this decreased to 5.6 patients monthly, a 41% reduction in short stay admissions (Figure 2). A total of 12 patients (average 2.4 monthly) followed the clinical pathway. Of these, 10 had cirrhosis and 12 were set up for hepatology and outpatient paracentesis clinic follow-up within one month of their ED visit.
Discussion: This multidisciplinary collaborative demonstrates a successful model for reducing short-stay admissions for ascites by transitioning appropriate care to the outpatient setting. This approach enabled a shared understanding of diverse clinical perspectives and facilitated both post-ED paracentesis and effective linkage to follow-up care. This model could be validated through implementation at other institutions and has the potential to improve health care utilization.
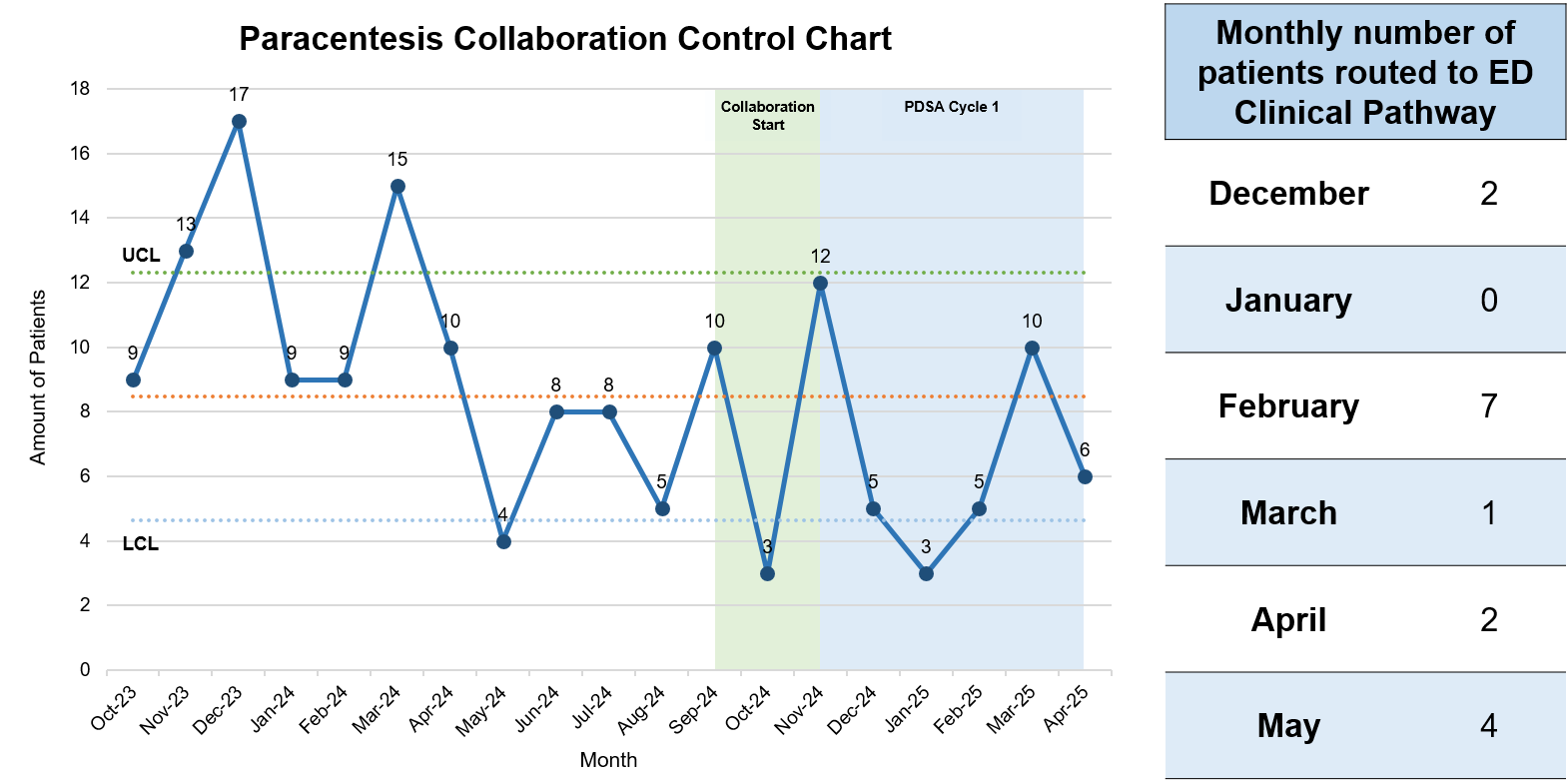
Figure: Streamlined clinical pathway for ED-initiated paracentesis in patients with ascites. Care flows from emergency department (ED) for timing and eligibility to NP Radiology for procedural execution to Ambulatory Infusion Care Clinic (AICC) for albumin administration, as needed, culminating with Hepatology or Post-Discharge Clinic (PDC) for appropriate referrals and specialty care.
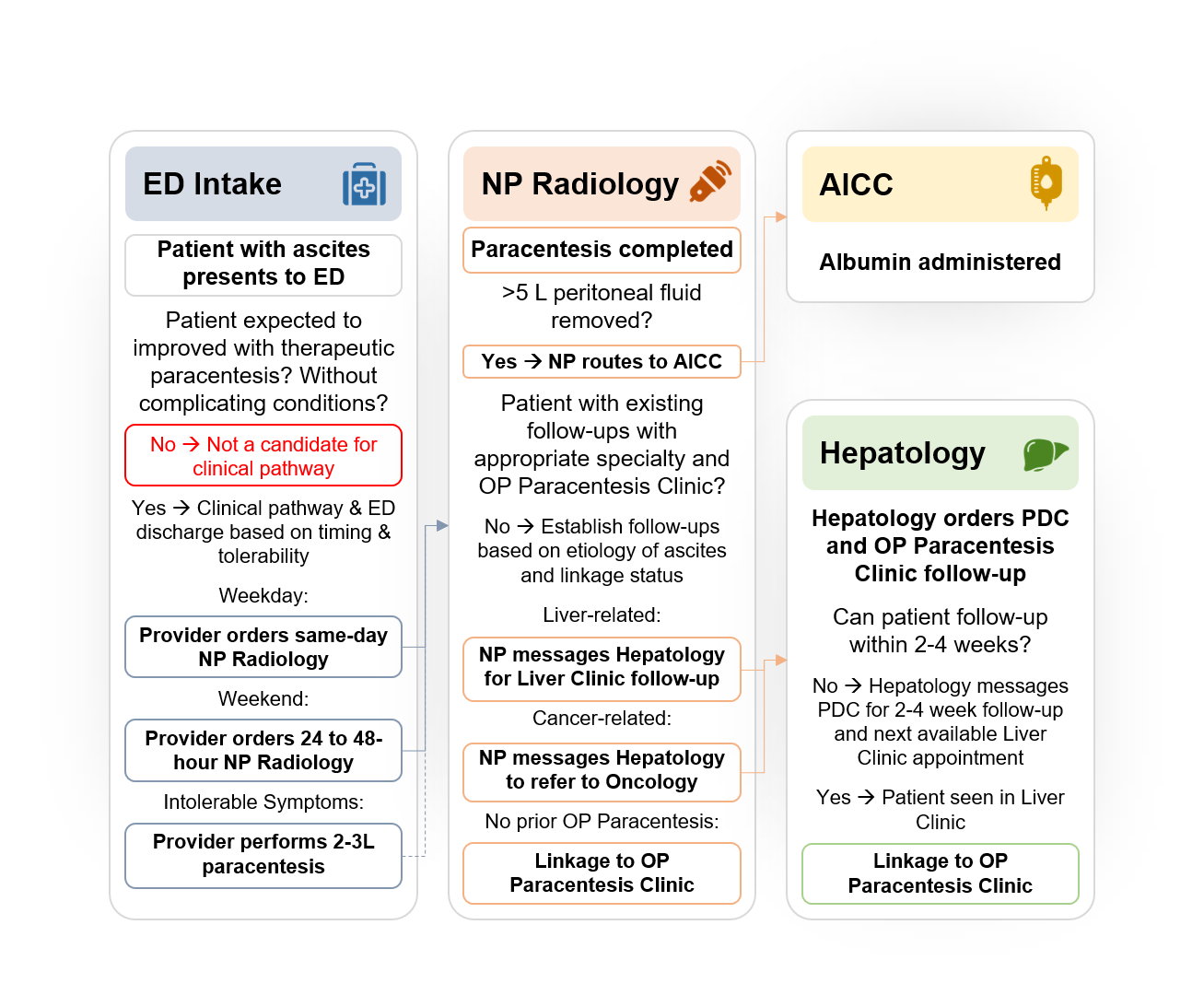
Figure: Paracentesis collaboration clinical pathway control chart and uptake table illustrating high monthly variability pre-collaboration, followed by reduced variability after pathway implementation and PDSA Cycle 1 with limited patient uptake.
Disclosures:
Malcolm Chapman indicated no relevant financial relationships.
John Cooper indicated no relevant financial relationships.
Crystal Knox indicated no relevant financial relationships.
Kyndal McKnight indicated no relevant financial relationships.
Laine McDonald indicated no relevant financial relationships.
Lauren Epp indicated no relevant financial relationships.
Paige Culp indicated no relevant financial relationships.
Benjamin von Schweinitz indicated no relevant financial relationships.
James Crosby indicated no relevant financial relationships.
Molly Miller indicated no relevant financial relationships.
Sujan Ravi indicated no relevant financial relationships.
Malcolm B. Chapman, MD, MBA1, John Cooper, MD1, Crystal Knox, MSN, RN2, Kyndal McKnight, MD1, Laine McDonald, MD1, Lauren Epp, CRNP1, Paige Culp, BSN1, Benjamin von Schweinitz, MD1, James Crosby, MD1, Molly Miller, PA-C1, Sujan Ravi, MD, MPH3. P1678 - Improving Care Pathways for Ascites: A Process Improvement Initiative to Reduce Short-Stay Admissions for Therapeutic Paracentesis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL; 2University of Alabama at Birmingham Hospital, Birmingham, AL; 3Basil I. Hirschowitz Endoscopic Center of Excellence, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL
Introduction: Patients with ascites are often admitted for inpatient care to undergo therapeutic paracentesis. While many present with other problems that necessitate acute care, a subset are otherwise stable for outpatient management. Hospitalization solely for paracentesis strains limited inpatient resources. Furthermore, it is important to address underlying drivers leading patients to seek care in the emergency department (ED).
We launched a multidisciplinary quality improvement collaborative to identify stable patients with ascites presenting to the ED and redirect them to same-day or next-day outpatient paracentesis. We also aimed to establish timely outpatient follow-up to prevent avoidable return visits to the ED.
Methods: The electronic health record was queried for hospital admissions 48 hours or less in duration during which a paracentesis was performed. A multidisciplinary team was formed from representatives of emergency medicine, hepatology, inpatient procedure team, radiology, outpatient paracentesis clinic, ambulatory intermediate care clinic, and post-discharge clinic. We used the Plan-Do-Study-Act methodology to guide our intervention. A clinical pathway (Figure 1) was created to coordinate same-day or next-day paracentesis after ED discharge. Patients deemed stable who did not warrant admission for other reasons were routed to radiology for outpatient paracentesis. Afterward, radiology providers communicated with the outpatient paracentesis clinic and hepatology team to establish follow-up.
Results: Prior to implementation of the clinical pathway, an average of 9.5 patients monthly were admitted for less than 48 hours and underwent paracentesis from November 2023 to 2024. Post-implementation, this decreased to 5.6 patients monthly, a 41% reduction in short stay admissions (Figure 2). A total of 12 patients (average 2.4 monthly) followed the clinical pathway. Of these, 10 had cirrhosis and 12 were set up for hepatology and outpatient paracentesis clinic follow-up within one month of their ED visit.
Discussion: This multidisciplinary collaborative demonstrates a successful model for reducing short-stay admissions for ascites by transitioning appropriate care to the outpatient setting. This approach enabled a shared understanding of diverse clinical perspectives and facilitated both post-ED paracentesis and effective linkage to follow-up care. This model could be validated through implementation at other institutions and has the potential to improve health care utilization.
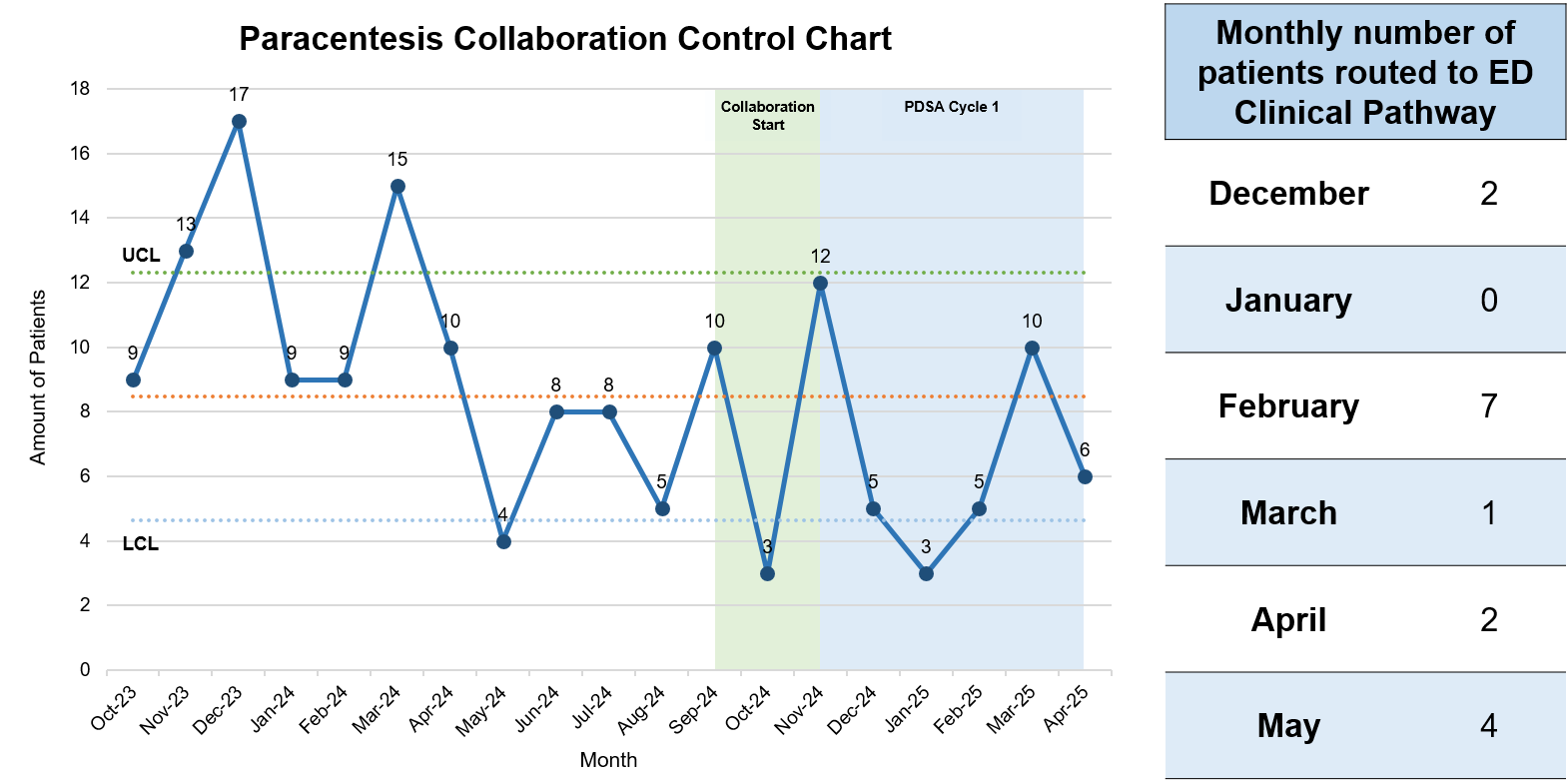
Figure: Streamlined clinical pathway for ED-initiated paracentesis in patients with ascites. Care flows from emergency department (ED) for timing and eligibility to NP Radiology for procedural execution to Ambulatory Infusion Care Clinic (AICC) for albumin administration, as needed, culminating with Hepatology or Post-Discharge Clinic (PDC) for appropriate referrals and specialty care.
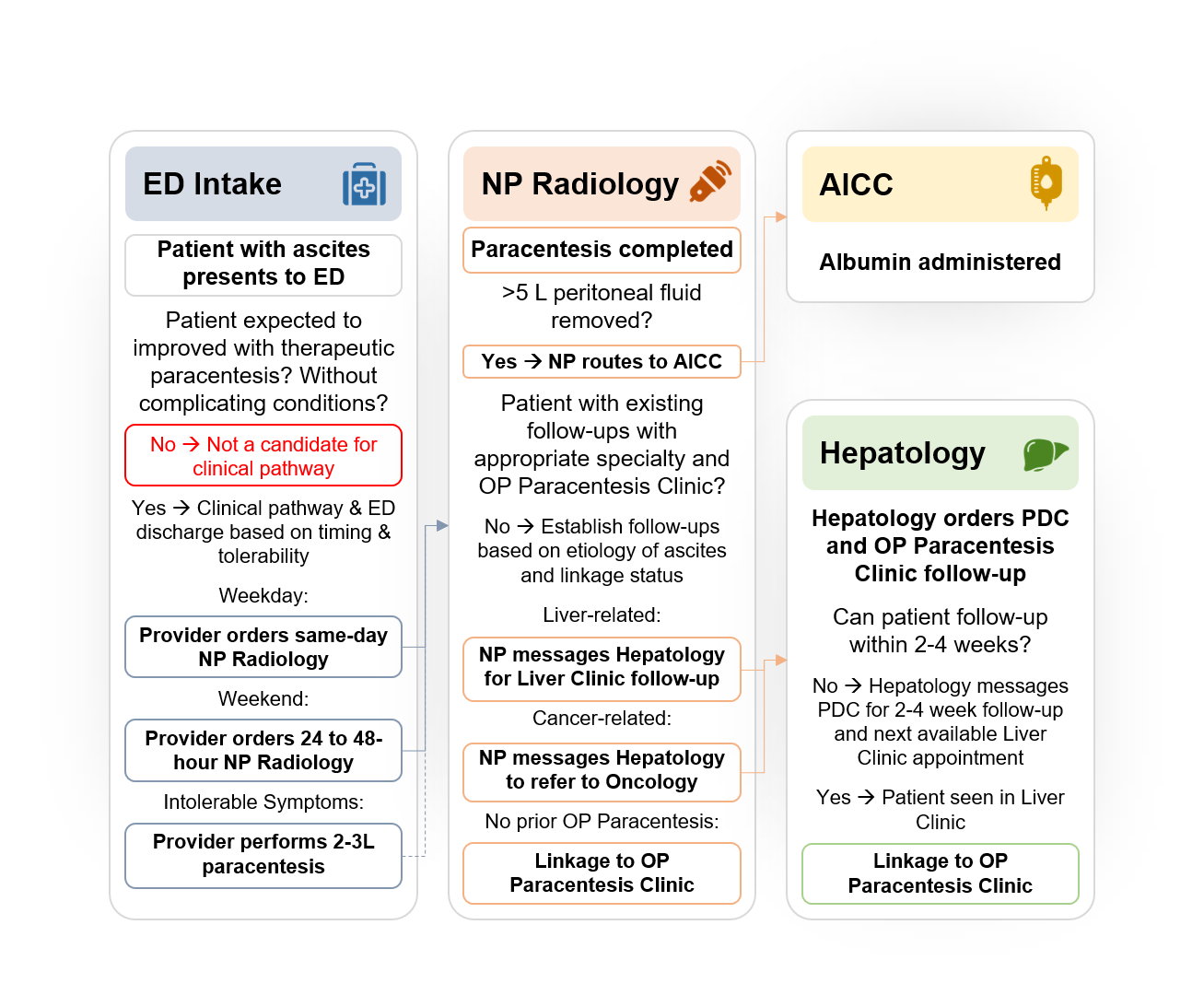
Figure: Paracentesis collaboration clinical pathway control chart and uptake table illustrating high monthly variability pre-collaboration, followed by reduced variability after pathway implementation and PDSA Cycle 1 with limited patient uptake.
Disclosures:
Malcolm Chapman indicated no relevant financial relationships.
John Cooper indicated no relevant financial relationships.
Crystal Knox indicated no relevant financial relationships.
Kyndal McKnight indicated no relevant financial relationships.
Laine McDonald indicated no relevant financial relationships.
Lauren Epp indicated no relevant financial relationships.
Paige Culp indicated no relevant financial relationships.
Benjamin von Schweinitz indicated no relevant financial relationships.
James Crosby indicated no relevant financial relationships.
Molly Miller indicated no relevant financial relationships.
Sujan Ravi indicated no relevant financial relationships.
Malcolm B. Chapman, MD, MBA1, John Cooper, MD1, Crystal Knox, MSN, RN2, Kyndal McKnight, MD1, Laine McDonald, MD1, Lauren Epp, CRNP1, Paige Culp, BSN1, Benjamin von Schweinitz, MD1, James Crosby, MD1, Molly Miller, PA-C1, Sujan Ravi, MD, MPH3. P1678 - Improving Care Pathways for Ascites: A Process Improvement Initiative to Reduce Short-Stay Admissions for Therapeutic Paracentesis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
