Sunday Poster Session
Category: Liver
P1569 - Flood Syndrome: A Systematic Review of Reported Cases and Management Outcomes
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Ismail Elkhattib, MBBCh
University of Nebraska
Hartford, CT
Presenting Author(s)
Ismail Elkhattib, MBBCh1, Bishoy Fahim, MBBCh2, Abanoub Mokhles, MBBCh3, Alaa Adrabou Abouelmagd, 4, Mohamed E. Haseeb, MBBCh5, George Karas, MBBCh6, Mohamed Yasser Elnaggar, MBBCH, MSc7, Mohamed A. Aldemerdash, 8, Mohamed A. B. Elnaggar, MD9
1University of Nebraska, Hartford, CT; 2Sohag University Hospital, Sohag, Suhaj, Egypt; 3University of Sohag, Cairo, Suhaj, Egypt; 4South Valley University, South Valley, Qina, Egypt; 5Minia University, Minia, Al Minya, Egypt; 6University of Sohag, Sohag, Suhaj, Egypt; 7Mansoura University, Mansoura, Ad Daqahliyah, Egypt; 8Sohag University, Faculty of Medicine, Sohag, Suhaj, Egypt; 9Hartford Healthcare, Hartford, CT
Introduction: Flood syndrome is a rare but life-threatening condition that occurs in patients with end-stage liver disease complicated by umbilical hernia, especially those with large-volume ascites. Umbilical hernias are seen in up to 20% of cirrhotic patients with ascites. In some patients, spontaneous rupture of an umbilical hernia leads to a sudden and significant ascitic fluid leakage. Managing Flood syndrome remains a challenge, as there is no clear or standardized treatment. Some reports suggest that elective hernia repair in cirrhotic patients lowers the 30-day mortality rate, around 1.2%, compared to emergency surgery, which may have a rate as high as 12.2%
Methods: For this systematic review, we searched PubMed, Scopus, Web of Science, and Embase until April 2025 to identify relevant case reports or case series on flood syndrome. We found a total of 60 relevant publications. From these, we collected and reviewed information on patient age, symptoms, the method of diagnosis, treatment approaches, and patient outcomes
Results: A total of 60 studies were included, representing approximately 142 cases of Flood syndrome. The mean age of the patients was 53.82 ± 12.10 years, with a slight male predominance (65.8%). 76 patients (52%) presented with spontaneous rupture of an umbilical hernia accompanied by ascitic fluid leak; the remaining presented with abdominal swelling with skin ulceration. All patients received medical management, Additionally, 21 patients underwent paracentesis. Eighty-four patients (57.53%) underwent surgical repair of the hernial defect, the remaining patients were managed with minimally invasive techniques. There were 11 cases (7.5%) of recurrent umbilical hernia reported after management. Mortality was noted in 20 patients (13.7%), 14 of whom (9.6%) had undergone surgical repair
Discussion: Flood syndrome is associated with significant morbidity and mortality, especially in patients who underwent emergency surgery. Elective hernia repair in patients with stable liver function and controlled ascites has, however, shown lower death rates, particularly when performed laparoscopically. These findings support the need to reconsider current management and examine whether earlier elective intervention could prevent rupture and improve mortality rates. Further research is necessary to create clear guidelines on when surgical repair is appropriate and which patients are suitable to prevent this life-threatening complication
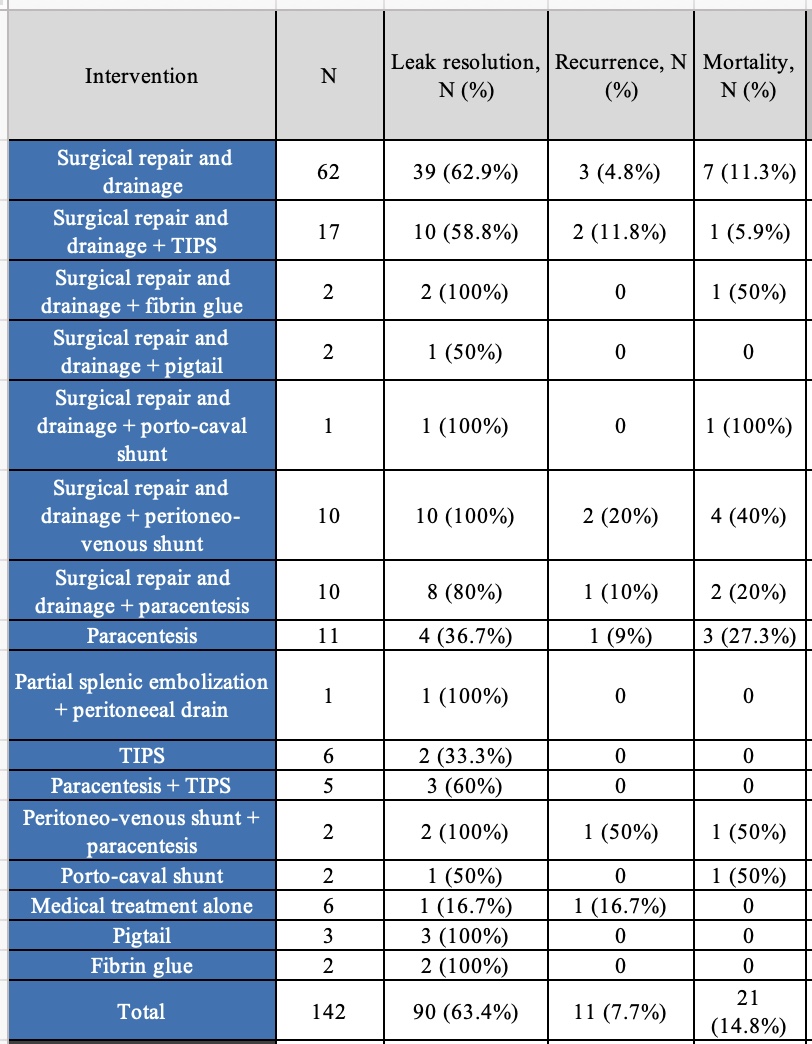
Figure: Table 1: Management outcomes in 142 reported cases of Flood syndrome
Disclosures:
Ismail Elkhattib indicated no relevant financial relationships.
Bishoy Fahim indicated no relevant financial relationships.
Abanoub Mokhles indicated no relevant financial relationships.
Alaa Adrabou Abouelmagd indicated no relevant financial relationships.
Mohamed E. Haseeb indicated no relevant financial relationships.
George Karas indicated no relevant financial relationships.
Mohamed Yasser Elnaggar indicated no relevant financial relationships.
Mohamed A. Aldemerdash indicated no relevant financial relationships.
Mohamed A. Elnaggar indicated no relevant financial relationships.
Ismail Elkhattib, MBBCh1, Bishoy Fahim, MBBCh2, Abanoub Mokhles, MBBCh3, Alaa Adrabou Abouelmagd, 4, Mohamed E. Haseeb, MBBCh5, George Karas, MBBCh6, Mohamed Yasser Elnaggar, MBBCH, MSc7, Mohamed A. Aldemerdash, 8, Mohamed A. B. Elnaggar, MD9. P1569 - Flood Syndrome: A Systematic Review of Reported Cases and Management Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Nebraska, Hartford, CT; 2Sohag University Hospital, Sohag, Suhaj, Egypt; 3University of Sohag, Cairo, Suhaj, Egypt; 4South Valley University, South Valley, Qina, Egypt; 5Minia University, Minia, Al Minya, Egypt; 6University of Sohag, Sohag, Suhaj, Egypt; 7Mansoura University, Mansoura, Ad Daqahliyah, Egypt; 8Sohag University, Faculty of Medicine, Sohag, Suhaj, Egypt; 9Hartford Healthcare, Hartford, CT
Introduction: Flood syndrome is a rare but life-threatening condition that occurs in patients with end-stage liver disease complicated by umbilical hernia, especially those with large-volume ascites. Umbilical hernias are seen in up to 20% of cirrhotic patients with ascites. In some patients, spontaneous rupture of an umbilical hernia leads to a sudden and significant ascitic fluid leakage. Managing Flood syndrome remains a challenge, as there is no clear or standardized treatment. Some reports suggest that elective hernia repair in cirrhotic patients lowers the 30-day mortality rate, around 1.2%, compared to emergency surgery, which may have a rate as high as 12.2%
Methods: For this systematic review, we searched PubMed, Scopus, Web of Science, and Embase until April 2025 to identify relevant case reports or case series on flood syndrome. We found a total of 60 relevant publications. From these, we collected and reviewed information on patient age, symptoms, the method of diagnosis, treatment approaches, and patient outcomes
Results: A total of 60 studies were included, representing approximately 142 cases of Flood syndrome. The mean age of the patients was 53.82 ± 12.10 years, with a slight male predominance (65.8%). 76 patients (52%) presented with spontaneous rupture of an umbilical hernia accompanied by ascitic fluid leak; the remaining presented with abdominal swelling with skin ulceration. All patients received medical management, Additionally, 21 patients underwent paracentesis. Eighty-four patients (57.53%) underwent surgical repair of the hernial defect, the remaining patients were managed with minimally invasive techniques. There were 11 cases (7.5%) of recurrent umbilical hernia reported after management. Mortality was noted in 20 patients (13.7%), 14 of whom (9.6%) had undergone surgical repair
Discussion: Flood syndrome is associated with significant morbidity and mortality, especially in patients who underwent emergency surgery. Elective hernia repair in patients with stable liver function and controlled ascites has, however, shown lower death rates, particularly when performed laparoscopically. These findings support the need to reconsider current management and examine whether earlier elective intervention could prevent rupture and improve mortality rates. Further research is necessary to create clear guidelines on when surgical repair is appropriate and which patients are suitable to prevent this life-threatening complication
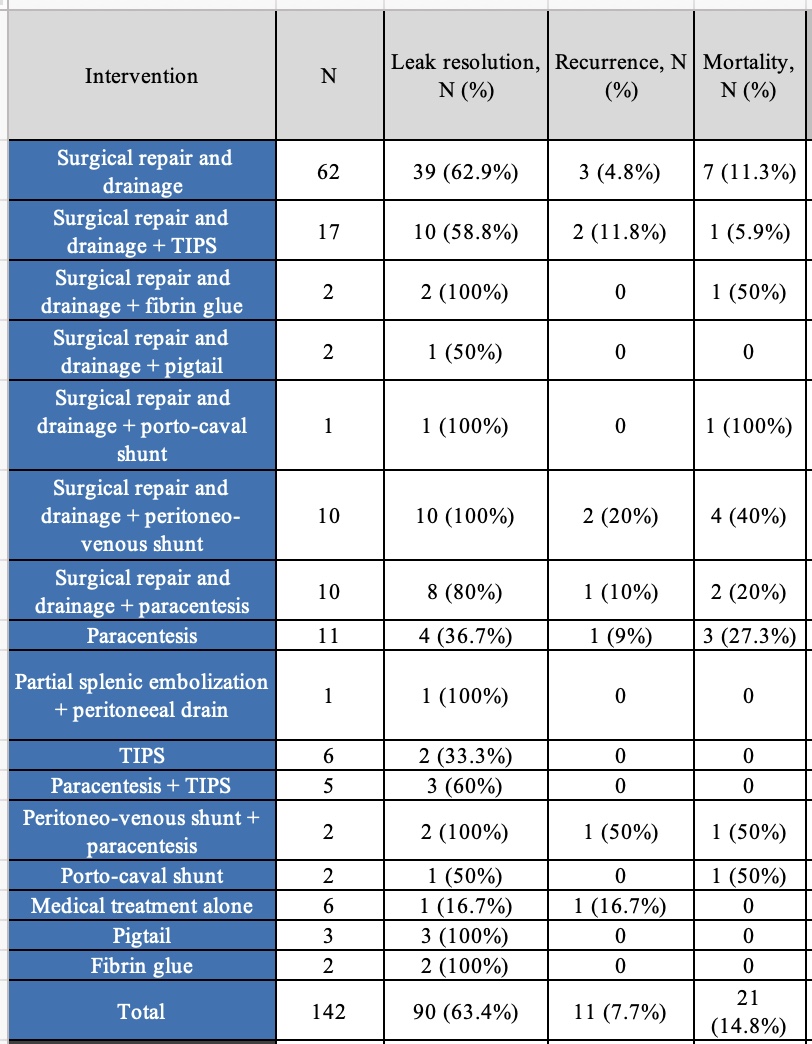
Figure: Table 1: Management outcomes in 142 reported cases of Flood syndrome
Disclosures:
Ismail Elkhattib indicated no relevant financial relationships.
Bishoy Fahim indicated no relevant financial relationships.
Abanoub Mokhles indicated no relevant financial relationships.
Alaa Adrabou Abouelmagd indicated no relevant financial relationships.
Mohamed E. Haseeb indicated no relevant financial relationships.
George Karas indicated no relevant financial relationships.
Mohamed Yasser Elnaggar indicated no relevant financial relationships.
Mohamed A. Aldemerdash indicated no relevant financial relationships.
Mohamed A. Elnaggar indicated no relevant financial relationships.
Ismail Elkhattib, MBBCh1, Bishoy Fahim, MBBCh2, Abanoub Mokhles, MBBCh3, Alaa Adrabou Abouelmagd, 4, Mohamed E. Haseeb, MBBCh5, George Karas, MBBCh6, Mohamed Yasser Elnaggar, MBBCH, MSc7, Mohamed A. Aldemerdash, 8, Mohamed A. B. Elnaggar, MD9. P1569 - Flood Syndrome: A Systematic Review of Reported Cases and Management Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
