Sunday Poster Session
Category: Liver
P1536 - Risk-Benefit Analysis of Therapeutic Anticoagulation in Liver Cirrhosis: A Large-Scale Cohort Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Randa Albloushy, MD (she/her/hers)
University Hospitals Cleveland Medical Center, Case Western Reserve University
Cleveland, OH
Presenting Author(s)
Abdulrahman Ibn Awadh, MD1, Randa Albloushy, MD1, Jaime A. Perez, PhD1, Apoorva K. Chandar, MBBS, MPH2, Resham Ramkissoon, MD3
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 3university Hospitals Cleveland Medical Center, Case Western Reserve, Cleveland, OH
Introduction: Therapeutic anticoagulation (AC) in patients with cirrhosis presents a challenging clinical dilemma. While variceal hemorrhage contributes significantly to morbidity and mortality, concurrent thrombotic conditions may necessitate anticoagulation, raising significant safety concerns. This study evaluates anticoagulation outcomes in cirrhotic patients with venous thromboembolism (VTE), portal vein thrombosis (PVT), or atrial fibrillation/flutter (AF) using a large national dataset.
Methods: We accessed data through a large-scale, de-identified health research network encompassing 102 healthcare organizations across the United States, representing over 150 million patients (TriNetX, Cambridge, MA). We analyzed AC safety in patients with cirrhosis and VTE, PVT, or AF. Patients were stratified into two groups: [1] those receiving AC within one month of VTE, PVT, or AF diagnosis and [2] those not receiving AC. Specific ICD-10 codes defined cirrhosis, VTE, PVT, and AF, requiring at least two documented cirrhosis diagnoses. Patients with hepatocellular carcinoma and bleeding disorders were excluded. Propensity score matching balanced patient cohorts based on demographics, comorbidities, and medications. Outcomes were assessed at 90 days.
Results: After matching, both groups were well-balanced with average age of 64 years, predominantly male (59%), and similar comorbidity profiles including hypertension (54–56%), diabetes (34%), and heart failure (24%). At 90 days, the AC group demonstrated lower variceal hemorrhage incidence (0.6% vs 0.9%, p=0.032) but higher overall gastrointestinal bleeding (3.7% vs 3.1%, p=0.013). Significantly more blood transfusions were required in the AC group (7.4% vs 3.8%, p< 0.001), with higher rates of severe anemia (9.1% vs 5.2%, p< 0.001) and spontaneous bacterial peritonitis (1.1% vs 0.8%, p=0.011). No significant difference in 90-day mortality was observed (12.5% vs 12.7%, p=0.505). Among AC patients, INR ≥2.0 was associated with significantly higher 90-day mortality versus INR < 2.0 (21.6% vs 16.8%, p=0.040).
Discussion: AC in cirrhotic patients requires careful risk-benefit assessment. While AC patients experienced reduced variceal bleeding, they faced increased transfusion requirements, severe anemia, and infectious complications. Most concerning, INR ≥2.0 was associated with significantly higher mortality, emphasizing the need for individualized decision-making and enhanced monitoring strategies.
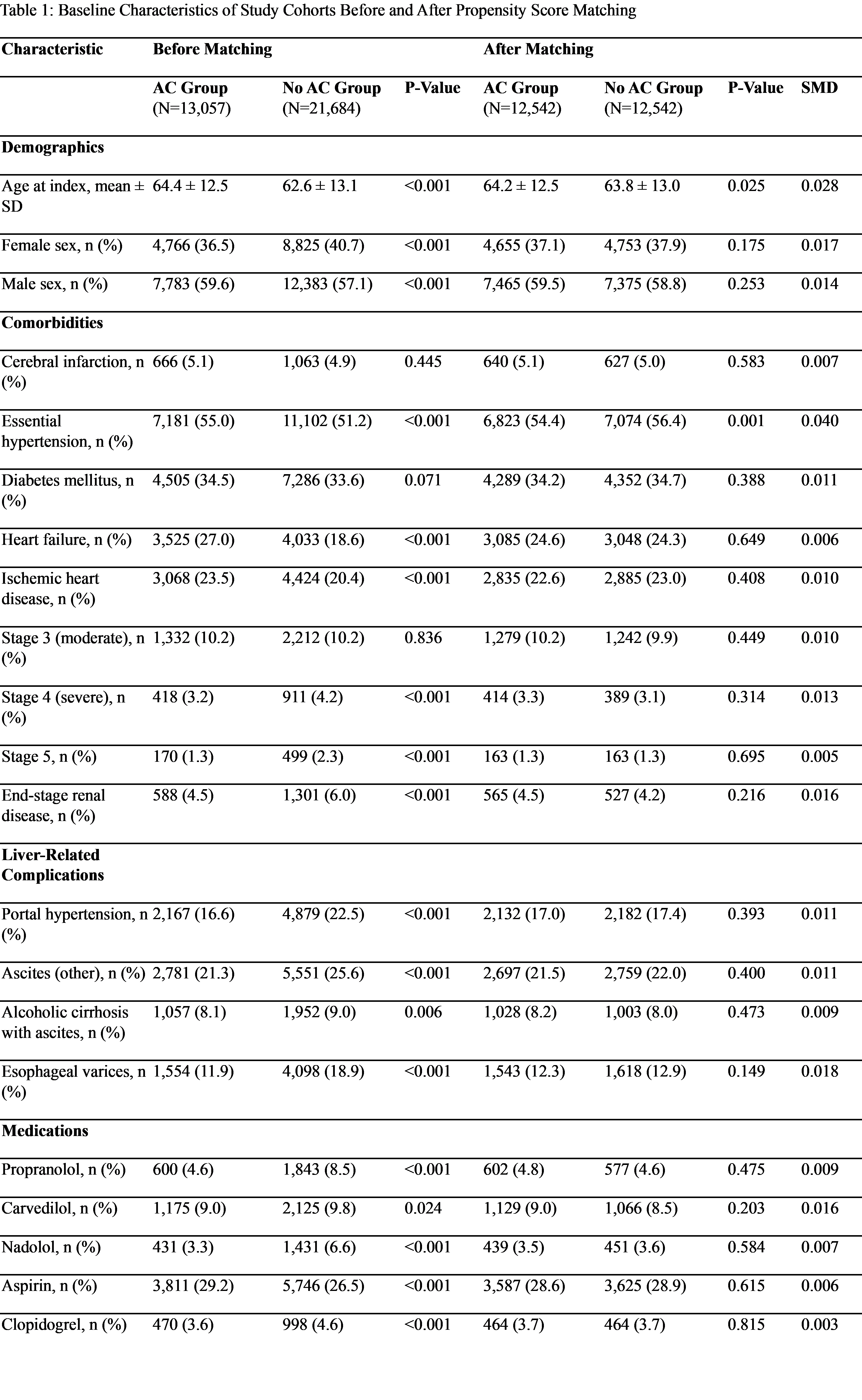
Figure: Baseline demographic, comorbidity, liver disease, and medication characteristics of cirrhotic patients diagnosed with VTE,PVT or AF, comparing those who received anticoagulation (AC group) and those who did not (No AC group), before and after 1:1 propensity score matching (N = 12,542 per group). Variables include age, sex, cardiovascular and renal comorbidities, liver-related complications such as ascites and portal hypertension, and medication use including beta-blockers and antiplatelets. Standardized mean differences (SMD) are shown to demonstrate balance across groups following matching.
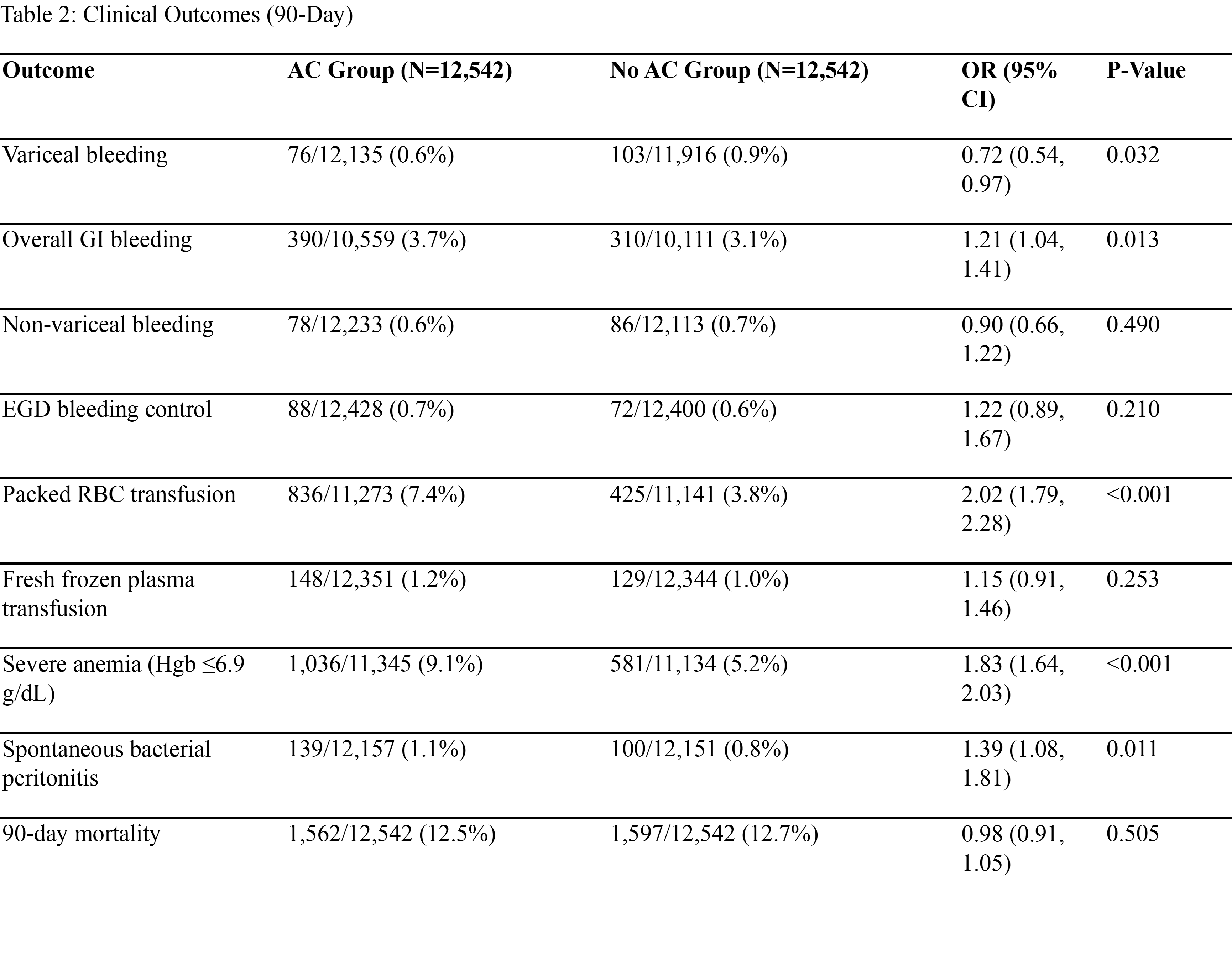
Figure: Ninety-day outcomes in matched cirrhotic patients with VTE,PVT or AF comparing those who received anticoagulation (AC) versus those who did not. Anticoagulation was associated with lower variceal bleeding but higher rates of GI bleeding, transfusion needs, severe anemia, and SBP. No difference in 90-day mortality was observed. Odds ratios (OR) and 95% confidence intervals (CI) are reported.
Disclosures:
Abdulrahman Ibn Awadh indicated no relevant financial relationships.
Randa Albloushy indicated no relevant financial relationships.
Jaime Perez indicated no relevant financial relationships.
Apoorva Chandar indicated no relevant financial relationships.
Resham Ramkissoon indicated no relevant financial relationships.
Abdulrahman Ibn Awadh, MD1, Randa Albloushy, MD1, Jaime A. Perez, PhD1, Apoorva K. Chandar, MBBS, MPH2, Resham Ramkissoon, MD3. P1536 - Risk-Benefit Analysis of Therapeutic Anticoagulation in Liver Cirrhosis: A Large-Scale Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 3university Hospitals Cleveland Medical Center, Case Western Reserve, Cleveland, OH
Introduction: Therapeutic anticoagulation (AC) in patients with cirrhosis presents a challenging clinical dilemma. While variceal hemorrhage contributes significantly to morbidity and mortality, concurrent thrombotic conditions may necessitate anticoagulation, raising significant safety concerns. This study evaluates anticoagulation outcomes in cirrhotic patients with venous thromboembolism (VTE), portal vein thrombosis (PVT), or atrial fibrillation/flutter (AF) using a large national dataset.
Methods: We accessed data through a large-scale, de-identified health research network encompassing 102 healthcare organizations across the United States, representing over 150 million patients (TriNetX, Cambridge, MA). We analyzed AC safety in patients with cirrhosis and VTE, PVT, or AF. Patients were stratified into two groups: [1] those receiving AC within one month of VTE, PVT, or AF diagnosis and [2] those not receiving AC. Specific ICD-10 codes defined cirrhosis, VTE, PVT, and AF, requiring at least two documented cirrhosis diagnoses. Patients with hepatocellular carcinoma and bleeding disorders were excluded. Propensity score matching balanced patient cohorts based on demographics, comorbidities, and medications. Outcomes were assessed at 90 days.
Results: After matching, both groups were well-balanced with average age of 64 years, predominantly male (59%), and similar comorbidity profiles including hypertension (54–56%), diabetes (34%), and heart failure (24%). At 90 days, the AC group demonstrated lower variceal hemorrhage incidence (0.6% vs 0.9%, p=0.032) but higher overall gastrointestinal bleeding (3.7% vs 3.1%, p=0.013). Significantly more blood transfusions were required in the AC group (7.4% vs 3.8%, p< 0.001), with higher rates of severe anemia (9.1% vs 5.2%, p< 0.001) and spontaneous bacterial peritonitis (1.1% vs 0.8%, p=0.011). No significant difference in 90-day mortality was observed (12.5% vs 12.7%, p=0.505). Among AC patients, INR ≥2.0 was associated with significantly higher 90-day mortality versus INR < 2.0 (21.6% vs 16.8%, p=0.040).
Discussion: AC in cirrhotic patients requires careful risk-benefit assessment. While AC patients experienced reduced variceal bleeding, they faced increased transfusion requirements, severe anemia, and infectious complications. Most concerning, INR ≥2.0 was associated with significantly higher mortality, emphasizing the need for individualized decision-making and enhanced monitoring strategies.
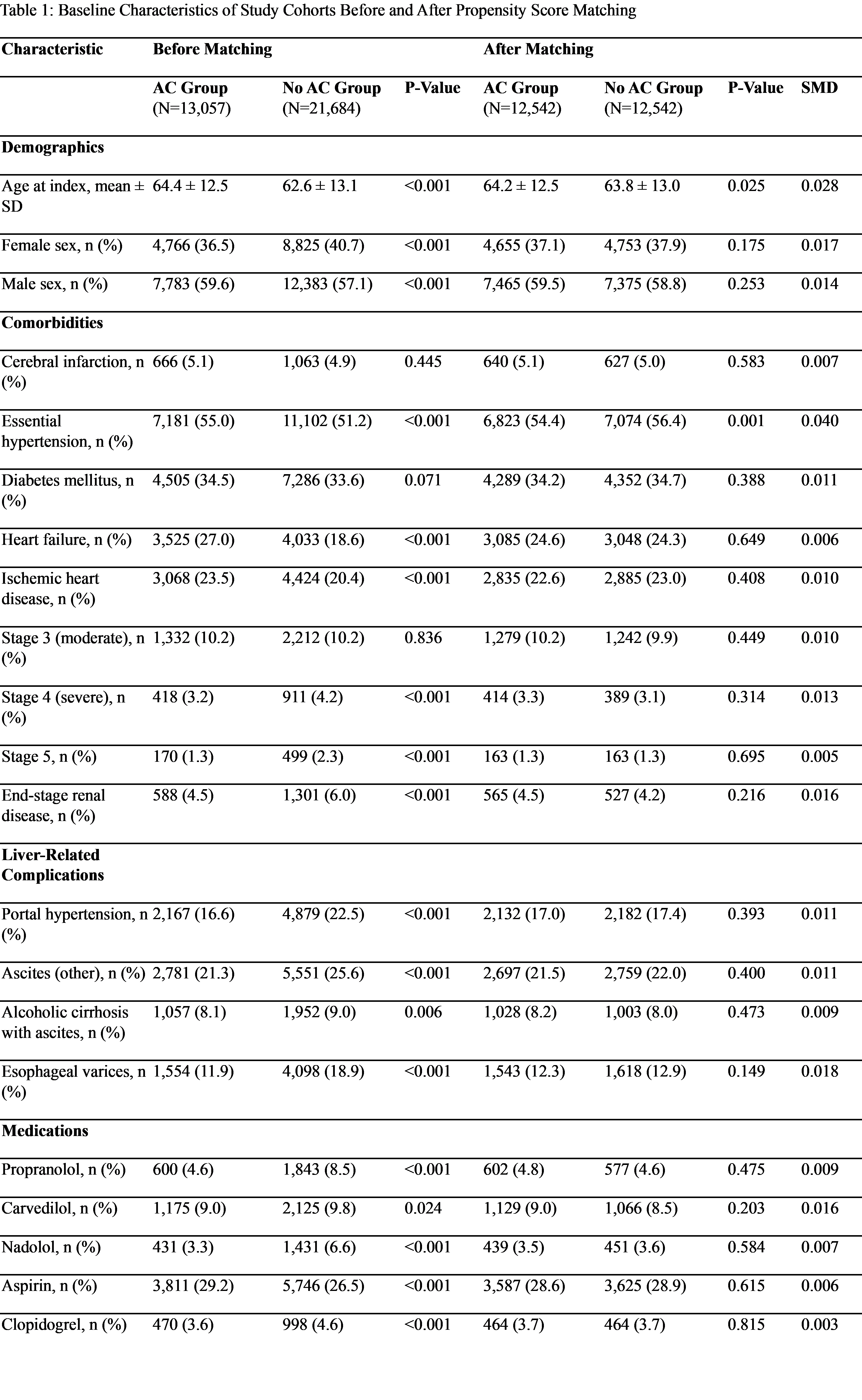
Figure: Baseline demographic, comorbidity, liver disease, and medication characteristics of cirrhotic patients diagnosed with VTE,PVT or AF, comparing those who received anticoagulation (AC group) and those who did not (No AC group), before and after 1:1 propensity score matching (N = 12,542 per group). Variables include age, sex, cardiovascular and renal comorbidities, liver-related complications such as ascites and portal hypertension, and medication use including beta-blockers and antiplatelets. Standardized mean differences (SMD) are shown to demonstrate balance across groups following matching.
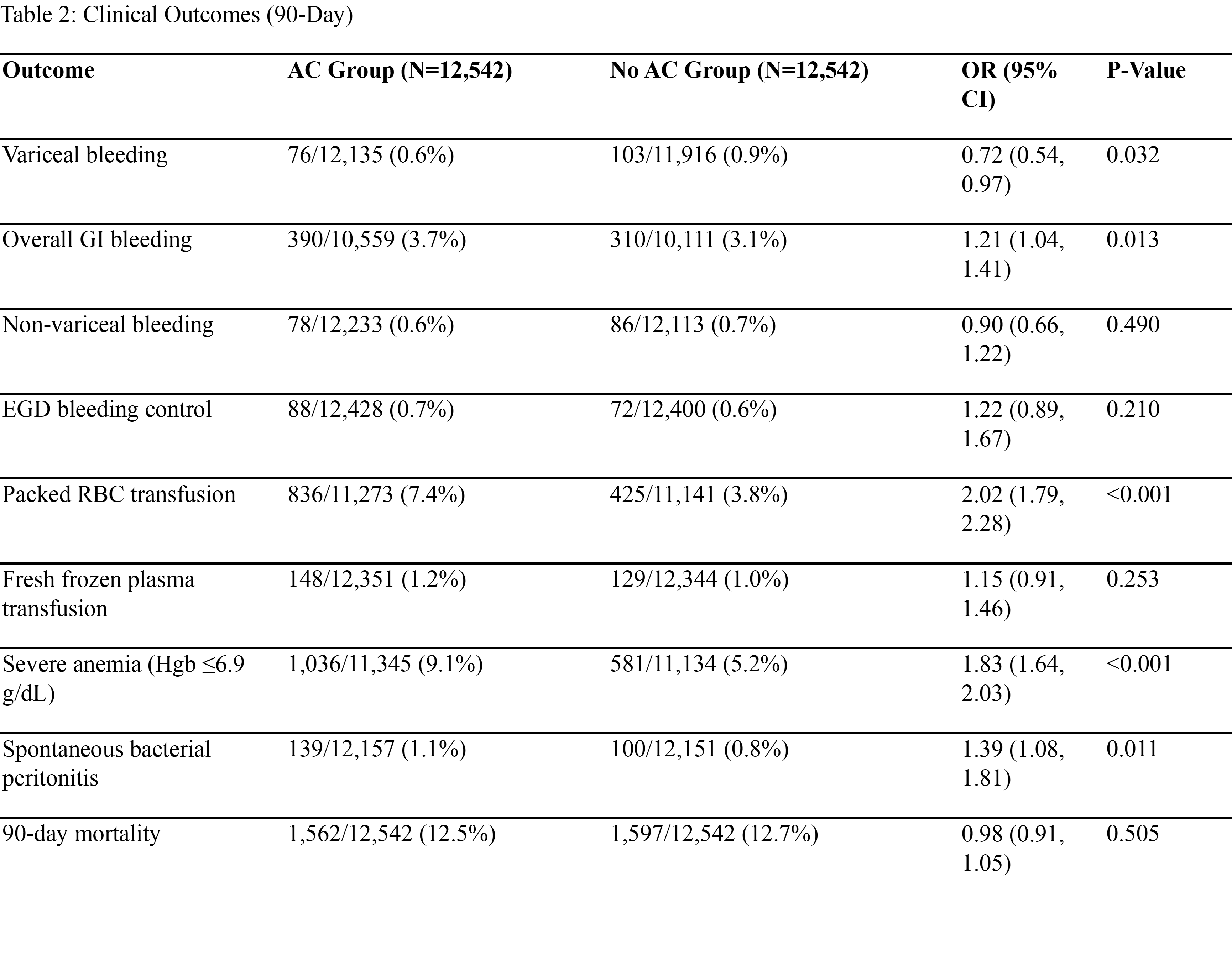
Figure: Ninety-day outcomes in matched cirrhotic patients with VTE,PVT or AF comparing those who received anticoagulation (AC) versus those who did not. Anticoagulation was associated with lower variceal bleeding but higher rates of GI bleeding, transfusion needs, severe anemia, and SBP. No difference in 90-day mortality was observed. Odds ratios (OR) and 95% confidence intervals (CI) are reported.
Disclosures:
Abdulrahman Ibn Awadh indicated no relevant financial relationships.
Randa Albloushy indicated no relevant financial relationships.
Jaime Perez indicated no relevant financial relationships.
Apoorva Chandar indicated no relevant financial relationships.
Resham Ramkissoon indicated no relevant financial relationships.
Abdulrahman Ibn Awadh, MD1, Randa Albloushy, MD1, Jaime A. Perez, PhD1, Apoorva K. Chandar, MBBS, MPH2, Resham Ramkissoon, MD3. P1536 - Risk-Benefit Analysis of Therapeutic Anticoagulation in Liver Cirrhosis: A Large-Scale Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
