Sunday Poster Session
Category: Liver
P1675 - Validation of S-WAVE Elasticity and ACE Attenuation Against MRE and MRI-PDFF in Patients with Clinically Diagnosed MASLD or MASH
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- RH
Reed B. Hogan, II, MD
GI Associates & Endoscopy Center: Flowood
Jackson, MS
Presenting Author(s)
Sri Naveen Surapaneni, MD, MPH1, Reed Hogan, MD2, Tessa Mury, MPH3, Ashley Horton, BS3, Dominique Claiborne, 4, Caitlin Schneider, PhD4
1Texas Digestive Disease Consultants/ GI Alliance, Houston, TX; 2GI Associates & Endoscopy Center: Flowood, Flowood, MS; 3Texas Digestive Disease Consultants, Webster, TX; 4Sonic Incytes Medical Corp, Vancouver, BC, Canada
Introduction: Non-invasive tools for liver assessment are increasingly becoming standard of care for screening, diagnosing and monitoring patients with MASLD and MASH. New guidance recommends that imaging tools be used in assessing clinics for assessing patients and determining eligibility for new treatments. Shear wave absolute vibro-elasticity (S-WAVE) and Attenuation Coefficient Estimate (ACE), available on Velacur devices represent a new point-of-care imaging of stiffness and estimates of liver fat based on quantitative ultrasound parameters. Previously compared to MRE and MRI-PDFF, this study validates those results in a new cohort of patients from Texas and Mississippi.
Methods: Patients with a clinical history of MASLD or MASH were enrolled in the study with a goal of enrolling patients with an even distribution of fibrosis and steatosis. All patients received an MR elastography (MRE) and MRI-Proton Density Fat Fraction (MRI-PDFF) scan within 28 days of the ultrasound scan. The MRE and MRI-PDFF were used as the ground truth, and MR based cutoffs were used to define disease status. For each MR cutoff, the area under the receiver operating characteristic curve (AUROC) is calculated for S-WAVE (elasticity), and ACE (attenuation). These results are then compared to previously published results.
Results: A total of 106 patients with clinically diagnosed MASLD or MASH were enrolled at two sites in the US. Of those enrolled, 87 patients in the analysis had a valid Velacur and MRE and MRI-PDFF scan. Fifteen patients did not complete the MRI due to scheduling, technical problems or patient discontinuation. Five patients failed to meet the quality thresholds defined by the objective AI algorithm on the device. Mean age was 58.9 years and the mean BMI was 32.3 kg/m2. For each of the MRE cutoffs, the resulting S-WAVE AUROC was >0.9 showing excellent discriminator ability for the full range of fibrosis stages, with the AUROC for advanced fibrosis being 0.95 [0.88, 0.98]. For MRI-PDFF cutoffs, the ACE AUROC for > 11%, or moderate steatosis, was 0.89 [0.80, 0.94]. These results align with previous regards, in which AUROC’s ranged from 0.83-0.97 for S-WAVE and 0.91-0.94 for ACE.
Discussion: In the first validation study, the results demonstrate the continued excellent performance of S-WAVE and ACE, in a new cohort of patients with MASLD and MASH. Using non-invasive MRI measures as the standard for patient diagnosis, S-WAVE and ACE show high discriminatory ability for a range of patient fibrosis and steatosis.
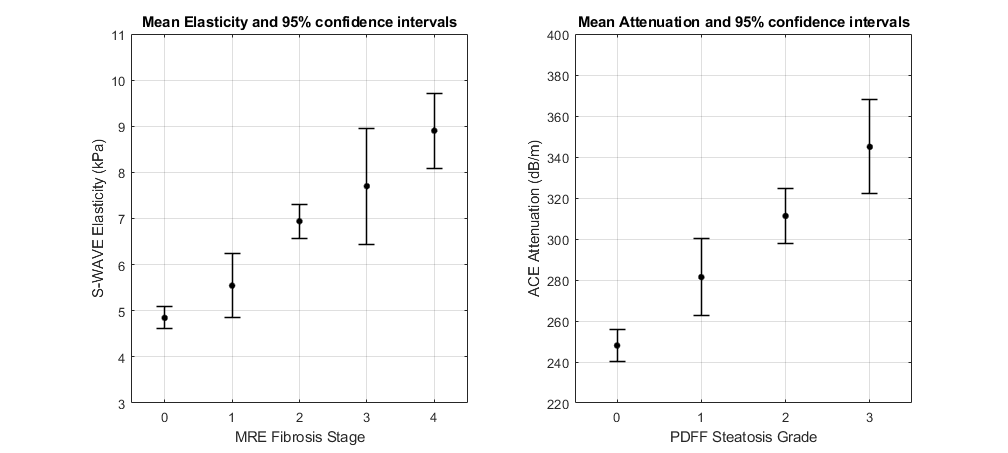
Figure: Mean S-WAVE Elasticity and ACE for each fibrosis stage and steatosis grade as defined by MRE (left) and MRI-PDFF (right) respectively
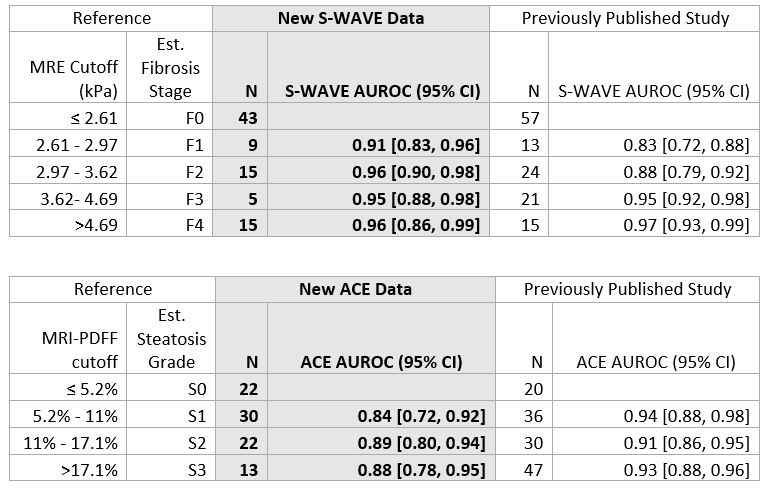
Figure: Comparison of results from this study to those of previously published literature
Disclosures:
Sri Naveen Surapaneni: Sonic Incytes – Grant/Research Support.
Reed Hogan: Sonic Incytes Medical Corp – Grant/Research Support.
Tessa Mury indicated no relevant financial relationships.
Ashley Horton indicated no relevant financial relationships.
Dominique Claiborne indicated no relevant financial relationships.
Caitlin Schneider: Sonic Incytes Medical Corp – Employee, Intellectual Property/Patents, Stock-privately held company.
Sri Naveen Surapaneni, MD, MPH1, Reed Hogan, MD2, Tessa Mury, MPH3, Ashley Horton, BS3, Dominique Claiborne, 4, Caitlin Schneider, PhD4. P1675 - Validation of S-WAVE Elasticity and ACE Attenuation Against MRE and MRI-PDFF in Patients with Clinically Diagnosed MASLD or MASH, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Texas Digestive Disease Consultants/ GI Alliance, Houston, TX; 2GI Associates & Endoscopy Center: Flowood, Flowood, MS; 3Texas Digestive Disease Consultants, Webster, TX; 4Sonic Incytes Medical Corp, Vancouver, BC, Canada
Introduction: Non-invasive tools for liver assessment are increasingly becoming standard of care for screening, diagnosing and monitoring patients with MASLD and MASH. New guidance recommends that imaging tools be used in assessing clinics for assessing patients and determining eligibility for new treatments. Shear wave absolute vibro-elasticity (S-WAVE) and Attenuation Coefficient Estimate (ACE), available on Velacur devices represent a new point-of-care imaging of stiffness and estimates of liver fat based on quantitative ultrasound parameters. Previously compared to MRE and MRI-PDFF, this study validates those results in a new cohort of patients from Texas and Mississippi.
Methods: Patients with a clinical history of MASLD or MASH were enrolled in the study with a goal of enrolling patients with an even distribution of fibrosis and steatosis. All patients received an MR elastography (MRE) and MRI-Proton Density Fat Fraction (MRI-PDFF) scan within 28 days of the ultrasound scan. The MRE and MRI-PDFF were used as the ground truth, and MR based cutoffs were used to define disease status. For each MR cutoff, the area under the receiver operating characteristic curve (AUROC) is calculated for S-WAVE (elasticity), and ACE (attenuation). These results are then compared to previously published results.
Results: A total of 106 patients with clinically diagnosed MASLD or MASH were enrolled at two sites in the US. Of those enrolled, 87 patients in the analysis had a valid Velacur and MRE and MRI-PDFF scan. Fifteen patients did not complete the MRI due to scheduling, technical problems or patient discontinuation. Five patients failed to meet the quality thresholds defined by the objective AI algorithm on the device. Mean age was 58.9 years and the mean BMI was 32.3 kg/m2. For each of the MRE cutoffs, the resulting S-WAVE AUROC was >0.9 showing excellent discriminator ability for the full range of fibrosis stages, with the AUROC for advanced fibrosis being 0.95 [0.88, 0.98]. For MRI-PDFF cutoffs, the ACE AUROC for > 11%, or moderate steatosis, was 0.89 [0.80, 0.94]. These results align with previous regards, in which AUROC’s ranged from 0.83-0.97 for S-WAVE and 0.91-0.94 for ACE.
Discussion: In the first validation study, the results demonstrate the continued excellent performance of S-WAVE and ACE, in a new cohort of patients with MASLD and MASH. Using non-invasive MRI measures as the standard for patient diagnosis, S-WAVE and ACE show high discriminatory ability for a range of patient fibrosis and steatosis.
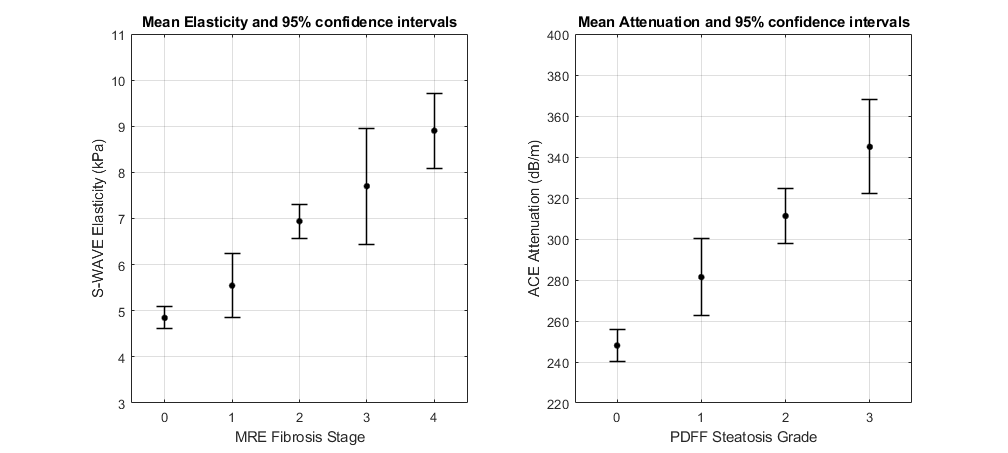
Figure: Mean S-WAVE Elasticity and ACE for each fibrosis stage and steatosis grade as defined by MRE (left) and MRI-PDFF (right) respectively
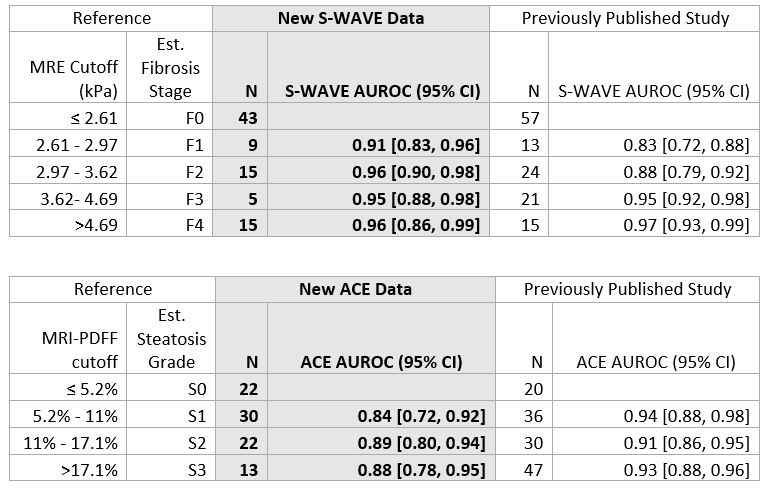
Figure: Comparison of results from this study to those of previously published literature
Disclosures:
Sri Naveen Surapaneni: Sonic Incytes – Grant/Research Support.
Reed Hogan: Sonic Incytes Medical Corp – Grant/Research Support.
Tessa Mury indicated no relevant financial relationships.
Ashley Horton indicated no relevant financial relationships.
Dominique Claiborne indicated no relevant financial relationships.
Caitlin Schneider: Sonic Incytes Medical Corp – Employee, Intellectual Property/Patents, Stock-privately held company.
Sri Naveen Surapaneni, MD, MPH1, Reed Hogan, MD2, Tessa Mury, MPH3, Ashley Horton, BS3, Dominique Claiborne, 4, Caitlin Schneider, PhD4. P1675 - Validation of S-WAVE Elasticity and ACE Attenuation Against MRE and MRI-PDFF in Patients with Clinically Diagnosed MASLD or MASH, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
