Sunday Poster Session
Category: Liver
P1601 - Comparative Outcomes of Robotic vs Laparoscopic Liver Resection for Malignancy: An Updated Meta-Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- AK
Aasta Kumari, MD (she/her/hers)
North Central Bronx Hospital
New York, NY
Presenting Author(s)
Aasta Kumari, MD1, Fnu Aakash, MD2, Pinky Bai, MD3, Omer Farooq Mohammed, MBBS4, Sunny Kumar, MD5, Deepak Kumar, MBBS, MD6, Osama Abdur Rehman, MD2, Fnu Arti, MD7, Abdus Sameey Anwar, MBBS8, Miroslav Radulovic, MD9
1North Central Bronx Hospital, New York, NY; 2Florida State University, Cape Coral, FL; 3Howard University Hospital, Washington, DC; 4Osmania General Hospital and Medical College, Hyderabad, Telangana, India; 5Wright Center for Graduate Medical Education, Scranton, PA; 6Northwell Health, Port Jefferson, NY; 7Saint Francis Medical Center, Monroe, LA; 8College of Medical Sciences, Bharatpur, Dhanbad, Jharkhand, India; 9North Central Bronx Hospital, Bronx, NY
Introduction: Surgical resection remains the mainstay treatment for liver malignancies. Recent advances in surgical techniques have introduced robotic-assisted liver resection (RLR) as a viable alternative to conventional laparoscopic liver resection (LLR). Both approaches aim to provide minimally invasive options, but the relative advantages in terms of surgical outcomes, recovery times, and oncological efficacy are still debated. This updated meta-analysis aims to systematically compare the outcomes of RLR and LLR for liver malignancies.
Methods: A comprehensive search was conducted in PubMed, Embase, Google Scholar, ScienceDirect, PLOS ONE, Cochrane databases, and ClinicalTrials.gov up to November 30, 2024. The quality of the included studies was assessed using the Newcastle–Ottawa quality assessment scale and the Cochrane Risk of Bias (RoB) tool. The mean difference with 95% CI was used for continuous variables; risk ratio with 95% CI was used for dichotomous variables; and hazard ratio with 95% CI was used for survival-related variables. Meta-analysis was performed using a random-effects model.
Results: Eight high-quality cohort studies and one RCT with 1785 patients were included (624 and 1161 cases for RLR and LLR, respectively). LLR was associated with a significantly shorter hospital stay compared to RLR (RR 0.46, 95% CI: 0.75 to 0.16, ) and a shorter operating time (RR 26.73, 95% CI: 15.90 to 37.57, ). Other outcomes, including conversion to laparotomy, major morbidity, 5-year overall survival and 5-year disease-free survival, showed no significant differences between the two techniques.
Discussion: LLR demonstrated shorter hospital stay and reduced operating time compared to RLR, with no significant difference in long-term surgical and oncological outcomes. These findings suggest that LLR may be the preferable approach for patients where shorter recovery and operative efficiency are priorities. Further research is needed to explore long-term surgical and oncological outcomes.
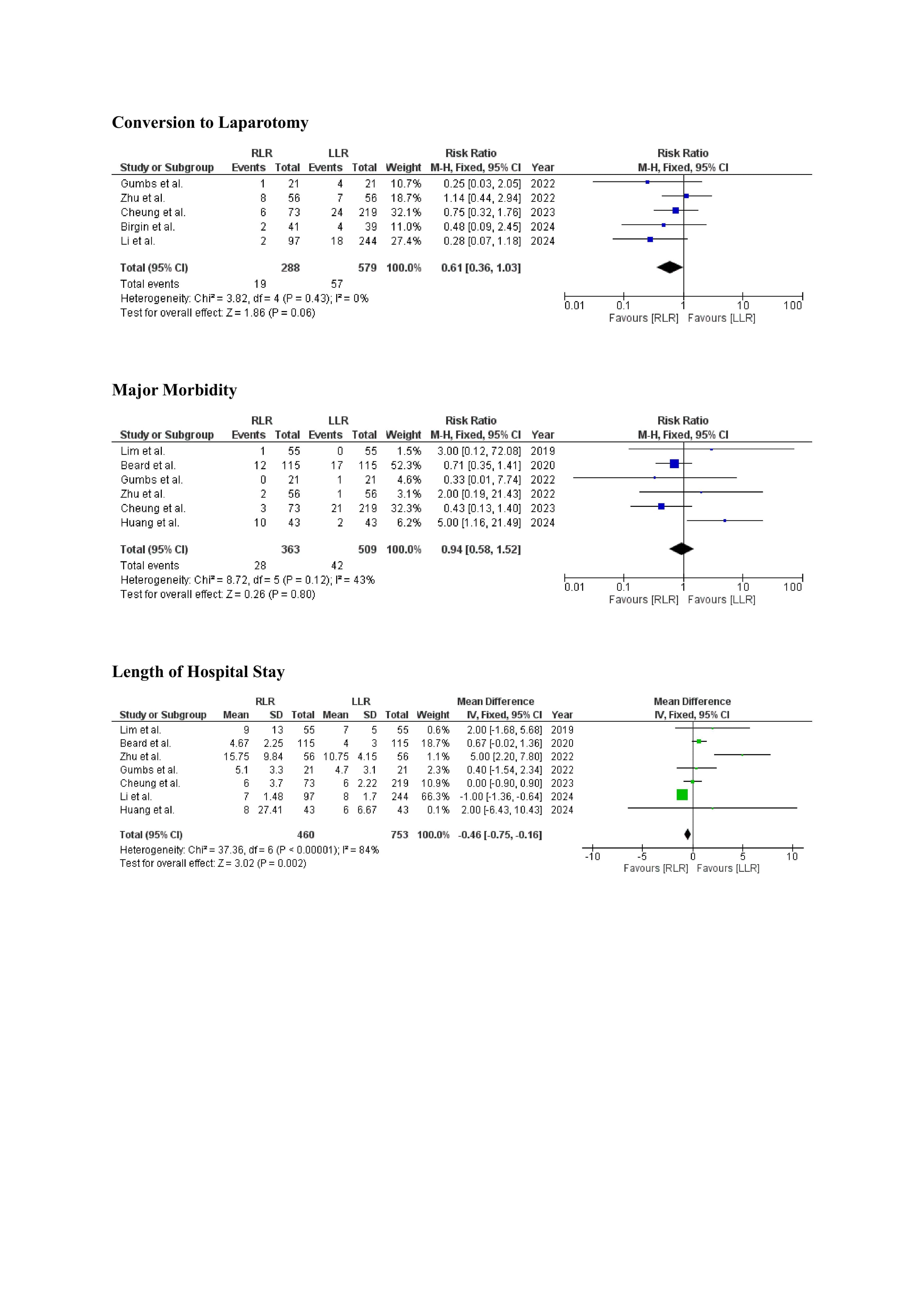
Figure: Figure 1: Forest plots comparing robotic-assisted laparoscopic resection (RLR) with laparoscopic liver resection (LLR) for oncologic and perioperative outcomes.
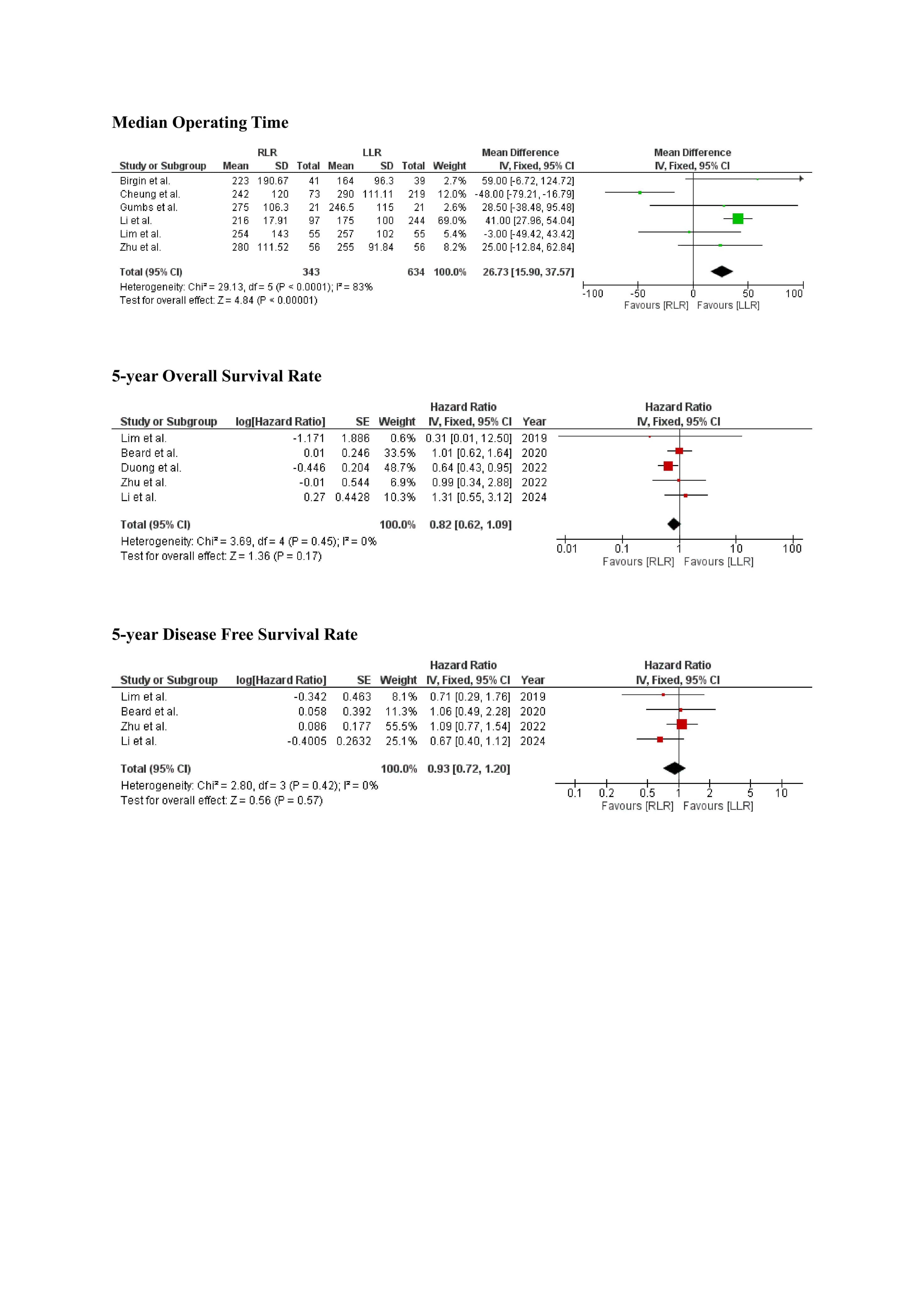
Figure: Figure 2: Forest plots from the meta-analysis comparing robotic-assisted laparoscopic resection (RLR) with laparoscopic liver resection (LLR) for key perioperative outcomes.
Disclosures:
Aasta Kumari indicated no relevant financial relationships.
Fnu Aakash indicated no relevant financial relationships.
Pinky Bai indicated no relevant financial relationships.
Omer Farooq Mohammed indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Deepak Kumar indicated no relevant financial relationships.
Osama Abdur Rehman indicated no relevant financial relationships.
Fnu Arti indicated no relevant financial relationships.
Abdus Sameey Anwar indicated no relevant financial relationships.
Miroslav Radulovic indicated no relevant financial relationships.
Aasta Kumari, MD1, Fnu Aakash, MD2, Pinky Bai, MD3, Omer Farooq Mohammed, MBBS4, Sunny Kumar, MD5, Deepak Kumar, MBBS, MD6, Osama Abdur Rehman, MD2, Fnu Arti, MD7, Abdus Sameey Anwar, MBBS8, Miroslav Radulovic, MD9. P1601 - Comparative Outcomes of Robotic vs Laparoscopic Liver Resection for Malignancy: An Updated Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1North Central Bronx Hospital, New York, NY; 2Florida State University, Cape Coral, FL; 3Howard University Hospital, Washington, DC; 4Osmania General Hospital and Medical College, Hyderabad, Telangana, India; 5Wright Center for Graduate Medical Education, Scranton, PA; 6Northwell Health, Port Jefferson, NY; 7Saint Francis Medical Center, Monroe, LA; 8College of Medical Sciences, Bharatpur, Dhanbad, Jharkhand, India; 9North Central Bronx Hospital, Bronx, NY
Introduction: Surgical resection remains the mainstay treatment for liver malignancies. Recent advances in surgical techniques have introduced robotic-assisted liver resection (RLR) as a viable alternative to conventional laparoscopic liver resection (LLR). Both approaches aim to provide minimally invasive options, but the relative advantages in terms of surgical outcomes, recovery times, and oncological efficacy are still debated. This updated meta-analysis aims to systematically compare the outcomes of RLR and LLR for liver malignancies.
Methods: A comprehensive search was conducted in PubMed, Embase, Google Scholar, ScienceDirect, PLOS ONE, Cochrane databases, and ClinicalTrials.gov up to November 30, 2024. The quality of the included studies was assessed using the Newcastle–Ottawa quality assessment scale and the Cochrane Risk of Bias (RoB) tool. The mean difference with 95% CI was used for continuous variables; risk ratio with 95% CI was used for dichotomous variables; and hazard ratio with 95% CI was used for survival-related variables. Meta-analysis was performed using a random-effects model.
Results: Eight high-quality cohort studies and one RCT with 1785 patients were included (624 and 1161 cases for RLR and LLR, respectively). LLR was associated with a significantly shorter hospital stay compared to RLR (RR 0.46, 95% CI: 0.75 to 0.16, ) and a shorter operating time (RR 26.73, 95% CI: 15.90 to 37.57, ). Other outcomes, including conversion to laparotomy, major morbidity, 5-year overall survival and 5-year disease-free survival, showed no significant differences between the two techniques.
Discussion: LLR demonstrated shorter hospital stay and reduced operating time compared to RLR, with no significant difference in long-term surgical and oncological outcomes. These findings suggest that LLR may be the preferable approach for patients where shorter recovery and operative efficiency are priorities. Further research is needed to explore long-term surgical and oncological outcomes.
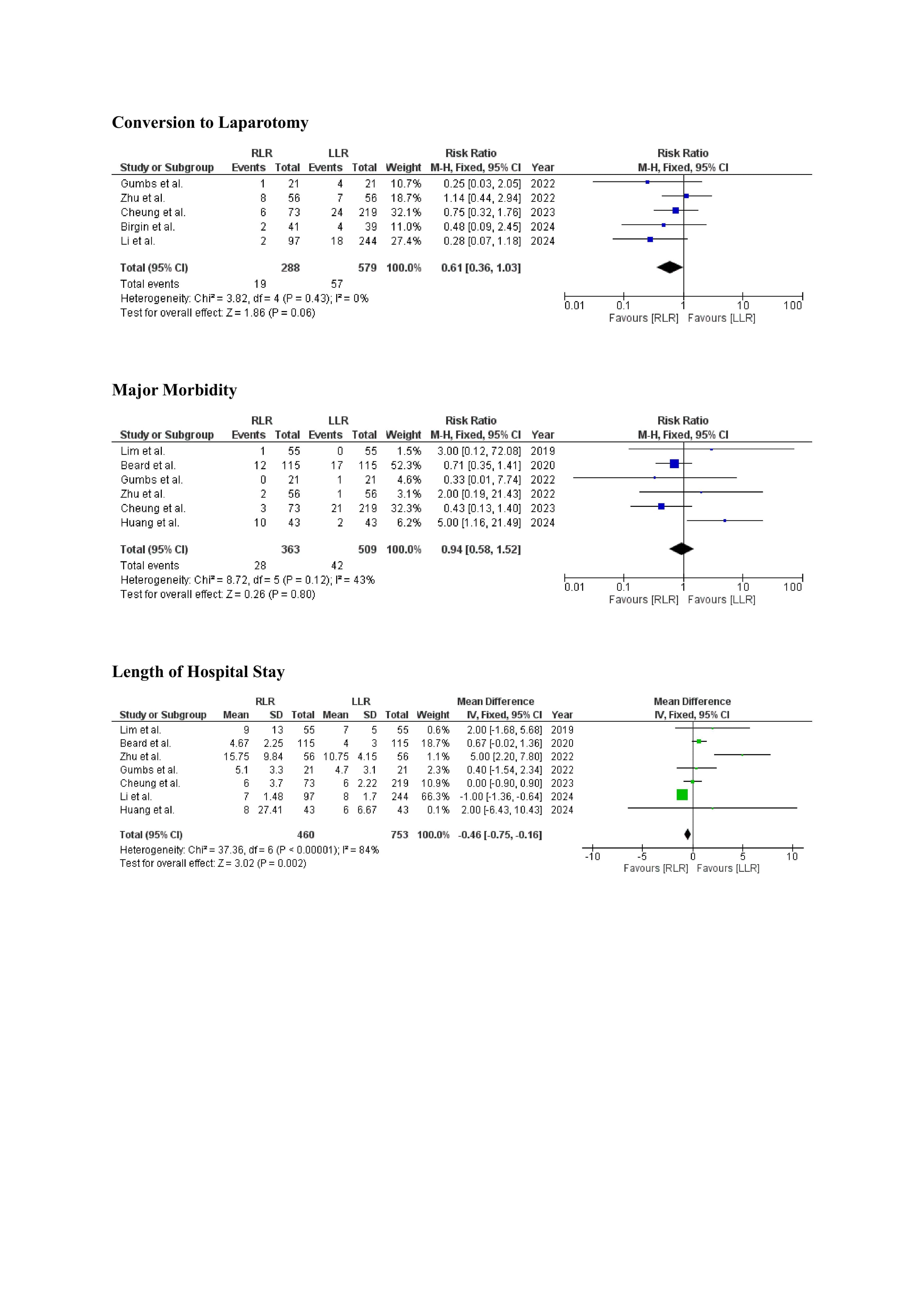
Figure: Figure 1: Forest plots comparing robotic-assisted laparoscopic resection (RLR) with laparoscopic liver resection (LLR) for oncologic and perioperative outcomes.
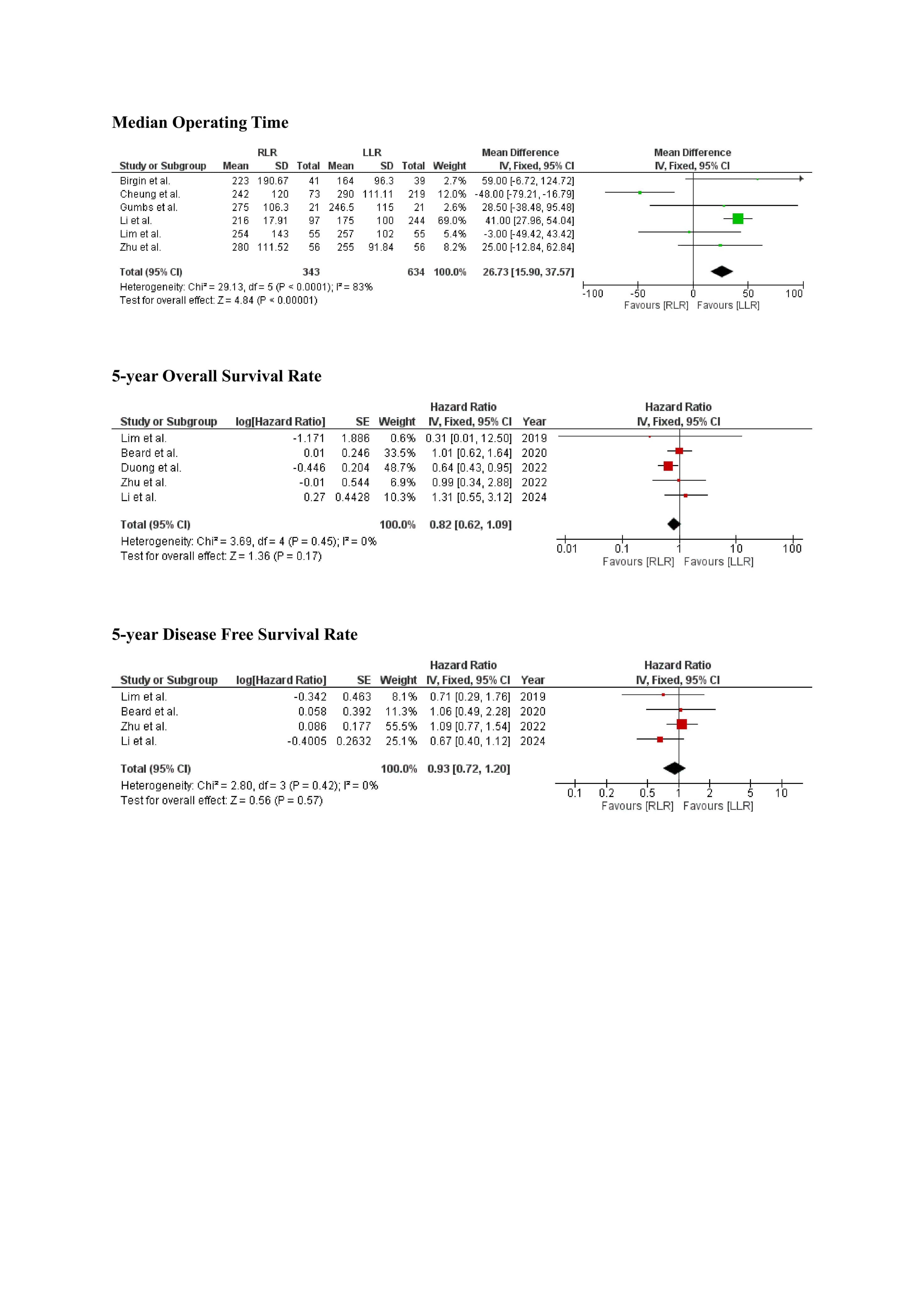
Figure: Figure 2: Forest plots from the meta-analysis comparing robotic-assisted laparoscopic resection (RLR) with laparoscopic liver resection (LLR) for key perioperative outcomes.
Disclosures:
Aasta Kumari indicated no relevant financial relationships.
Fnu Aakash indicated no relevant financial relationships.
Pinky Bai indicated no relevant financial relationships.
Omer Farooq Mohammed indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Deepak Kumar indicated no relevant financial relationships.
Osama Abdur Rehman indicated no relevant financial relationships.
Fnu Arti indicated no relevant financial relationships.
Abdus Sameey Anwar indicated no relevant financial relationships.
Miroslav Radulovic indicated no relevant financial relationships.
Aasta Kumari, MD1, Fnu Aakash, MD2, Pinky Bai, MD3, Omer Farooq Mohammed, MBBS4, Sunny Kumar, MD5, Deepak Kumar, MBBS, MD6, Osama Abdur Rehman, MD2, Fnu Arti, MD7, Abdus Sameey Anwar, MBBS8, Miroslav Radulovic, MD9. P1601 - Comparative Outcomes of Robotic vs Laparoscopic Liver Resection for Malignancy: An Updated Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
