Sunday Poster Session
Category: Liver
P1594 - Missed Opportunities for Noninvasive Fibrosis Risk Stratification in MASLD: A Veteran Population Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Jacky Reny, MD (he/him/his)
Stony Brook University Hospital
Port Jefferson Station, NY
Presenting Author(s)
Jacky Reny, MD1, Jordan Barnett-Kradjian, DO2, Kaustav Patra, MD1, Pallavi Kawatra, BS3, Lisa Fisher, MD4
1Stony Brook University Hospital, Port Jefferson Station, NY; 2Stony Brook Medicine, Stony Brook, NY; 3Philadelphia College of Osteopathic Medicine, Philadelphia, PA; 4Stony Brook University Hospital, Northport, NY
Introduction: Noninvasive fibrosis scores such as Fib-4 and the NAFLD fibrosis score are recommended by major guidelines for risk stratification in MASLD. However, adherence to these recommendations is unclear, and predictors of missed risk stratification have not been well characterized. Understanding care gaps is essential to inform quality improvement initiatives and optimize patient outcomes. We sought to determine the prevalence and predictors of missed noninvasive fibrosis risk stratification in a Veteran MASLD cohort and to identify subpopulations at greatest risk for being overlooked.
Methods: We conducted a retrospective cohort study of 80 adults with MASLD followed at a veteran's affairs hospital. EMR were reviewed for documentation of Fib-4 and/or NAFLD fibrosis score. “Missed risk stratification” was defined as the absence of both a Fib-4 and a NAFLD fibrosis score in the medical record. Clinical variables, including age, BMI, platelet count, ALT, A1c, ASCVD 10-year risk, and type 2 diabetes (T2DM) status, were extracted for all patients. Logistic regression was used to identify independent predictors of missed risk stratification.
Results: Of 80 patients, 21 (26%) had no documented Fib-4 or NAFLD fibrosis score, representing a significant care gap in guideline-recommended MASLD management. Older age was independently associated with higher odds of missed risk stratification (OR per year: 1.14, 95% CI 1.06–1.24, p = 0.001), while T2DM was associated with a dramatically lower risk (OR: 0.02, 95% CI 0.001–0.38, p = 0.009). BMI, platelet count, and ALT were not significantly associated with missed risk stratification. Among patients without risk scores, 18% had laboratory or clinical findings suggestive of advanced fibrosis, indicating potential for missed diagnosis and delayed specialist referral.
Discussion: More than one in four MASLD patients did not undergo noninvasive fibrosis risk stratification, with older adults at the highest risk of being overlooked. In contrast, patients with T2DM were substantially more likely to have been appropriately risk stratified, possibly reflecting targeted screening efforts in this population. These findings highlight the need for system-level interventions to ensure that all MASLD patients receive guideline-recommended risk assessment. Proactive identification and management of care gaps may reduce missed opportunities for early diagnosis and improve long-term liver-related outcomes.
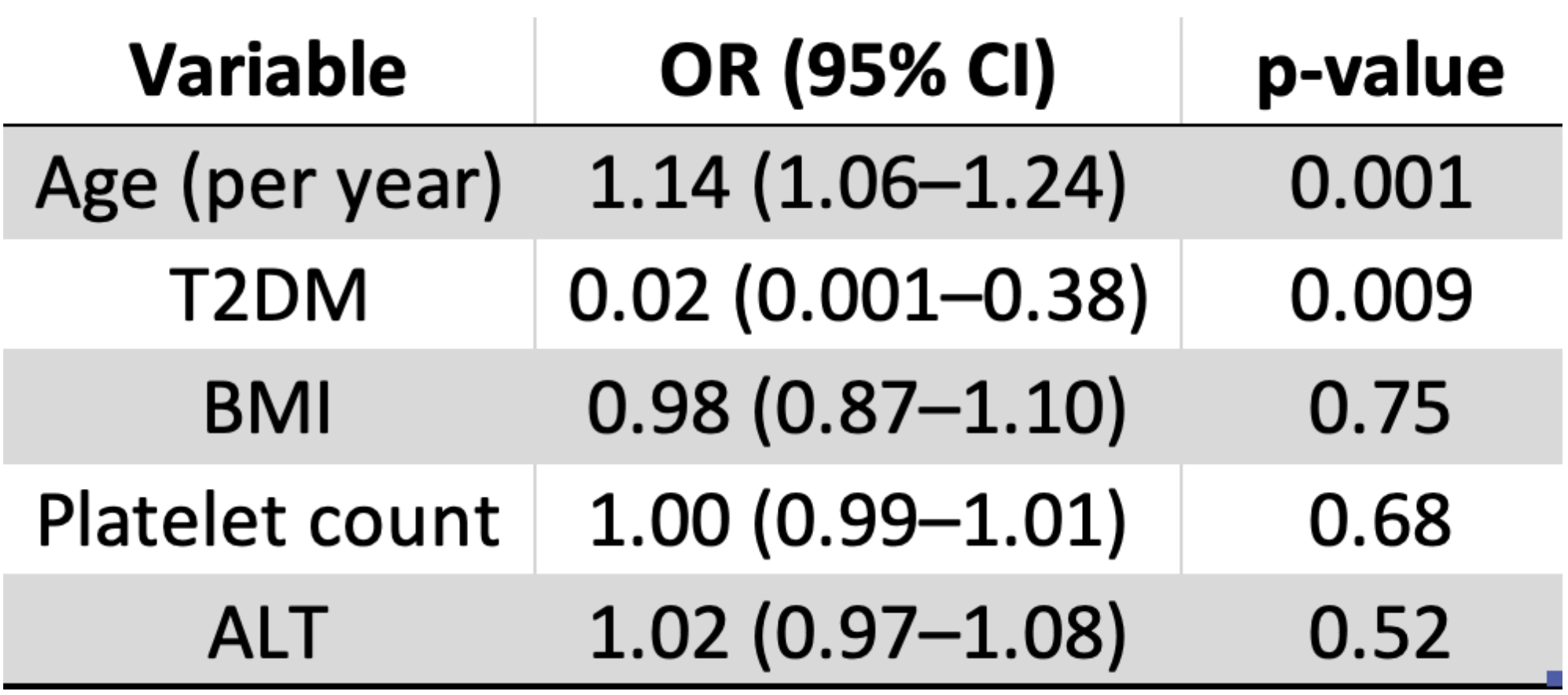
Figure: Predictors of Missed Risk Stratification in MASLD (Logistic Regression Results)
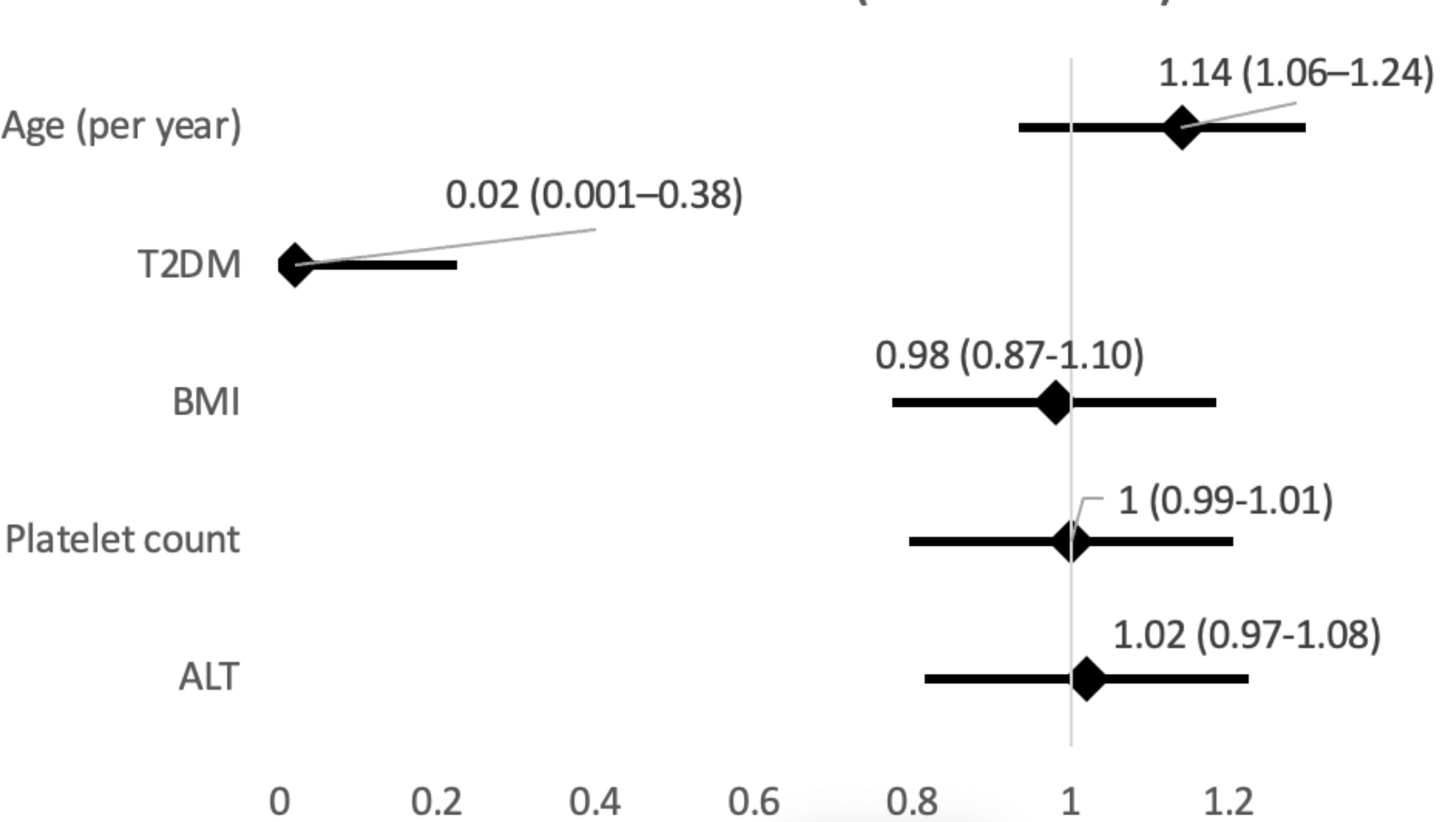
Figure: Predictors for Missed Fibrosis Risk Stratification (OR: 95% CI)
Disclosures:
Jacky Reny indicated no relevant financial relationships.
Jordan Barnett-Kradjian indicated no relevant financial relationships.
Kaustav Patra indicated no relevant financial relationships.
Pallavi Kawatra indicated no relevant financial relationships.
Lisa Fisher indicated no relevant financial relationships.
Jacky Reny, MD1, Jordan Barnett-Kradjian, DO2, Kaustav Patra, MD1, Pallavi Kawatra, BS3, Lisa Fisher, MD4. P1594 - Missed Opportunities for Noninvasive Fibrosis Risk Stratification in MASLD: A Veteran Population Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Stony Brook University Hospital, Port Jefferson Station, NY; 2Stony Brook Medicine, Stony Brook, NY; 3Philadelphia College of Osteopathic Medicine, Philadelphia, PA; 4Stony Brook University Hospital, Northport, NY
Introduction: Noninvasive fibrosis scores such as Fib-4 and the NAFLD fibrosis score are recommended by major guidelines for risk stratification in MASLD. However, adherence to these recommendations is unclear, and predictors of missed risk stratification have not been well characterized. Understanding care gaps is essential to inform quality improvement initiatives and optimize patient outcomes. We sought to determine the prevalence and predictors of missed noninvasive fibrosis risk stratification in a Veteran MASLD cohort and to identify subpopulations at greatest risk for being overlooked.
Methods: We conducted a retrospective cohort study of 80 adults with MASLD followed at a veteran's affairs hospital. EMR were reviewed for documentation of Fib-4 and/or NAFLD fibrosis score. “Missed risk stratification” was defined as the absence of both a Fib-4 and a NAFLD fibrosis score in the medical record. Clinical variables, including age, BMI, platelet count, ALT, A1c, ASCVD 10-year risk, and type 2 diabetes (T2DM) status, were extracted for all patients. Logistic regression was used to identify independent predictors of missed risk stratification.
Results: Of 80 patients, 21 (26%) had no documented Fib-4 or NAFLD fibrosis score, representing a significant care gap in guideline-recommended MASLD management. Older age was independently associated with higher odds of missed risk stratification (OR per year: 1.14, 95% CI 1.06–1.24, p = 0.001), while T2DM was associated with a dramatically lower risk (OR: 0.02, 95% CI 0.001–0.38, p = 0.009). BMI, platelet count, and ALT were not significantly associated with missed risk stratification. Among patients without risk scores, 18% had laboratory or clinical findings suggestive of advanced fibrosis, indicating potential for missed diagnosis and delayed specialist referral.
Discussion: More than one in four MASLD patients did not undergo noninvasive fibrosis risk stratification, with older adults at the highest risk of being overlooked. In contrast, patients with T2DM were substantially more likely to have been appropriately risk stratified, possibly reflecting targeted screening efforts in this population. These findings highlight the need for system-level interventions to ensure that all MASLD patients receive guideline-recommended risk assessment. Proactive identification and management of care gaps may reduce missed opportunities for early diagnosis and improve long-term liver-related outcomes.
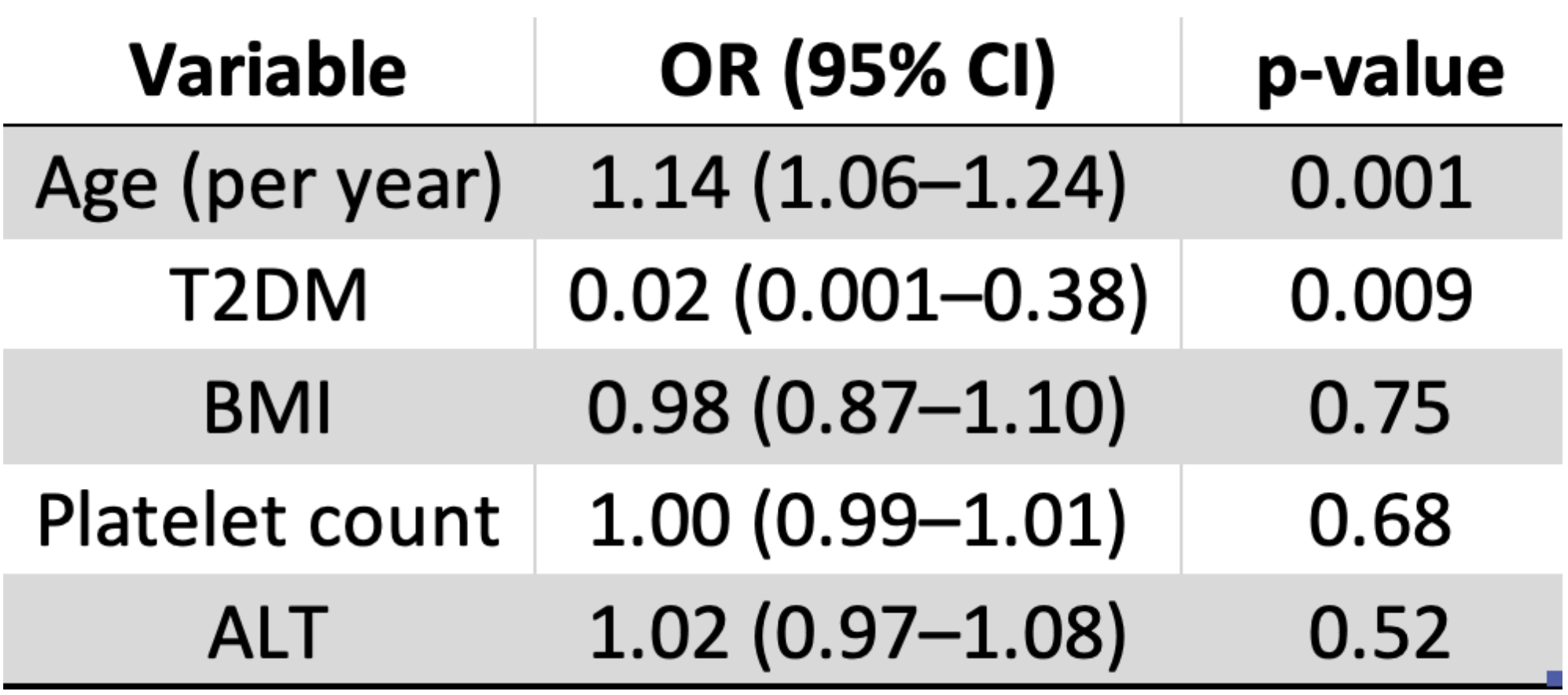
Figure: Predictors of Missed Risk Stratification in MASLD (Logistic Regression Results)
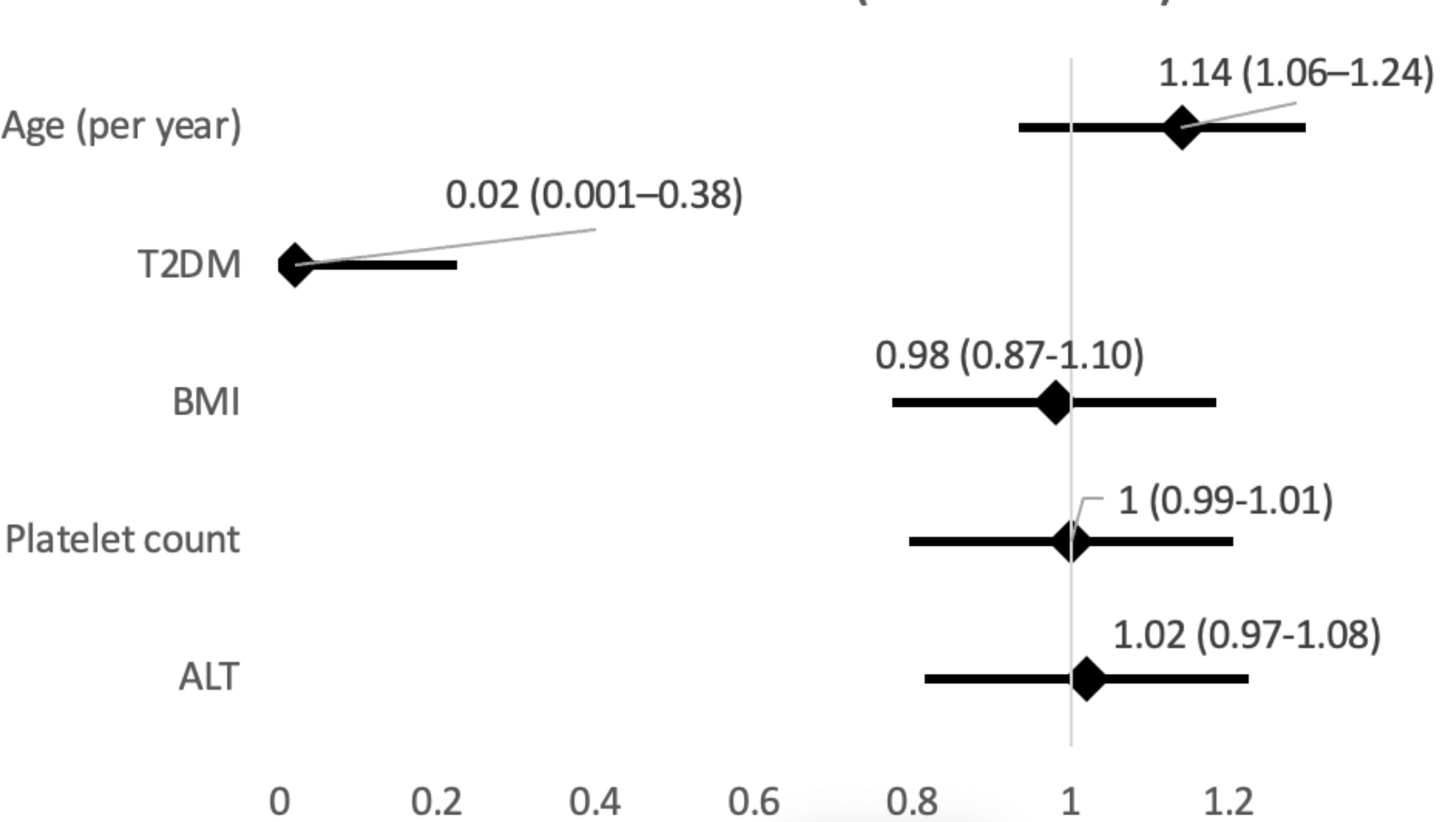
Figure: Predictors for Missed Fibrosis Risk Stratification (OR: 95% CI)
Disclosures:
Jacky Reny indicated no relevant financial relationships.
Jordan Barnett-Kradjian indicated no relevant financial relationships.
Kaustav Patra indicated no relevant financial relationships.
Pallavi Kawatra indicated no relevant financial relationships.
Lisa Fisher indicated no relevant financial relationships.
Jacky Reny, MD1, Jordan Barnett-Kradjian, DO2, Kaustav Patra, MD1, Pallavi Kawatra, BS3, Lisa Fisher, MD4. P1594 - Missed Opportunities for Noninvasive Fibrosis Risk Stratification in MASLD: A Veteran Population Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
