Sunday Poster Session
Category: Liver
P1671 - Statins Are Underutilized and Underdosed in Patients Undergoing Liver Transplant Evaluation, Despite High ASCVD Risk
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- GN
Gomathy Nageswaran, MBBS (she/her/hers)
University of Arkansas for Medical Sciences
Little Rock, AR
Presenting Author(s)
Gomathy Nageswaran, MBBS1, Shambhavi Anshumali, MD1, Drew Castleberry, MD1, Mauricio Garcia, MD1, Srikanth Vallurupalli, MD2, Ragesh Thandassery, MD3
1University of Arkansas for Medical Sciences, Little Rock, AR; 2Central Arkansas Veterans Healthcare System, Little Rock, AR; 3Dept of Solid Organ Transplantation, University of Arkansas for Medical Sciences, Little Rock, AR
Introduction: Atherosclerotic cardiovascular disease (ASCVD) is an important and common cause of death in patients with cirrhosis. The 2013 ACC/AHA ASCVD risk score provides a 10-year risk estimate of the incidence of hard ASCVD (myocardial infarction, stroke, or death due to coronary heart disease or stroke) in patients aged 40-75 years. HMG-CoA reductase inhibitors (statins) are known to reduce mortality risk in patients with high ASCVD risk. Statins are underutilized in cirrhosis due to popular misconceptions about their risk for hepatotoxicity. We aimed to characterize the ASCVD risk scores, and the pattern of statin use among patients undergoing liver transplant (LT) evaluation.
Methods: We retrospectively analyzed 499 patients undergoing liver transplant (LT) evaluation between 2015 and 2024 in the Midwest US. An ASCVD risk score between 7.5% and 19.9% indicated intermediate risk, and a score of >20% indicated a high risk of ASCVD.
Results: Mean age was 57.1(SD 10.4), with a median BMI of 28.7(IQR 24.7-33.1). The population was 43.1% female and predominantly Caucasian (82.7%). Median MELD score was 17 (IQR 11-24). 31.1% (n=155) had intermediate ASCVD risk and 41.0% (n=204) had high ASCVD risk at the time of LT evaluation. Of each of these groups, only 25.2% (n = 39) and 23.5% (n = 48) of the patients were on statins. Among those with established coronary artery disease (n=63), only one-third (n=21) were on statins.
Out of the 105 patients who were on statins, 23.8% were on high-intensity statins, 61.0% were on moderate-intensity, and 15.2% were on low-intensity statins. Out of the patients with a MELD score of >15, 21.7% were on statins, whereas among those with a MELD score of <15, 20.7% were on statins. The median LDL-C for patients on statins was 76 mg/dL (IQR, 59-110 mg/dL) compared to 85 mg/dL (IQR, 67-112 mg/dL) for those not on statins, p-value = 0.13 (Figure 1).
Discussion: The safety of statins in cirrhosis, with the benefit of reducing both all-cause and cardiovascular mortality, is well established. However, statins are underutilized and underdosed in this cohort of patients undergoing LT evaluation with significant ASCVD risk. Popular misconceptions about statin use in cirrhosis could be mitigated by interdisciplinary discussions with primary care providers and cardiologists to help optimize statin use in these high-risk patients.
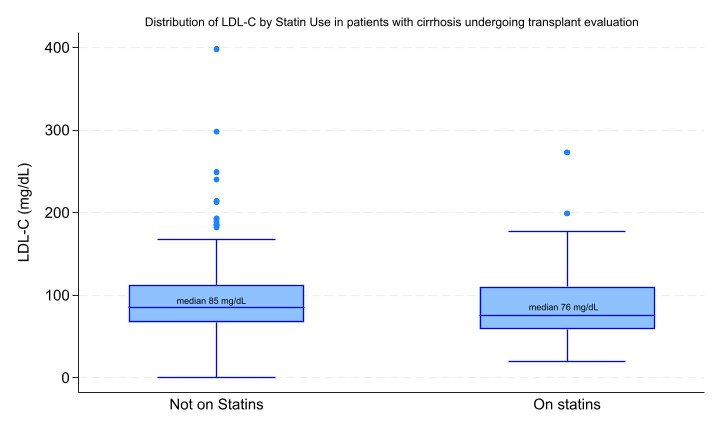
Figure: Distribution of LDL-C levels by statin use in patients with cirrhosis undergoing liver transplant evaluation
Disclosures:
Gomathy Nageswaran indicated no relevant financial relationships.
Shambhavi Anshumali indicated no relevant financial relationships.
Drew Castleberry indicated no relevant financial relationships.
Mauricio Garcia indicated no relevant financial relationships.
Srikanth Vallurupalli indicated no relevant financial relationships.
Ragesh Thandassery indicated no relevant financial relationships.
Gomathy Nageswaran, MBBS1, Shambhavi Anshumali, MD1, Drew Castleberry, MD1, Mauricio Garcia, MD1, Srikanth Vallurupalli, MD2, Ragesh Thandassery, MD3. P1671 - Statins Are Underutilized and Underdosed in Patients Undergoing Liver Transplant Evaluation, Despite High ASCVD Risk, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Arkansas for Medical Sciences, Little Rock, AR; 2Central Arkansas Veterans Healthcare System, Little Rock, AR; 3Dept of Solid Organ Transplantation, University of Arkansas for Medical Sciences, Little Rock, AR
Introduction: Atherosclerotic cardiovascular disease (ASCVD) is an important and common cause of death in patients with cirrhosis. The 2013 ACC/AHA ASCVD risk score provides a 10-year risk estimate of the incidence of hard ASCVD (myocardial infarction, stroke, or death due to coronary heart disease or stroke) in patients aged 40-75 years. HMG-CoA reductase inhibitors (statins) are known to reduce mortality risk in patients with high ASCVD risk. Statins are underutilized in cirrhosis due to popular misconceptions about their risk for hepatotoxicity. We aimed to characterize the ASCVD risk scores, and the pattern of statin use among patients undergoing liver transplant (LT) evaluation.
Methods: We retrospectively analyzed 499 patients undergoing liver transplant (LT) evaluation between 2015 and 2024 in the Midwest US. An ASCVD risk score between 7.5% and 19.9% indicated intermediate risk, and a score of >20% indicated a high risk of ASCVD.
Results: Mean age was 57.1(SD 10.4), with a median BMI of 28.7(IQR 24.7-33.1). The population was 43.1% female and predominantly Caucasian (82.7%). Median MELD score was 17 (IQR 11-24). 31.1% (n=155) had intermediate ASCVD risk and 41.0% (n=204) had high ASCVD risk at the time of LT evaluation. Of each of these groups, only 25.2% (n = 39) and 23.5% (n = 48) of the patients were on statins. Among those with established coronary artery disease (n=63), only one-third (n=21) were on statins.
Out of the 105 patients who were on statins, 23.8% were on high-intensity statins, 61.0% were on moderate-intensity, and 15.2% were on low-intensity statins. Out of the patients with a MELD score of >15, 21.7% were on statins, whereas among those with a MELD score of <15, 20.7% were on statins. The median LDL-C for patients on statins was 76 mg/dL (IQR, 59-110 mg/dL) compared to 85 mg/dL (IQR, 67-112 mg/dL) for those not on statins, p-value = 0.13 (Figure 1).
Discussion: The safety of statins in cirrhosis, with the benefit of reducing both all-cause and cardiovascular mortality, is well established. However, statins are underutilized and underdosed in this cohort of patients undergoing LT evaluation with significant ASCVD risk. Popular misconceptions about statin use in cirrhosis could be mitigated by interdisciplinary discussions with primary care providers and cardiologists to help optimize statin use in these high-risk patients.
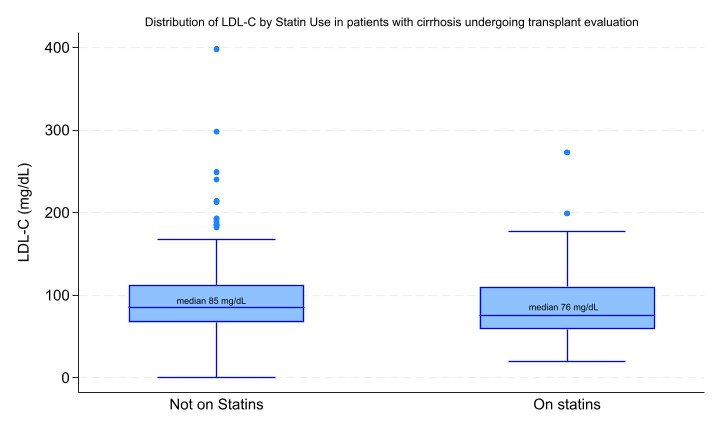
Figure: Distribution of LDL-C levels by statin use in patients with cirrhosis undergoing liver transplant evaluation
Disclosures:
Gomathy Nageswaran indicated no relevant financial relationships.
Shambhavi Anshumali indicated no relevant financial relationships.
Drew Castleberry indicated no relevant financial relationships.
Mauricio Garcia indicated no relevant financial relationships.
Srikanth Vallurupalli indicated no relevant financial relationships.
Ragesh Thandassery indicated no relevant financial relationships.
Gomathy Nageswaran, MBBS1, Shambhavi Anshumali, MD1, Drew Castleberry, MD1, Mauricio Garcia, MD1, Srikanth Vallurupalli, MD2, Ragesh Thandassery, MD3. P1671 - Statins Are Underutilized and Underdosed in Patients Undergoing Liver Transplant Evaluation, Despite High ASCVD Risk, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
