Sunday Poster Session
Category: Liver
P1631 - PCABs or PPIs for Cirrhotic Patients? A Real-World Analysis of Bleeding Outcomes Using TriNetX
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- VS
Venkata Sunkesula, MD
Case Western Reserve University / MetroHealth
Cleveland, OH
Presenting Author(s)
Venkata Sunkesula, MD1, Thai Hau Koo, MD2, Rishi Chowdhary, MD1, Archana Kharel, MD3, Sirisha kundrapu, MD1, Ala Abdel-Jalil, MD4
1Case Western Reserve University / MetroHealth, Cleveland, OH; 2University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 3Cleveland Clinic, Cleveland, OH; 4MetroHealth Medical Center - CLEVELAND, OH, Cleveland, OH
Introduction: The comparative effectiveness of PCABs and PPIs in preventing upper gastrointestinal bleeding (UGIB) in cirrhotic patients remains unclear. Although PPIs are commonly used for acid suppression, concerns exist about their potential risks, including infections and hepatic encephalopathy. This study compares the incidence of UGIB following initiation of PCAB versus PPI therapy in patients with Cirrhosis.
Methods: We performed a retrospective cohort study using TriNetX Research Network, a federated database of de-identified electronic health records. Data were collected from 134 healthcare organizations in 14 different countries. Adult patients (≥18 years) with a diagnosis of Cirrhosis between January 1, 2016, and December 31, 2024, who were prescribed either PCAB or PPI, were identified. Patients with a history of UGIB within 6 months prior to drug initiation were excluded. Patients with PCAB exposure were also excluded if they had received a PPI within 6 months of PCAB initiation. Propensity score matching (1:1) was adjusted for demographic characteristics and known risk factors of UGIB. Kaplan-Meier survival analysis and univariate Cox proportional hazards models were used to assess the incidence of UGIB within 90 days of therapy initiation. The secondary outcomes included rebleeding, need for endoscopic intervention, and mortality.
Results: A total of 790,065 adults with cirrhosis and 137,843,348 without were analyzed. Before propensity score matching (PSM), PCAB users were older and had higher rates of diabetes, dialysis, and anticoagulant/antiplatelet use, but lower rates of varices, alcohol use, and NSAID exposure (all p< 0.001). After 1:1 PSM, 58 patients per group were matched. Within 90 days, UGIB incidence was significantly lower with PCABs than PPIs (OR 0.490; 95% CI, 0.261–0.921; p=0.024). While endoscopic intervention rates were similar (p=0.079), the PCAB group had significantly lower rebleeding rates (p=0.010) and inpatient mortality (OR 0.294; 95% CI, 0.156–0.552; p< 0.001).
Discussion: PCAB use was associated with significantly lower odds of UGIB compared to PPI use. PCAB users also had lower rates of rebleeding and inpatient mortality, suggesting a safer bleeding profile in patients with Cirrhosis. These findings support re-evaluating acid suppression strategies in cirrhotic patients at high risk for bleeding.
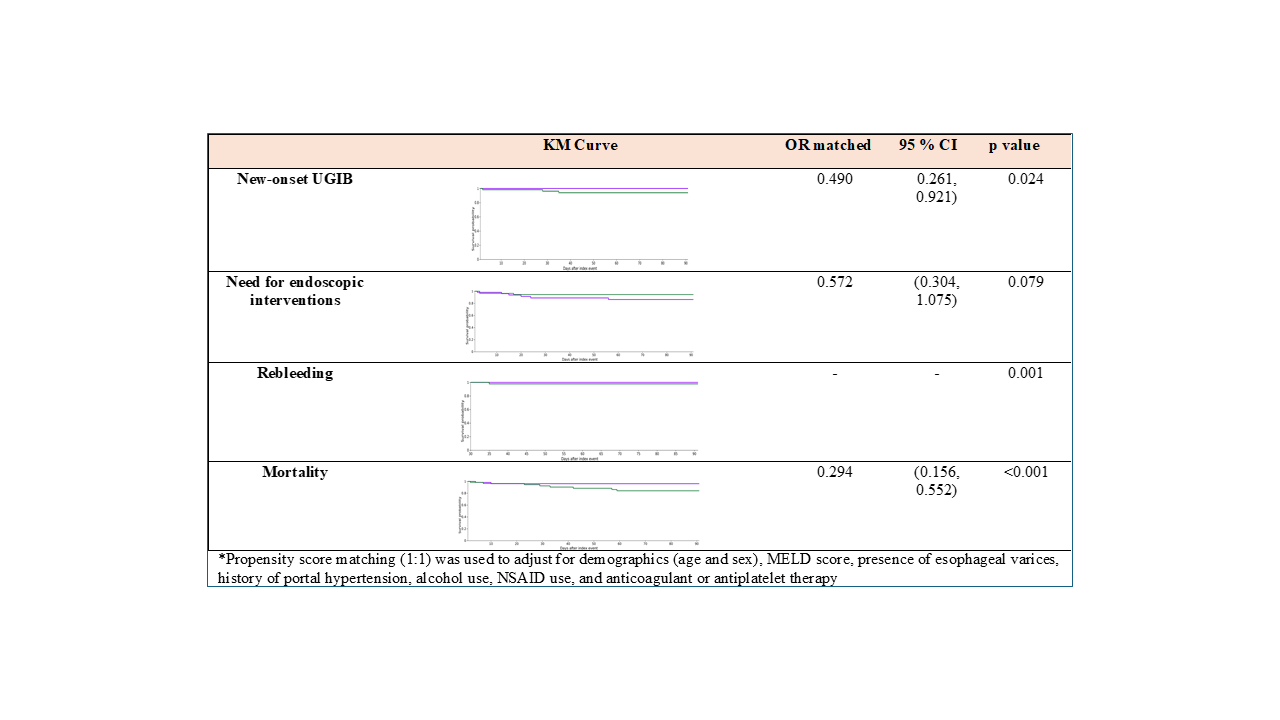
Figure: Demographics and clinical variables of patients with liver cirrhosis among those with PCAB as compared to PPI
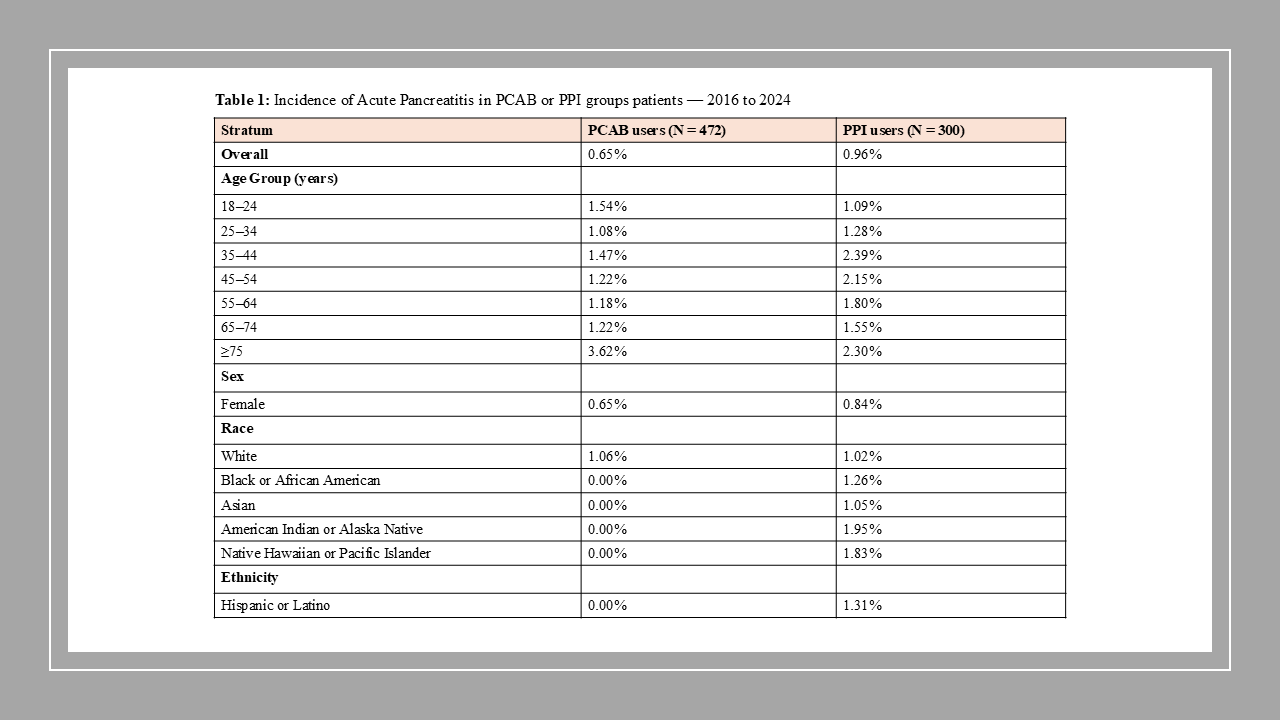
Figure: Odds ratios* of clinical outcome of patients with liver cirrhosis among those with PCAB as compared to PPI within the first 90 days follow up.
Disclosures:
Venkata Sunkesula indicated no relevant financial relationships.
Thai Hau Koo indicated no relevant financial relationships.
Rishi Chowdhary indicated no relevant financial relationships.
Archana Kharel indicated no relevant financial relationships.
Sirisha kundrapu indicated no relevant financial relationships.
Ala Abdel-Jalil indicated no relevant financial relationships.
Venkata Sunkesula, MD1, Thai Hau Koo, MD2, Rishi Chowdhary, MD1, Archana Kharel, MD3, Sirisha kundrapu, MD1, Ala Abdel-Jalil, MD4. P1631 - PCABs or PPIs for Cirrhotic Patients? A Real-World Analysis of Bleeding Outcomes Using TriNetX, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Case Western Reserve University / MetroHealth, Cleveland, OH; 2University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 3Cleveland Clinic, Cleveland, OH; 4MetroHealth Medical Center - CLEVELAND, OH, Cleveland, OH
Introduction: The comparative effectiveness of PCABs and PPIs in preventing upper gastrointestinal bleeding (UGIB) in cirrhotic patients remains unclear. Although PPIs are commonly used for acid suppression, concerns exist about their potential risks, including infections and hepatic encephalopathy. This study compares the incidence of UGIB following initiation of PCAB versus PPI therapy in patients with Cirrhosis.
Methods: We performed a retrospective cohort study using TriNetX Research Network, a federated database of de-identified electronic health records. Data were collected from 134 healthcare organizations in 14 different countries. Adult patients (≥18 years) with a diagnosis of Cirrhosis between January 1, 2016, and December 31, 2024, who were prescribed either PCAB or PPI, were identified. Patients with a history of UGIB within 6 months prior to drug initiation were excluded. Patients with PCAB exposure were also excluded if they had received a PPI within 6 months of PCAB initiation. Propensity score matching (1:1) was adjusted for demographic characteristics and known risk factors of UGIB. Kaplan-Meier survival analysis and univariate Cox proportional hazards models were used to assess the incidence of UGIB within 90 days of therapy initiation. The secondary outcomes included rebleeding, need for endoscopic intervention, and mortality.
Results: A total of 790,065 adults with cirrhosis and 137,843,348 without were analyzed. Before propensity score matching (PSM), PCAB users were older and had higher rates of diabetes, dialysis, and anticoagulant/antiplatelet use, but lower rates of varices, alcohol use, and NSAID exposure (all p< 0.001). After 1:1 PSM, 58 patients per group were matched. Within 90 days, UGIB incidence was significantly lower with PCABs than PPIs (OR 0.490; 95% CI, 0.261–0.921; p=0.024). While endoscopic intervention rates were similar (p=0.079), the PCAB group had significantly lower rebleeding rates (p=0.010) and inpatient mortality (OR 0.294; 95% CI, 0.156–0.552; p< 0.001).
Discussion: PCAB use was associated with significantly lower odds of UGIB compared to PPI use. PCAB users also had lower rates of rebleeding and inpatient mortality, suggesting a safer bleeding profile in patients with Cirrhosis. These findings support re-evaluating acid suppression strategies in cirrhotic patients at high risk for bleeding.
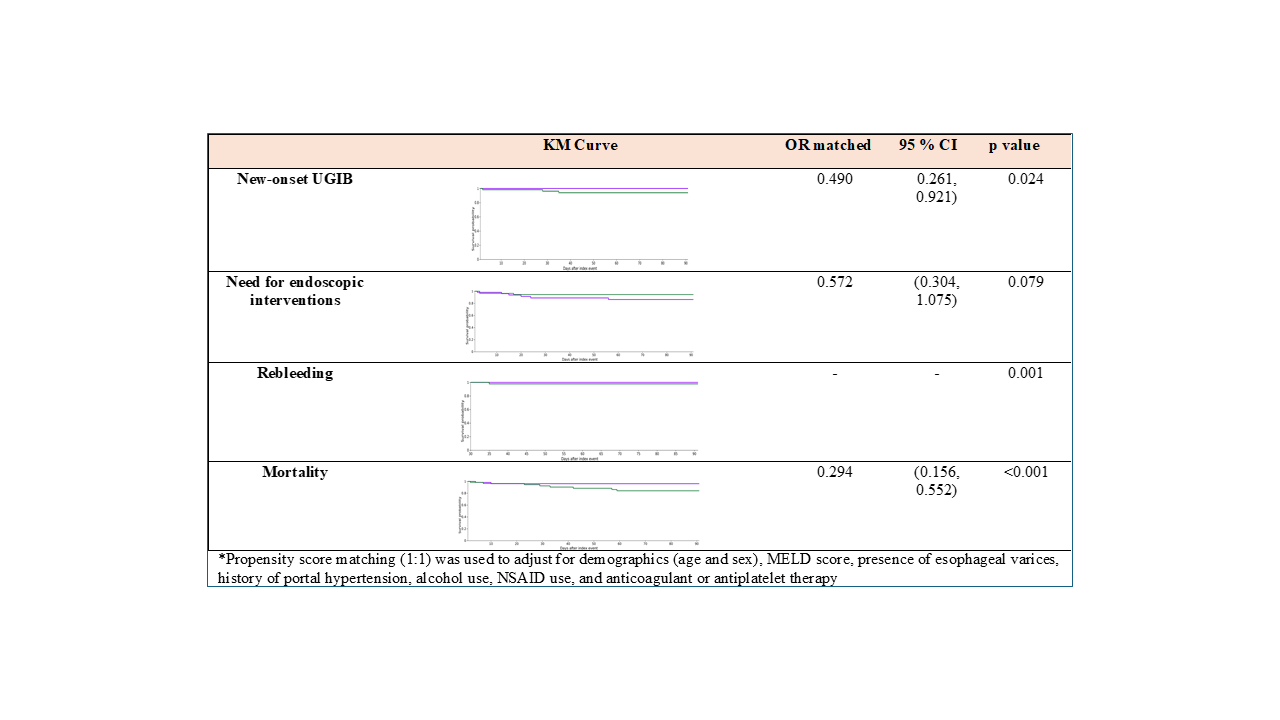
Figure: Demographics and clinical variables of patients with liver cirrhosis among those with PCAB as compared to PPI
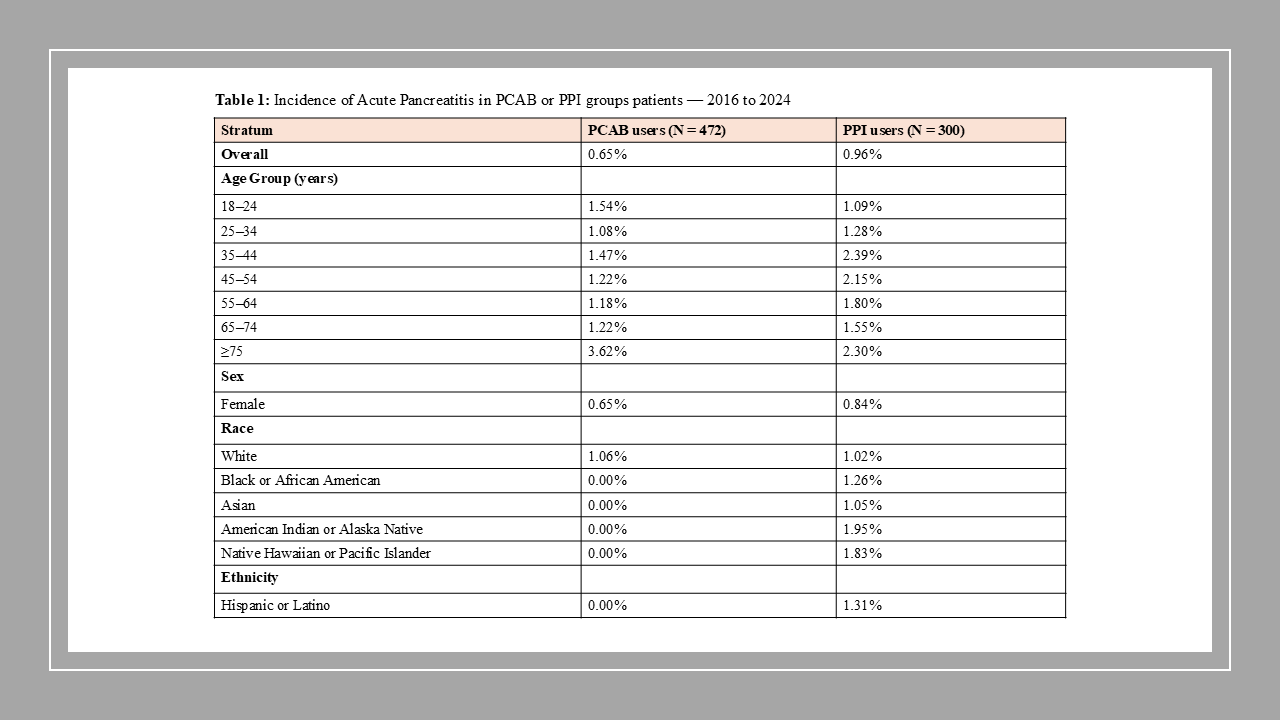
Figure: Odds ratios* of clinical outcome of patients with liver cirrhosis among those with PCAB as compared to PPI within the first 90 days follow up.
Disclosures:
Venkata Sunkesula indicated no relevant financial relationships.
Thai Hau Koo indicated no relevant financial relationships.
Rishi Chowdhary indicated no relevant financial relationships.
Archana Kharel indicated no relevant financial relationships.
Sirisha kundrapu indicated no relevant financial relationships.
Ala Abdel-Jalil indicated no relevant financial relationships.
Venkata Sunkesula, MD1, Thai Hau Koo, MD2, Rishi Chowdhary, MD1, Archana Kharel, MD3, Sirisha kundrapu, MD1, Ala Abdel-Jalil, MD4. P1631 - PCABs or PPIs for Cirrhotic Patients? A Real-World Analysis of Bleeding Outcomes Using TriNetX, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

