Sunday Poster Session
Category: Liver
P1625 - Transition from Locoregional to Systemic Therapies for Hepatocellular Carcinoma (HCC) Does Not Improve Survival
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Eddy KW Leung, MD (he/him/his)
Oregon Health & Science University
Portland, OR
Presenting Author(s)
Eddy KW. Leung, MD, Scott Naugler, MD
Oregon Health & Science University, Portland, OR
Introduction: Locoregional therapies (LRT) are frequently recommended as initial treatment for hepatocellular carcinoma (HCC), though no clear data exists on how to sequence LRTs and systemic therapy in such patients. In practice, many patients who might benefit from systemic therapies never transition to them due to hepatic decompensation from repeated LRT. It remains unclear whether transitioning to systemic therapy improves outcomes compared to remaining on LRT until death, or if a strategy of starting with systemic treatment may be optimal.
Methods: We conducted a retrospective, single-center cohort study of 375 patients with HCC who presented consecutively to the OHSU multidisciplinary liver tumor board from 5/2021 to 11/2023. Patients with metastatic disease, those considered for liver transplant, and those with concurrent other malignancies were excluded. We focused only on patients who died within the treatment period or with a minimum of one year of follow up from the initiation of treatment. We compared patients who received LRT alone and those who transitioned to systemic therapy before death. Survival time was calculated from diagnosis to death. Kaplan-Meier curves and log-rank tests were used for survival comparisons.
Results: Among 375 initial patients with HCC, 65 died during the study period or within a year after and received LRT as initial therapy. Of these, 39 received LRT alone and 26 ultimately transitioned to systemic therapy, which was almost exclusively systemic immunotherapy of varying regimens. In the focused comparison, median survival was similar between LRT alone and LRT/systemic therapy groups (713 vs 743 days; p = 0.78). Stratified survival showed no survival differences in the treatment groups in low MELD ≤10 (p = 0.91) or high MELD >10 (p = 0.77). Regardless of treatment, MELD ≤10 was associated with improved survival compared to MELD >10 (832 vs 585 days; p = 0.062).
Discussion: In this cohort of HCC patients initially treated with LRT, transition to systemic therapy did not improve survival over LRT alone. Ongoing studies assessing the combination of systemic and LRT from treatment onset may help to clarify treatment sequencing questions for these patients. As in other studies, this study confirms that liver dysfunction is a key indicator of death in these patients, driving prognosis as much as oncologic burden.
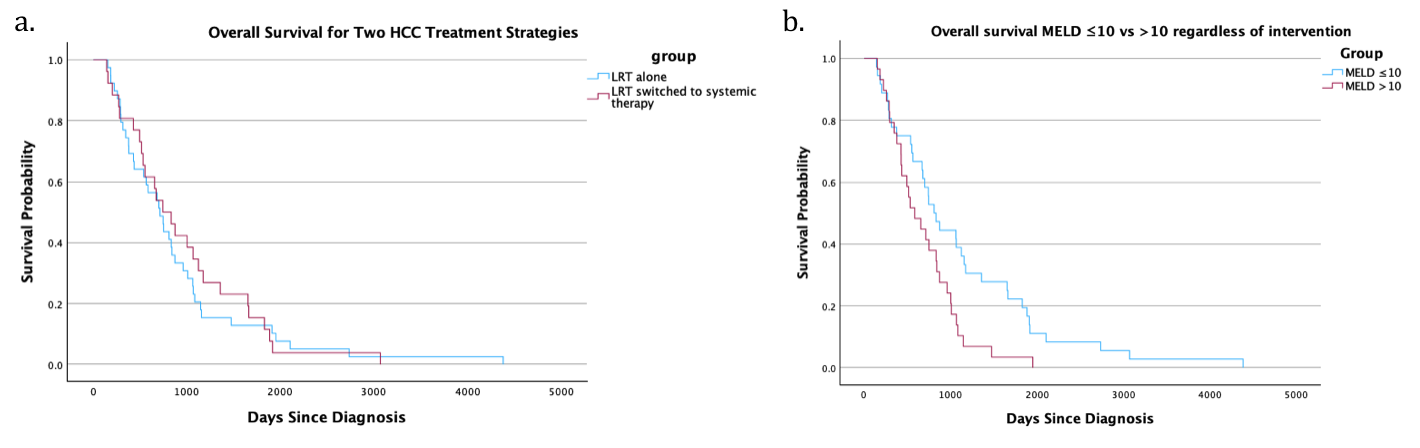
Figure: Figure: Kaplan-Meier survival curves. Survival probability was compared between groups using the log-rank test. a) Those who received LRT alone and those who transitioned to systemic therapy prior to death showed similar survival (median survival 713 vs 743 days; p= 0.78). b) There was a trend toward improved survival in patients with MELD ≤10 compared to those with MELD >10, when not accounting for treatment strategy (median survival 832 vs 585 days; p= 0.062).
Disclosures:
Eddy Leung indicated no relevant financial relationships.
Scott Naugler indicated no relevant financial relationships.
Eddy KW. Leung, MD, Scott Naugler, MD. P1625 - Transition from Locoregional to Systemic Therapies for Hepatocellular Carcinoma (HCC) Does Not Improve Survival, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Oregon Health & Science University, Portland, OR
Introduction: Locoregional therapies (LRT) are frequently recommended as initial treatment for hepatocellular carcinoma (HCC), though no clear data exists on how to sequence LRTs and systemic therapy in such patients. In practice, many patients who might benefit from systemic therapies never transition to them due to hepatic decompensation from repeated LRT. It remains unclear whether transitioning to systemic therapy improves outcomes compared to remaining on LRT until death, or if a strategy of starting with systemic treatment may be optimal.
Methods: We conducted a retrospective, single-center cohort study of 375 patients with HCC who presented consecutively to the OHSU multidisciplinary liver tumor board from 5/2021 to 11/2023. Patients with metastatic disease, those considered for liver transplant, and those with concurrent other malignancies were excluded. We focused only on patients who died within the treatment period or with a minimum of one year of follow up from the initiation of treatment. We compared patients who received LRT alone and those who transitioned to systemic therapy before death. Survival time was calculated from diagnosis to death. Kaplan-Meier curves and log-rank tests were used for survival comparisons.
Results: Among 375 initial patients with HCC, 65 died during the study period or within a year after and received LRT as initial therapy. Of these, 39 received LRT alone and 26 ultimately transitioned to systemic therapy, which was almost exclusively systemic immunotherapy of varying regimens. In the focused comparison, median survival was similar between LRT alone and LRT/systemic therapy groups (713 vs 743 days; p = 0.78). Stratified survival showed no survival differences in the treatment groups in low MELD ≤10 (p = 0.91) or high MELD >10 (p = 0.77). Regardless of treatment, MELD ≤10 was associated with improved survival compared to MELD >10 (832 vs 585 days; p = 0.062).
Discussion: In this cohort of HCC patients initially treated with LRT, transition to systemic therapy did not improve survival over LRT alone. Ongoing studies assessing the combination of systemic and LRT from treatment onset may help to clarify treatment sequencing questions for these patients. As in other studies, this study confirms that liver dysfunction is a key indicator of death in these patients, driving prognosis as much as oncologic burden.
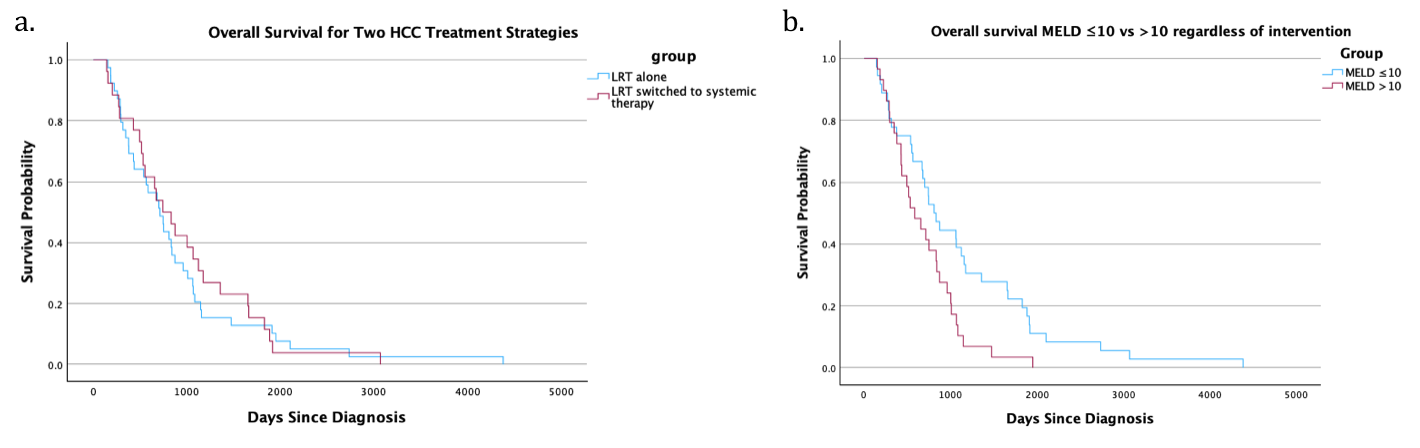
Figure: Figure: Kaplan-Meier survival curves. Survival probability was compared between groups using the log-rank test. a) Those who received LRT alone and those who transitioned to systemic therapy prior to death showed similar survival (median survival 713 vs 743 days; p= 0.78). b) There was a trend toward improved survival in patients with MELD ≤10 compared to those with MELD >10, when not accounting for treatment strategy (median survival 832 vs 585 days; p= 0.062).
Disclosures:
Eddy Leung indicated no relevant financial relationships.
Scott Naugler indicated no relevant financial relationships.
Eddy KW. Leung, MD, Scott Naugler, MD. P1625 - Transition from Locoregional to Systemic Therapies for Hepatocellular Carcinoma (HCC) Does Not Improve Survival, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
