Sunday Poster Session
Category: Liver
P1571 - The Impact of MELD 3.0 Score Severity in Cirrhotic Patients on Cardiac Structure and Function Based on ECG and Echocardiogram Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- IA
Ishan Abdullah, BS (he/him/his)
The George Washington University School of Medicine and Health Sciences
Washington, DC
Presenting Author(s)
Ishan Abdullah, BS1, Omar Saadi, BS1, Abdelrhman Refaey, MD2, Ahmed Attia, MD3, Mohammed Zohery, BS1, Fatma Mokhtar, MD4, Ameer Abutaleb, MD5, Marco Mercader, MD6
1The George Washington University School of Medicine and Health Sciences, Washington, DC; 2Division of Gastroenterology and Liver Disease, Department of Medicine, George Washington University School of Medicine and Health Sciences, Washington, DC; 3Transplant Institute, Department of Surgery, George Washington University School of Medicine and Health Science, Washington, DC; 4he George Washington Transplant Institute, Department of Surgery, The George Washington University Hospital, Washington, DC; 5The George Washington Transplant Institute, Department of Surgery, The George Washington University Hospital, Washington, DC; 6Department of Cardiology, The George Washington University School of Medicine and Health Sciences, Washington, DC
Introduction: Liver cirrhosis is recognized as a contributor to cardiovascular dysfunction, including impaired cardiac function and conduction abnormalities. While ECG findings such as QRS voltage attenuation are commonly reported, their relationship to liver disease severity is unclear. Prior studies suggest that ECG parameters in cirrhotic patients may be affected by fluid distribution. This study examines the association between the MELD 3.0 score and both cardiac dysfunction and ECG abnormalities in cirrhotic patients.
Methods: We analyzed 156 cirrhotic patients with available ECGs. MELD 3.0 scores, calculated using labs within two weeks of ECG acquisition, categorized into three groups (< 10, 10–19, ≥20). QRS voltages and intervals (PR, QTc) were manually measured using EP Calipers. One-way ANOVA was used to compare ECG and cardiac functional parameters, such as left ventricular (LV) ejection fraction, across MELD groups. We used correlational and multiple linear regression analyses to assess the relationship between MELD 3.0 scores and QRS voltages in limb and precordial leads. These analyses also evaluated the independent effects of fluid distribution, specifically peripheral edema and ascites, on voltage changes.
Results: Cryptogenic cirrhosis was the most etiology. Higher MELD 3.0 scores were associated with lower LV ejection fraction (p=0.018), a higher prevalence of atrial fibrillation (p=0.013), T-wave abnormalities (p=0.033), and LV hypertrophy (p=0.037). QRS amplitude in lead aVR declined with increasing MELD 3.0 severity (p=0.05). While QRS voltages in precordial and limb leads showed weak negative correlations with MELD 3.0, these were not statistically significant. Adjusting for ascites modestly improved the correlation in limb leads (p=0.035), but no clear trends emerged across lead types or fluid distribution patterns.
Discussion: Higher MELD 3.0 scores were significantly associated with both structural (LV dysfunction, hypertrophy) and electrophysiological (arrhythmias, repolarization abnormalities) cardiac changes. These findings align with prior studies suggesting that worsening liver disease, as measured by earlier versions of the MELD and Child-Pugh scores, contributes to cardiac dysfunction. Although QRS voltage attenuation was observed, it showed a weak negative correlation with MELD 3.0 and appeared unaffected by fluid distribution. This suggests that intrinsic myocardial dysfunction, rather than fluid-related factors, may underlie the ECG abnormalities in advanced cirrhosis.
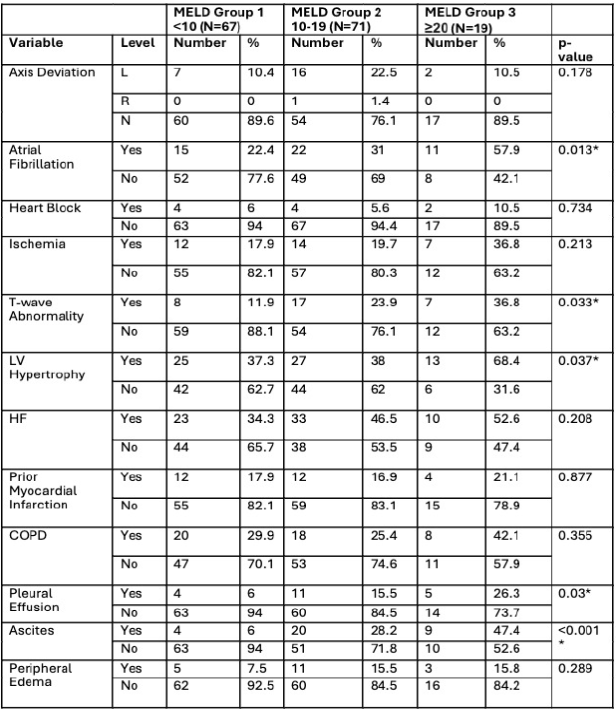
Figure: Prevalence of Cardiac Abnormalities and Fluid Distribution Findings by MELD 3.0 Group
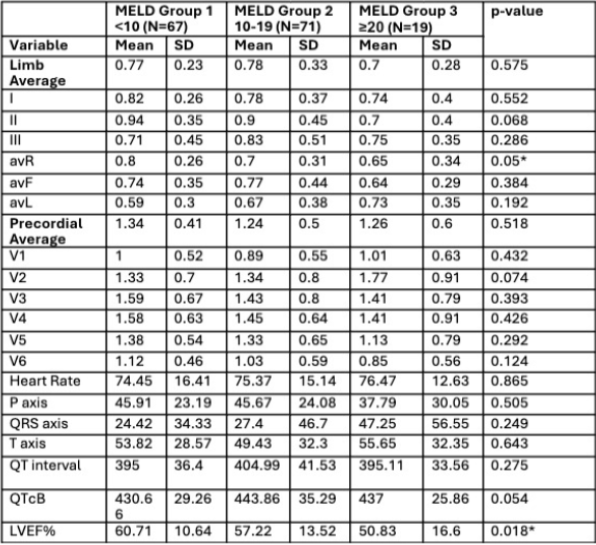
Figure: Electrocardiographic and Echocardiographic Parameters Across MELD 3.0 Severity Groups
Disclosures:
Ishan Abdullah indicated no relevant financial relationships.
Omar Saadi indicated no relevant financial relationships.
Abdelrhman Refaey indicated no relevant financial relationships.
Ahmed Attia indicated no relevant financial relationships.
Mohammed Zohery indicated no relevant financial relationships.
Fatma Mokhtar indicated no relevant financial relationships.
Ameer Abutaleb indicated no relevant financial relationships.
Marco Mercader indicated no relevant financial relationships.
Ishan Abdullah, BS1, Omar Saadi, BS1, Abdelrhman Refaey, MD2, Ahmed Attia, MD3, Mohammed Zohery, BS1, Fatma Mokhtar, MD4, Ameer Abutaleb, MD5, Marco Mercader, MD6. P1571 - The Impact of MELD 3.0 Score Severity in Cirrhotic Patients on Cardiac Structure and Function Based on ECG and Echocardiogram Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1The George Washington University School of Medicine and Health Sciences, Washington, DC; 2Division of Gastroenterology and Liver Disease, Department of Medicine, George Washington University School of Medicine and Health Sciences, Washington, DC; 3Transplant Institute, Department of Surgery, George Washington University School of Medicine and Health Science, Washington, DC; 4he George Washington Transplant Institute, Department of Surgery, The George Washington University Hospital, Washington, DC; 5The George Washington Transplant Institute, Department of Surgery, The George Washington University Hospital, Washington, DC; 6Department of Cardiology, The George Washington University School of Medicine and Health Sciences, Washington, DC
Introduction: Liver cirrhosis is recognized as a contributor to cardiovascular dysfunction, including impaired cardiac function and conduction abnormalities. While ECG findings such as QRS voltage attenuation are commonly reported, their relationship to liver disease severity is unclear. Prior studies suggest that ECG parameters in cirrhotic patients may be affected by fluid distribution. This study examines the association between the MELD 3.0 score and both cardiac dysfunction and ECG abnormalities in cirrhotic patients.
Methods: We analyzed 156 cirrhotic patients with available ECGs. MELD 3.0 scores, calculated using labs within two weeks of ECG acquisition, categorized into three groups (< 10, 10–19, ≥20). QRS voltages and intervals (PR, QTc) were manually measured using EP Calipers. One-way ANOVA was used to compare ECG and cardiac functional parameters, such as left ventricular (LV) ejection fraction, across MELD groups. We used correlational and multiple linear regression analyses to assess the relationship between MELD 3.0 scores and QRS voltages in limb and precordial leads. These analyses also evaluated the independent effects of fluid distribution, specifically peripheral edema and ascites, on voltage changes.
Results: Cryptogenic cirrhosis was the most etiology. Higher MELD 3.0 scores were associated with lower LV ejection fraction (p=0.018), a higher prevalence of atrial fibrillation (p=0.013), T-wave abnormalities (p=0.033), and LV hypertrophy (p=0.037). QRS amplitude in lead aVR declined with increasing MELD 3.0 severity (p=0.05). While QRS voltages in precordial and limb leads showed weak negative correlations with MELD 3.0, these were not statistically significant. Adjusting for ascites modestly improved the correlation in limb leads (p=0.035), but no clear trends emerged across lead types or fluid distribution patterns.
Discussion: Higher MELD 3.0 scores were significantly associated with both structural (LV dysfunction, hypertrophy) and electrophysiological (arrhythmias, repolarization abnormalities) cardiac changes. These findings align with prior studies suggesting that worsening liver disease, as measured by earlier versions of the MELD and Child-Pugh scores, contributes to cardiac dysfunction. Although QRS voltage attenuation was observed, it showed a weak negative correlation with MELD 3.0 and appeared unaffected by fluid distribution. This suggests that intrinsic myocardial dysfunction, rather than fluid-related factors, may underlie the ECG abnormalities in advanced cirrhosis.
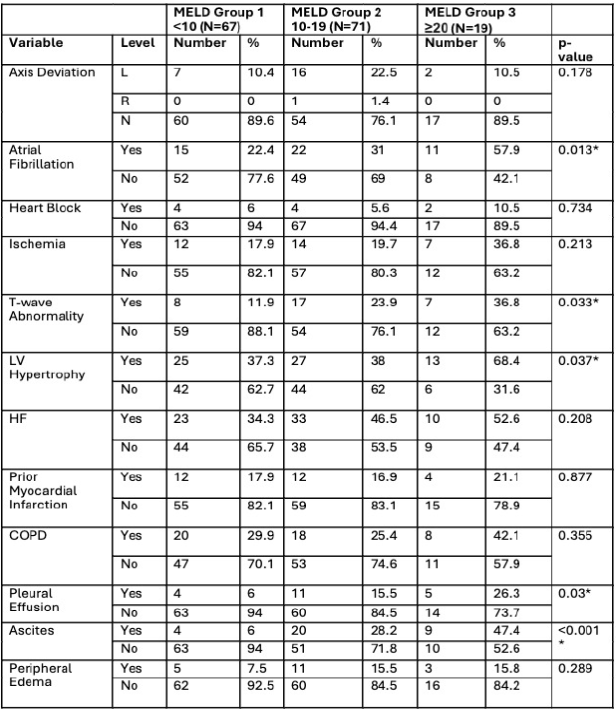
Figure: Prevalence of Cardiac Abnormalities and Fluid Distribution Findings by MELD 3.0 Group
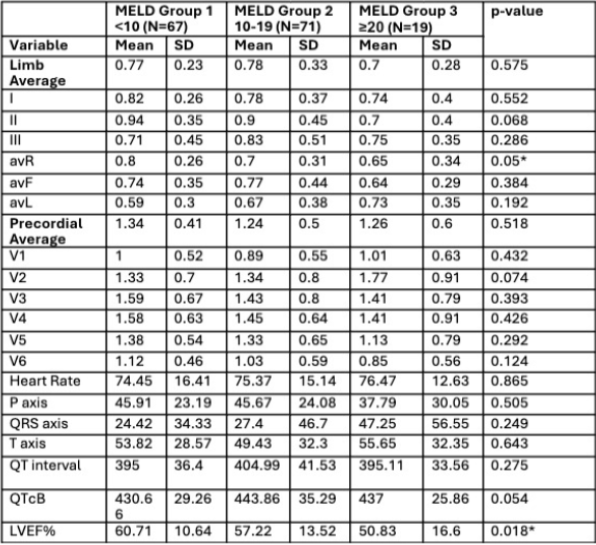
Figure: Electrocardiographic and Echocardiographic Parameters Across MELD 3.0 Severity Groups
Disclosures:
Ishan Abdullah indicated no relevant financial relationships.
Omar Saadi indicated no relevant financial relationships.
Abdelrhman Refaey indicated no relevant financial relationships.
Ahmed Attia indicated no relevant financial relationships.
Mohammed Zohery indicated no relevant financial relationships.
Fatma Mokhtar indicated no relevant financial relationships.
Ameer Abutaleb indicated no relevant financial relationships.
Marco Mercader indicated no relevant financial relationships.
Ishan Abdullah, BS1, Omar Saadi, BS1, Abdelrhman Refaey, MD2, Ahmed Attia, MD3, Mohammed Zohery, BS1, Fatma Mokhtar, MD4, Ameer Abutaleb, MD5, Marco Mercader, MD6. P1571 - The Impact of MELD 3.0 Score Severity in Cirrhotic Patients on Cardiac Structure and Function Based on ECG and Echocardiogram Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
