Sunday Poster Session
Category: Liver
P1606 - Impact of Cirrhosis on Rare and Common Thromboembolic Events in Acute Pancreatitis: A Propensity-Matched Cohort Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Hany Habib, MD
Allegheny Health Network Medicine Institute
Pittsburgh, PA
Presenting Author(s)
Hany Habib, MD1, Kojo-Frimpong B. Awuah, MD2, Somtochukwu Onwuzo, MD3, Kaitlyn Gernhard, DO1, Tyrell Daniel, MD4, Rashid Abdel-Razeq, MD5, Chidera Onwuzo, MBBS6
1Allegheny Health Network Medicine Institute, Pittsburgh, PA; 2Allegheny Health Network, Pittsburgh, PA; 3Allegheny Center for Digestive Health, Pittsburgh, PA; 4Sentara Northern Virginia Medical Center, Pittsburgh, PA; 5Cleveland Clinic Foundation, Cleveland, OH; 6SUNY Upstate Medical University Hospital, Syracuse, NY
Introduction: Cirrhosis increases the risk of mortality and thromboembolic complications in acute pancreatitis (AP), particularly portal vein thrombosis (PVT) and deep vein thrombosis (DVT). While these are well-described, the incidence of rarer thromboemolic events, such as hepatic vein, inferior vena cava (IVC), and left ventricular (LV) thrombi, remains unknown.
Methods: We conducted a retrospective cohort study using the TriNetX database to compare thromboembolic events in hospitalized adults with AP with and without cirrhosis. Cirrhosis was defined using validated ICD-10 codes recorded prior to or at the index AP admission. Propensity score matching (1:1) was performed for demographics and comorbidities to minimize baseline differences. The primary outcomes were rare thromboembolic events, and results were reported using risk ratios (RRs) with 95% confidence intervals (CIs); statistical significance was defined as p< 0.05.
Results: We identified 27,002 AP patients with cirrhosis and 586,636 without. Following 1:1 propensity score matching, rare thromboembolic events were significantly more common in cirrhotic patients: hepatic vein thrombosis (0.19% vs. 0.04%; RR 5.02, 95% CI 2.55–9.90; p< 0.001) and IVC thrombosis (0.12% vs. 0.06%; RR 1.83, 95% CI 1.01–3.30; p=0.042). Left ventricular thrombus was not significantly different between groups (0.20% vs. 0.19%; RR 1.02, 95% CI 0.69–1.51; p=0.919). Among secondary outcomes, cirrhotic patients had higher risk of PVT (2.2% vs. 0.5%; RR 4.03, 95% CI 3.35–4.85; p< 0.001) and DVT (1.8% vs. 1.4%; RR 1.31, 95% CI 1.14–1.50; p< 0.001), while rates of pulmonary embolism (1.1% vs. 1.2%; RR 0.93, 95% CI 0.79–1.09; p=0.379), axillary (0.04% vs. 0.04%; RR 1.10, 95% CI 0.47–2.59; p=0.826), and subclavian vein thrombosis (0.05% vs. 0.04%; RR 1.40, 95% CI 0.62–3.15; p=0.414) were also not significantly different.
Discussion: Cirrhosis is associated with a significantly increased risk of rare thromboembolic events in acute pancreatitis, particularly hepatic vein and IVC thromboses. These findings highlight the need for increased clinical awareness and targeted risk stratification in this high-risk population.
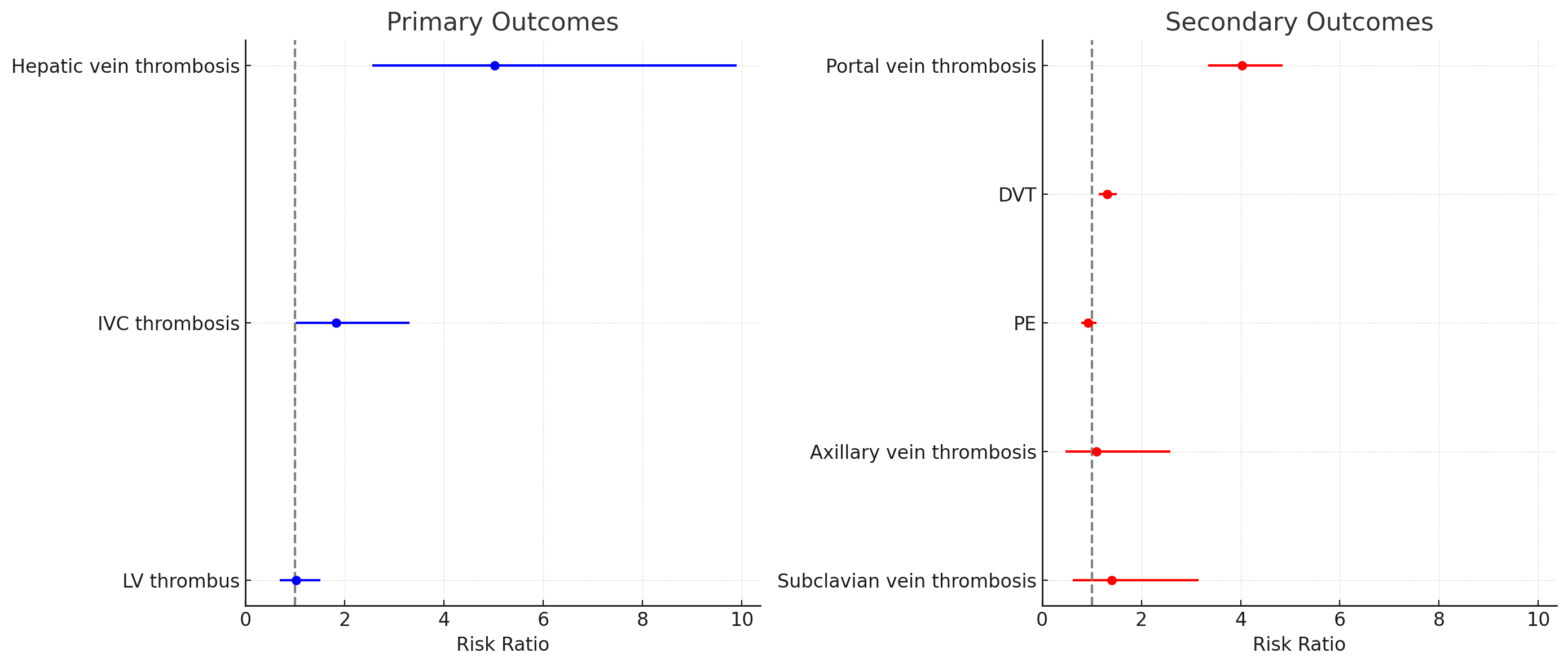
Figure: Figure 1. Forest Plots Comparing Risk Ratios of Thromboembolic Events in Acute Pancreatitis Between Cirrhotic and Non-Cirrhotic Patients
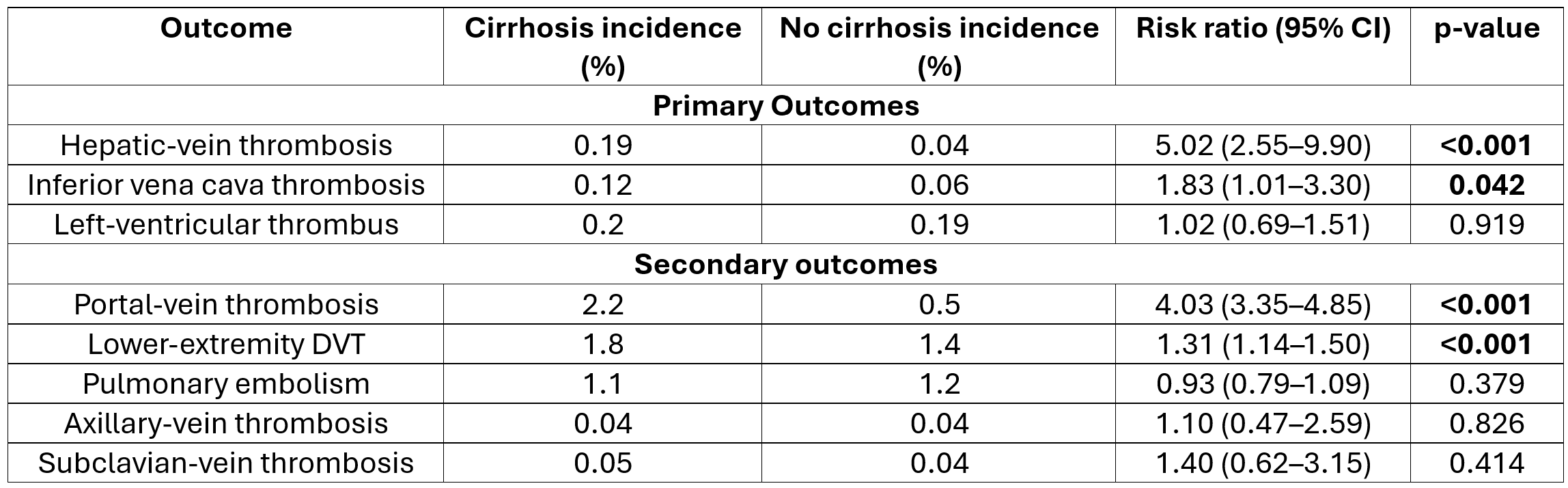
Figure: Table 1. Incidence and Risk Ratios of Thromboembolic Events in Acute Pancreatitis in Patients With Cirrhosis Compared to Those Without Cirrhosis
Disclosures:
Hany Habib indicated no relevant financial relationships.
Kojo-Frimpong B. Awuah indicated no relevant financial relationships.
Somtochukwu Onwuzo indicated no relevant financial relationships.
Kaitlyn Gernhard indicated no relevant financial relationships.
Tyrell Daniel indicated no relevant financial relationships.
Rashid Abdel-Razeq indicated no relevant financial relationships.
Chidera Onwuzo indicated no relevant financial relationships.
Hany Habib, MD1, Kojo-Frimpong B. Awuah, MD2, Somtochukwu Onwuzo, MD3, Kaitlyn Gernhard, DO1, Tyrell Daniel, MD4, Rashid Abdel-Razeq, MD5, Chidera Onwuzo, MBBS6. P1606 - Impact of Cirrhosis on Rare and Common Thromboembolic Events in Acute Pancreatitis: A Propensity-Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Allegheny Health Network Medicine Institute, Pittsburgh, PA; 2Allegheny Health Network, Pittsburgh, PA; 3Allegheny Center for Digestive Health, Pittsburgh, PA; 4Sentara Northern Virginia Medical Center, Pittsburgh, PA; 5Cleveland Clinic Foundation, Cleveland, OH; 6SUNY Upstate Medical University Hospital, Syracuse, NY
Introduction: Cirrhosis increases the risk of mortality and thromboembolic complications in acute pancreatitis (AP), particularly portal vein thrombosis (PVT) and deep vein thrombosis (DVT). While these are well-described, the incidence of rarer thromboemolic events, such as hepatic vein, inferior vena cava (IVC), and left ventricular (LV) thrombi, remains unknown.
Methods: We conducted a retrospective cohort study using the TriNetX database to compare thromboembolic events in hospitalized adults with AP with and without cirrhosis. Cirrhosis was defined using validated ICD-10 codes recorded prior to or at the index AP admission. Propensity score matching (1:1) was performed for demographics and comorbidities to minimize baseline differences. The primary outcomes were rare thromboembolic events, and results were reported using risk ratios (RRs) with 95% confidence intervals (CIs); statistical significance was defined as p< 0.05.
Results: We identified 27,002 AP patients with cirrhosis and 586,636 without. Following 1:1 propensity score matching, rare thromboembolic events were significantly more common in cirrhotic patients: hepatic vein thrombosis (0.19% vs. 0.04%; RR 5.02, 95% CI 2.55–9.90; p< 0.001) and IVC thrombosis (0.12% vs. 0.06%; RR 1.83, 95% CI 1.01–3.30; p=0.042). Left ventricular thrombus was not significantly different between groups (0.20% vs. 0.19%; RR 1.02, 95% CI 0.69–1.51; p=0.919). Among secondary outcomes, cirrhotic patients had higher risk of PVT (2.2% vs. 0.5%; RR 4.03, 95% CI 3.35–4.85; p< 0.001) and DVT (1.8% vs. 1.4%; RR 1.31, 95% CI 1.14–1.50; p< 0.001), while rates of pulmonary embolism (1.1% vs. 1.2%; RR 0.93, 95% CI 0.79–1.09; p=0.379), axillary (0.04% vs. 0.04%; RR 1.10, 95% CI 0.47–2.59; p=0.826), and subclavian vein thrombosis (0.05% vs. 0.04%; RR 1.40, 95% CI 0.62–3.15; p=0.414) were also not significantly different.
Discussion: Cirrhosis is associated with a significantly increased risk of rare thromboembolic events in acute pancreatitis, particularly hepatic vein and IVC thromboses. These findings highlight the need for increased clinical awareness and targeted risk stratification in this high-risk population.
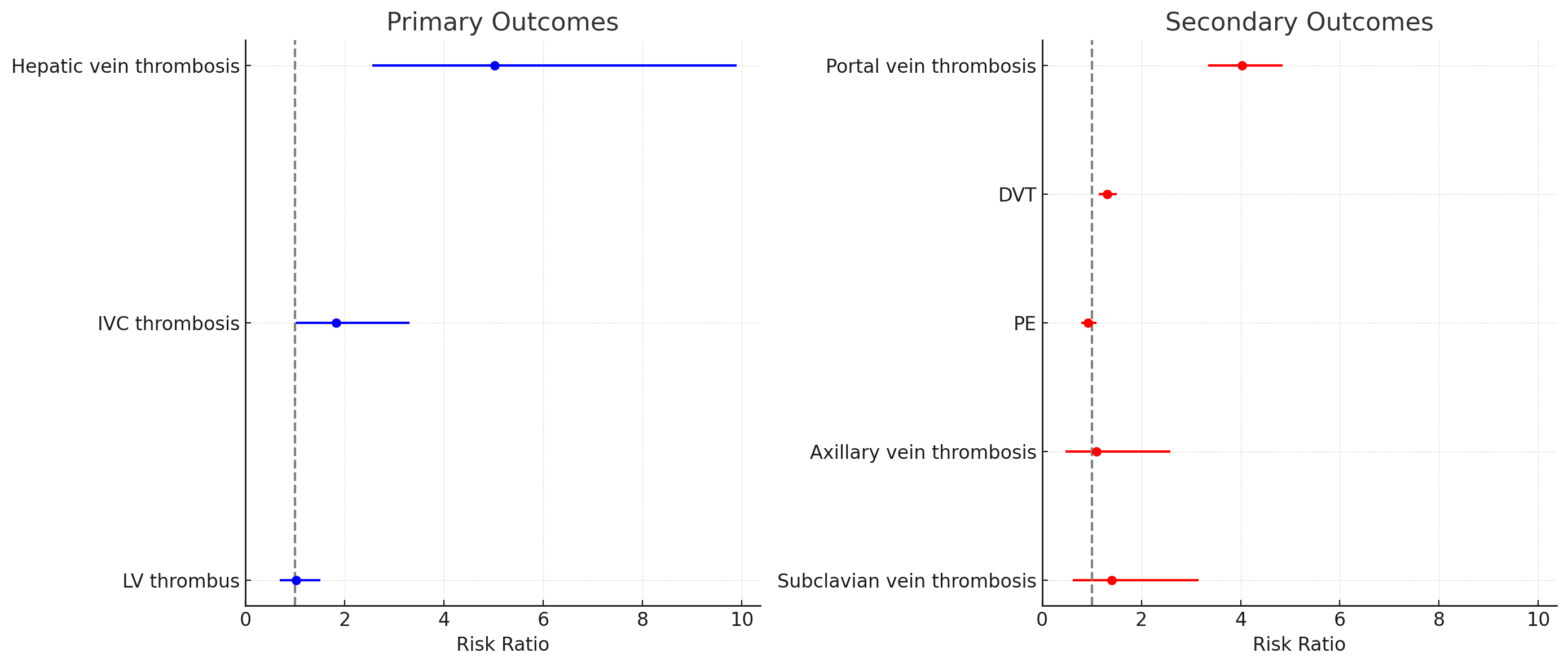
Figure: Figure 1. Forest Plots Comparing Risk Ratios of Thromboembolic Events in Acute Pancreatitis Between Cirrhotic and Non-Cirrhotic Patients
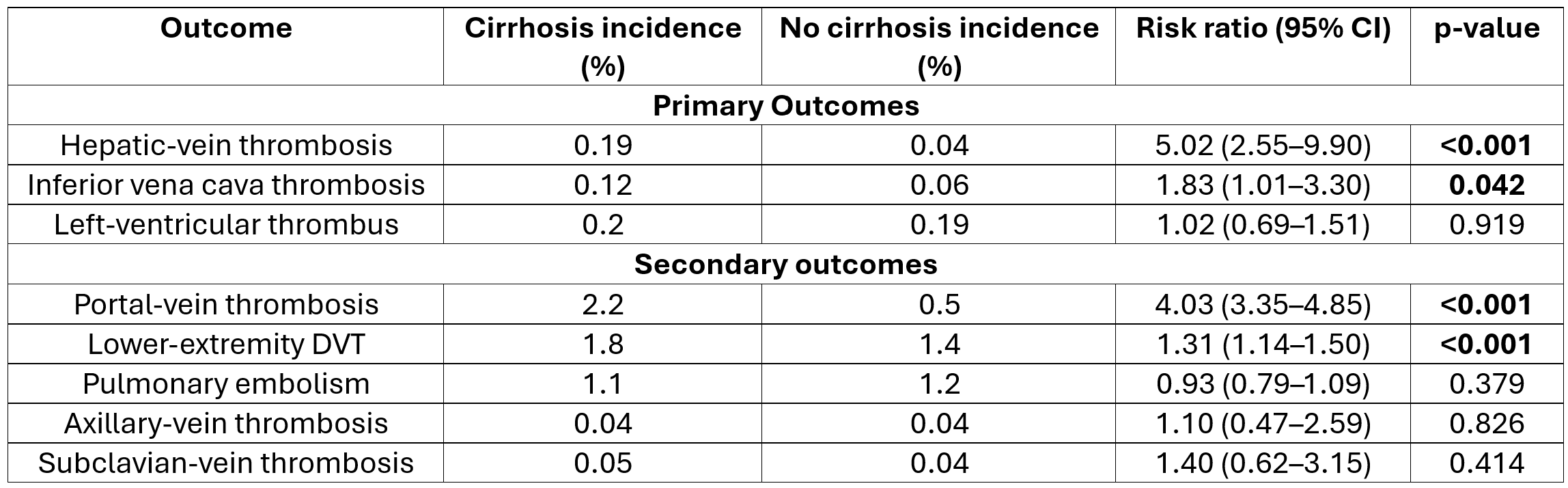
Figure: Table 1. Incidence and Risk Ratios of Thromboembolic Events in Acute Pancreatitis in Patients With Cirrhosis Compared to Those Without Cirrhosis
Disclosures:
Hany Habib indicated no relevant financial relationships.
Kojo-Frimpong B. Awuah indicated no relevant financial relationships.
Somtochukwu Onwuzo indicated no relevant financial relationships.
Kaitlyn Gernhard indicated no relevant financial relationships.
Tyrell Daniel indicated no relevant financial relationships.
Rashid Abdel-Razeq indicated no relevant financial relationships.
Chidera Onwuzo indicated no relevant financial relationships.
Hany Habib, MD1, Kojo-Frimpong B. Awuah, MD2, Somtochukwu Onwuzo, MD3, Kaitlyn Gernhard, DO1, Tyrell Daniel, MD4, Rashid Abdel-Razeq, MD5, Chidera Onwuzo, MBBS6. P1606 - Impact of Cirrhosis on Rare and Common Thromboembolic Events in Acute Pancreatitis: A Propensity-Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
