Sunday Poster Session
Category: Liver
P1677 - Obesity and Its Association With Clinical Outcomes and Readmissions After TIPS: A Propensity Matched Analysis Using Nationwide Readmissions Database 2017-2021
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- MK
Maulik Kaneriya, MD
One Brooklyn Health-Interfaith Medical Center
Brooklyn, NY
Presenting Author(s)
Maulik Kaneriya, MD1, Madhav Changela, MD1, Janak Bahirwani, MD2, Nishit Patel, MD3, Krishna Bodrya, MD4, Sanket Basida, MD5, Yecheskel Schneider, MD, MS6
1One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 2Kadlec Regional Medical Center, Richland, WA; 3St. Luke's University Health Network, Bethlehem, PA; 4Leigh Valley Health Network, Easton, PA; 5University of Missouri School of Medicine, Columbia, MO; 6Virtua Health System, Moorestown, NJ
Introduction: Transjugular Intrahepatic Portosystemic Shunt (TIPS) is a minimally invasive procedure used to relieve portal hypertension in patients with decompensated liver cirrhosis. Obesity may influence procedural risk and outcomes after TIPS placement, but large-scale data are lacking. We assessed the impact of obesity on in-hospital mortality, 30-day readmission, and clinical complications following TIPS.
Methods: This is a retrospective analysis using data from the National Readmission Database for the years 2017-2021. We included all the patients aged over 18 years who underwent TIPS, stratified based on obesity. Primary outcomes included mortality and all-cause 30-day readmissions. Secondary outcomes included length of stay, total hospitalization charges, sepsis, acute kidney injury(AKI), shock, post-procedural hemorrhage, and hepatic encephalopathy. Univariate and Multivariate regression analyses were used to evaluate the outcomes among two cohorts. To further address confounding propensity scores were estimated by incorporating age, gender, charlson comorbidity index(CCI), hospital bed-size, teaching status and median income, after which the outcomes were analyzed. P value < 0.05 was considered statistically significant.
Results: A total of 29,334 patients underwent TIPS, among whom 4,858 (16.6%) were obese. Additional demographic characteristics are summarized in Table 1. There was no significant difference in mortality between the two groups. All-cause readmissions was higher in the obese cohort compared to the control. All other outcomes were insignificant between two groups except shock, which was associated with being lower in the obese cohort compared to control. Post-TIPS, obese cohort was more likely to be discharged to a skilled nursing facility compared to controls. Statistically significant independent predictors of 30-day all-cause readmissions following TIPS included advanced age, a high CCI, admission to a metropolitan teaching hospital, shock, and AKI.
Discussion: Our study found that obesity and TIPS was associated with lower odds of shock and higher odds of all-cause readmissions compared to controls. Obese patients were more likely to be discharged to a skilled nursing facility compared to non-obese patients. These findings highlight the potential need for enhanced discharge planning and post-discharge support strategies in obese patients undergoing TIPS. Future research should explore the role of obesity severity and tailored interventions to reduce readmissions.
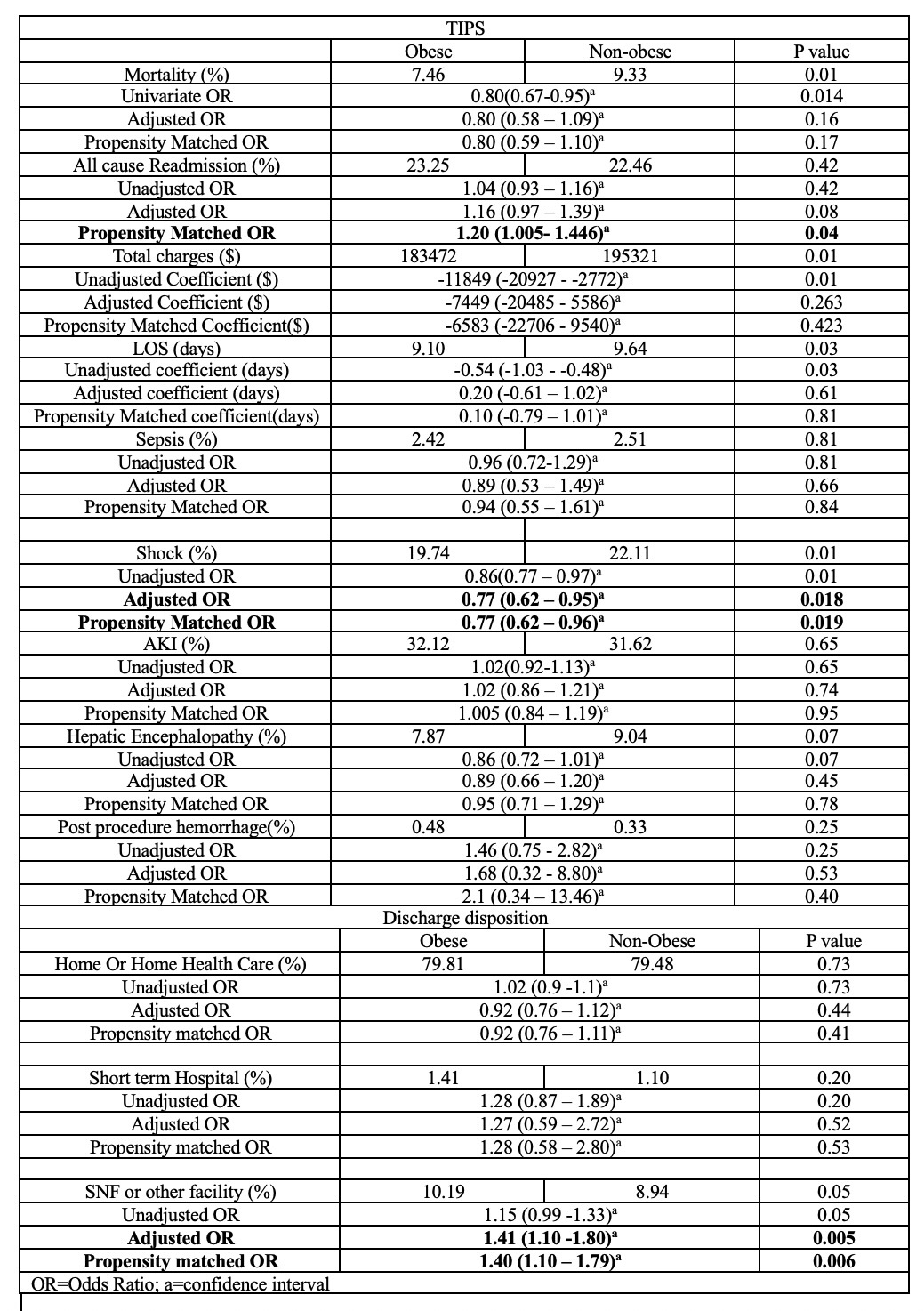
Figure: Table 1: Patient demographics and Predictors of all cause 30-day readmission
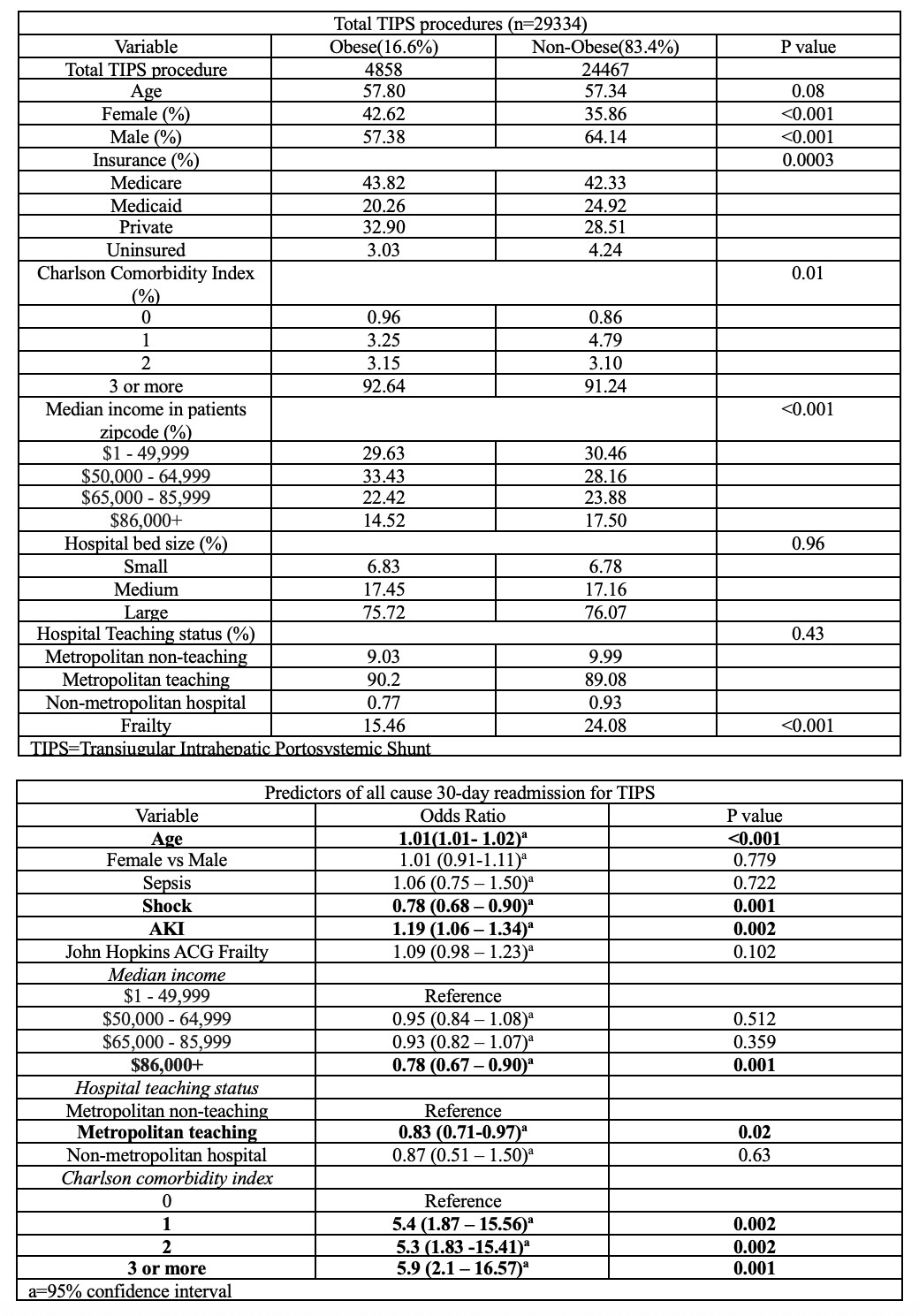
Figure: Table 2: Clinical outcomes and discharge disposition post TIPS procedure.
Disclosures:
Maulik Kaneriya indicated no relevant financial relationships.
Madhav Changela indicated no relevant financial relationships.
Janak Bahirwani indicated no relevant financial relationships.
Nishit Patel indicated no relevant financial relationships.
Krishna Bodrya indicated no relevant financial relationships.
Sanket Basida indicated no relevant financial relationships.
Yecheskel Schneider indicated no relevant financial relationships.
Maulik Kaneriya, MD1, Madhav Changela, MD1, Janak Bahirwani, MD2, Nishit Patel, MD3, Krishna Bodrya, MD4, Sanket Basida, MD5, Yecheskel Schneider, MD, MS6. P1677 - Obesity and Its Association With Clinical Outcomes and Readmissions After TIPS: A Propensity Matched Analysis Using Nationwide Readmissions Database 2017-2021, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 2Kadlec Regional Medical Center, Richland, WA; 3St. Luke's University Health Network, Bethlehem, PA; 4Leigh Valley Health Network, Easton, PA; 5University of Missouri School of Medicine, Columbia, MO; 6Virtua Health System, Moorestown, NJ
Introduction: Transjugular Intrahepatic Portosystemic Shunt (TIPS) is a minimally invasive procedure used to relieve portal hypertension in patients with decompensated liver cirrhosis. Obesity may influence procedural risk and outcomes after TIPS placement, but large-scale data are lacking. We assessed the impact of obesity on in-hospital mortality, 30-day readmission, and clinical complications following TIPS.
Methods: This is a retrospective analysis using data from the National Readmission Database for the years 2017-2021. We included all the patients aged over 18 years who underwent TIPS, stratified based on obesity. Primary outcomes included mortality and all-cause 30-day readmissions. Secondary outcomes included length of stay, total hospitalization charges, sepsis, acute kidney injury(AKI), shock, post-procedural hemorrhage, and hepatic encephalopathy. Univariate and Multivariate regression analyses were used to evaluate the outcomes among two cohorts. To further address confounding propensity scores were estimated by incorporating age, gender, charlson comorbidity index(CCI), hospital bed-size, teaching status and median income, after which the outcomes were analyzed. P value < 0.05 was considered statistically significant.
Results: A total of 29,334 patients underwent TIPS, among whom 4,858 (16.6%) were obese. Additional demographic characteristics are summarized in Table 1. There was no significant difference in mortality between the two groups. All-cause readmissions was higher in the obese cohort compared to the control. All other outcomes were insignificant between two groups except shock, which was associated with being lower in the obese cohort compared to control. Post-TIPS, obese cohort was more likely to be discharged to a skilled nursing facility compared to controls. Statistically significant independent predictors of 30-day all-cause readmissions following TIPS included advanced age, a high CCI, admission to a metropolitan teaching hospital, shock, and AKI.
Discussion: Our study found that obesity and TIPS was associated with lower odds of shock and higher odds of all-cause readmissions compared to controls. Obese patients were more likely to be discharged to a skilled nursing facility compared to non-obese patients. These findings highlight the potential need for enhanced discharge planning and post-discharge support strategies in obese patients undergoing TIPS. Future research should explore the role of obesity severity and tailored interventions to reduce readmissions.
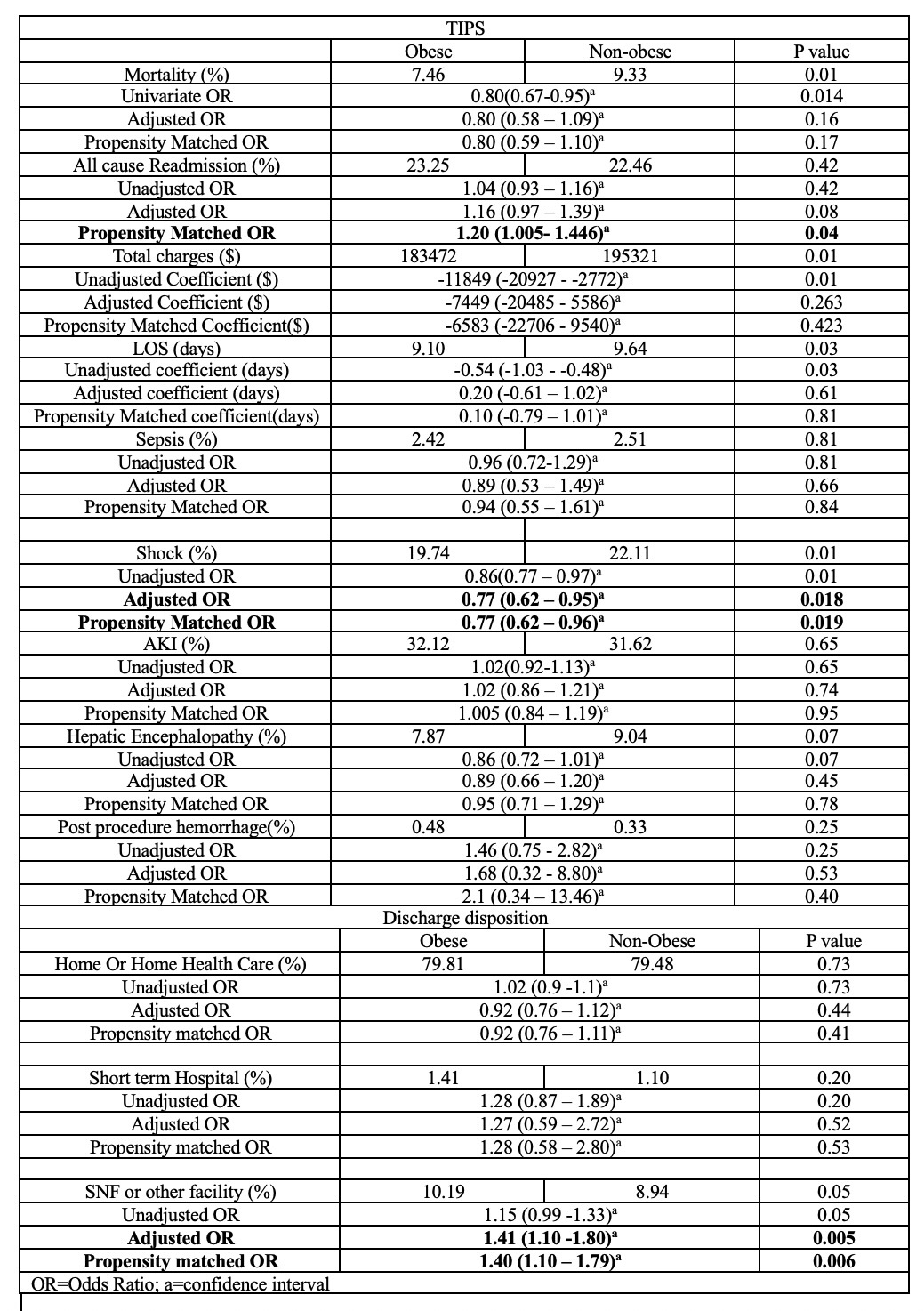
Figure: Table 1: Patient demographics and Predictors of all cause 30-day readmission
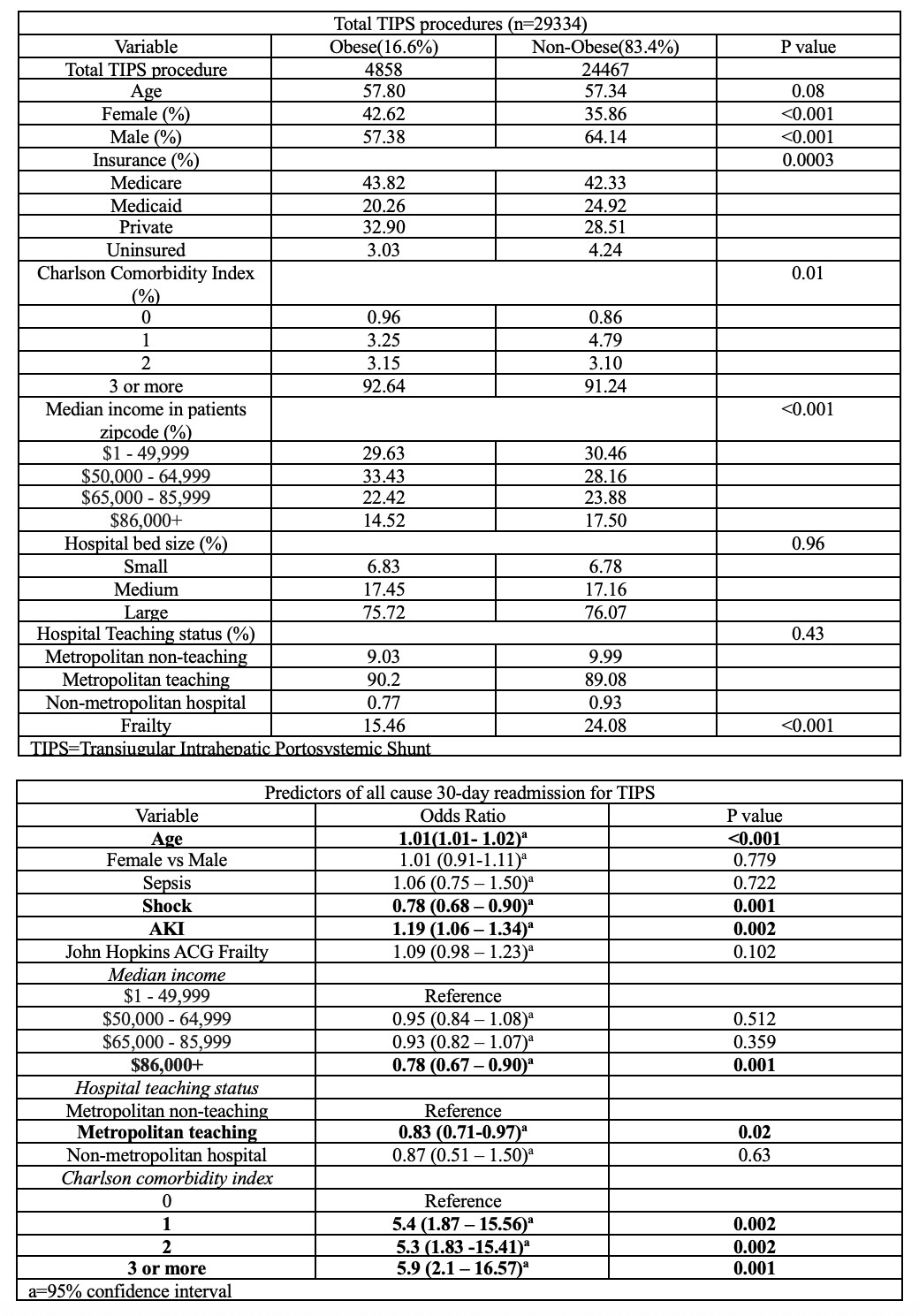
Figure: Table 2: Clinical outcomes and discharge disposition post TIPS procedure.
Disclosures:
Maulik Kaneriya indicated no relevant financial relationships.
Madhav Changela indicated no relevant financial relationships.
Janak Bahirwani indicated no relevant financial relationships.
Nishit Patel indicated no relevant financial relationships.
Krishna Bodrya indicated no relevant financial relationships.
Sanket Basida indicated no relevant financial relationships.
Yecheskel Schneider indicated no relevant financial relationships.
Maulik Kaneriya, MD1, Madhav Changela, MD1, Janak Bahirwani, MD2, Nishit Patel, MD3, Krishna Bodrya, MD4, Sanket Basida, MD5, Yecheskel Schneider, MD, MS6. P1677 - Obesity and Its Association With Clinical Outcomes and Readmissions After TIPS: A Propensity Matched Analysis Using Nationwide Readmissions Database 2017-2021, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
