Sunday Poster Session
Category: Liver
P1535 - Metabolic Dysfunction-Associated Steatotic Liver Disease and Colorectal Adenomatous Polyp Risk: A Puerto Rican Cohort Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Natalia Rodriguez-Martino, MD (she/her/hers)
University of Puerto Rico, Medical Sciences Campus
San Juan, PR
Presenting Author(s)
Natalia Rodriguez-Martino, MD1, Barbara Rosado-Carrion, MD2, Gladymar Gonzalez-Marrero, MD3, Nicole Fontanet-Gomez, MD4
1University of Puerto Rico, Medical Sciences Campus, San Juan, Puerto Rico; 2Ponce Health Sciences University, School of Medicine, Ponce, Puerto Rico; 3Ponce Health Sciences University, Vega Baja, Puerto Rico; 4Ponce Health Sciences University, Ponce, Puerto Rico
Introduction: This study investigates the association between Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) and the development of colorectal adenomatous polyps and cancer, conditions increasingly linked to risk factors, such as obesity, physical inactivity, and unhealthy diets. A recent meta-analysis found a pooled prevalence of 41% for MASLD in U.S. Hispanic adults, highlighting MASLD as a significant health concern. Given the link between MASLD and metabolic syndrome, our objective is to explore this association in a Puerto Rican cohort.
Methods: This retrospective study evaluated 1,405 records of MASLD patients who underwent colonoscopy. Inclusion criteria included evidence of MASLD via Liver Elastography with Controlled Attenuation Parameter (CAP) score. Patients were categorized based on liver stiffness measures and CAP score for measures of fat accumulation. Variables such as age, gender, BMI, comorbidities, and laboratory findings were considered. Exclusion criteria were implemented to minimize confounding factors known to increase MASLD risk or related to medications that can induce MASLD; these included IBD, autoimmune disorders, immunosuppression, heavy alcohol use and other liver diseases.
Results: Preliminary analysis of 290 records meeting inclusion criteria revealed hypertension in 68.3%, dyslipidemia in 62.1%, diabetes in 44.5%, and obesity in 43.4% as the main comorbidities. Of these 290 records, 44.1% had colonoscopy-confirmed polyps, with 31% being adenomatous, 6.2% hyperplastic, 7.2% other, and no pathology reported for 55.5%. Colorectal polyps were more prevalent in women: 62.7% compared to 37.3% in men, although this difference did not reach statistical significance (p=0.091). Among patients with polyps, fibrosis stages were: F0-F1 in 35.3%, F1 in 37.3% , F2 in 13.7% and F3 in 13.7%. The distribution of CAP scores was: S3 in 23.5% ,S2 in 21.6% ,S1 in 25.5% and S0 in 29.4%.
Discussion: Preliminary results indicate a significant proportion of patients had colonoscopy-confirmed polyps in this MASLD cohort. While no association with hepatocyte steatosis or fibrosis was observed, and the trend toward greater polyp prevalence in women was not statistically significant, further studies are needed to determine whether MASLD truly increases the risk of colorectal polyps, specifically adenomatous, when compared to individuals without MASLD and to investigate potential gender related disparities.
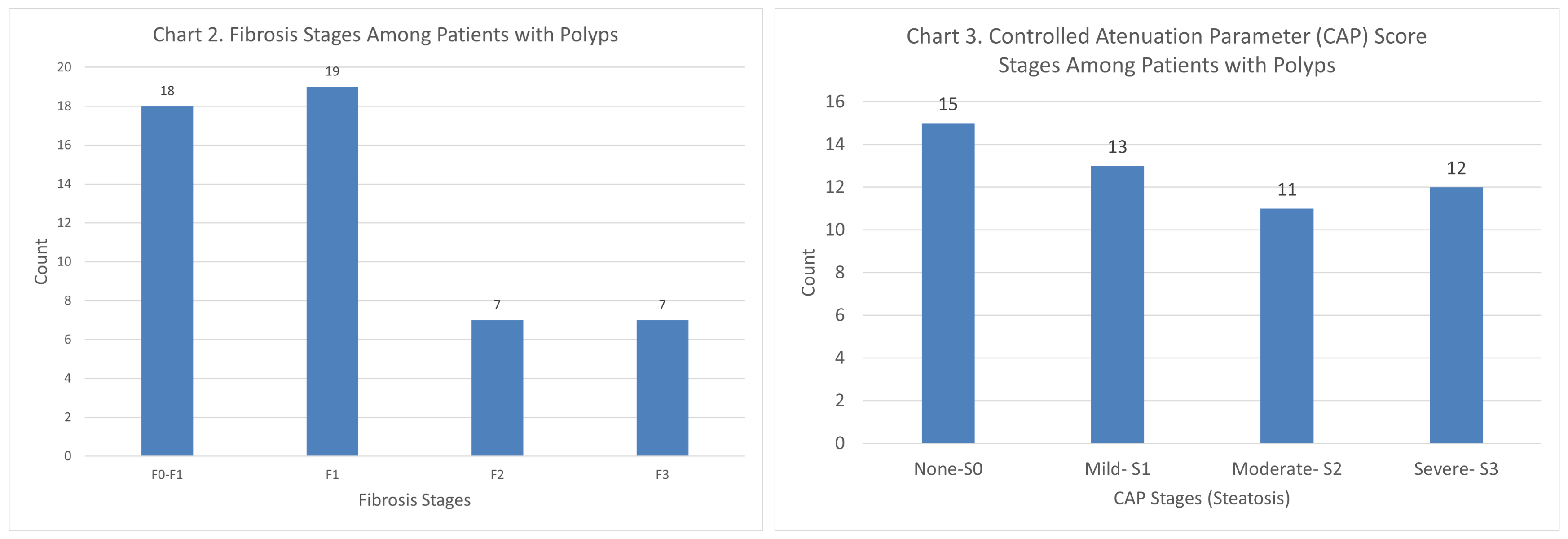
Figure: Chart 1: Post-Colonoscopy Polyp Findings by Gender.
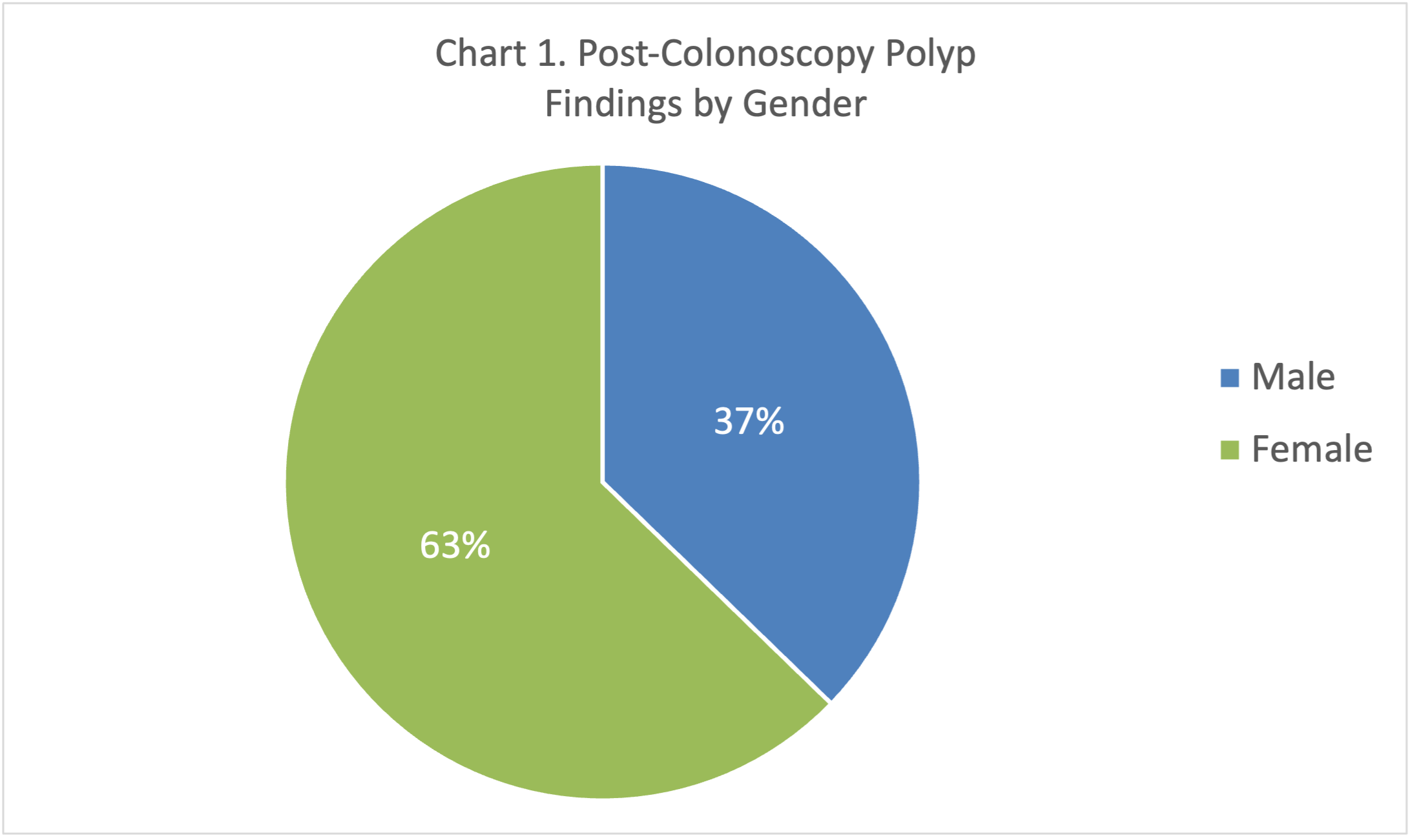
Figure: Chart 2: Fibrosis Stages Among Patients with Polyps; Chart 3: Controlled Attenuation Parameter (CAP) Score Stages Among Patients with Polyps.
Disclosures:
Natalia Rodriguez-Martino indicated no relevant financial relationships.
Barbara Rosado-Carrion indicated no relevant financial relationships.
Gladymar Gonzalez-Marrero indicated no relevant financial relationships.
Nicole Fontanet-Gomez indicated no relevant financial relationships.
Natalia Rodriguez-Martino, MD1, Barbara Rosado-Carrion, MD2, Gladymar Gonzalez-Marrero, MD3, Nicole Fontanet-Gomez, MD4. P1535 - Metabolic Dysfunction-Associated Steatotic Liver Disease and Colorectal Adenomatous Polyp Risk: A Puerto Rican Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Puerto Rico, Medical Sciences Campus, San Juan, Puerto Rico; 2Ponce Health Sciences University, School of Medicine, Ponce, Puerto Rico; 3Ponce Health Sciences University, Vega Baja, Puerto Rico; 4Ponce Health Sciences University, Ponce, Puerto Rico
Introduction: This study investigates the association between Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) and the development of colorectal adenomatous polyps and cancer, conditions increasingly linked to risk factors, such as obesity, physical inactivity, and unhealthy diets. A recent meta-analysis found a pooled prevalence of 41% for MASLD in U.S. Hispanic adults, highlighting MASLD as a significant health concern. Given the link between MASLD and metabolic syndrome, our objective is to explore this association in a Puerto Rican cohort.
Methods: This retrospective study evaluated 1,405 records of MASLD patients who underwent colonoscopy. Inclusion criteria included evidence of MASLD via Liver Elastography with Controlled Attenuation Parameter (CAP) score. Patients were categorized based on liver stiffness measures and CAP score for measures of fat accumulation. Variables such as age, gender, BMI, comorbidities, and laboratory findings were considered. Exclusion criteria were implemented to minimize confounding factors known to increase MASLD risk or related to medications that can induce MASLD; these included IBD, autoimmune disorders, immunosuppression, heavy alcohol use and other liver diseases.
Results: Preliminary analysis of 290 records meeting inclusion criteria revealed hypertension in 68.3%, dyslipidemia in 62.1%, diabetes in 44.5%, and obesity in 43.4% as the main comorbidities. Of these 290 records, 44.1% had colonoscopy-confirmed polyps, with 31% being adenomatous, 6.2% hyperplastic, 7.2% other, and no pathology reported for 55.5%. Colorectal polyps were more prevalent in women: 62.7% compared to 37.3% in men, although this difference did not reach statistical significance (p=0.091). Among patients with polyps, fibrosis stages were: F0-F1 in 35.3%, F1 in 37.3% , F2 in 13.7% and F3 in 13.7%. The distribution of CAP scores was: S3 in 23.5% ,S2 in 21.6% ,S1 in 25.5% and S0 in 29.4%.
Discussion: Preliminary results indicate a significant proportion of patients had colonoscopy-confirmed polyps in this MASLD cohort. While no association with hepatocyte steatosis or fibrosis was observed, and the trend toward greater polyp prevalence in women was not statistically significant, further studies are needed to determine whether MASLD truly increases the risk of colorectal polyps, specifically adenomatous, when compared to individuals without MASLD and to investigate potential gender related disparities.
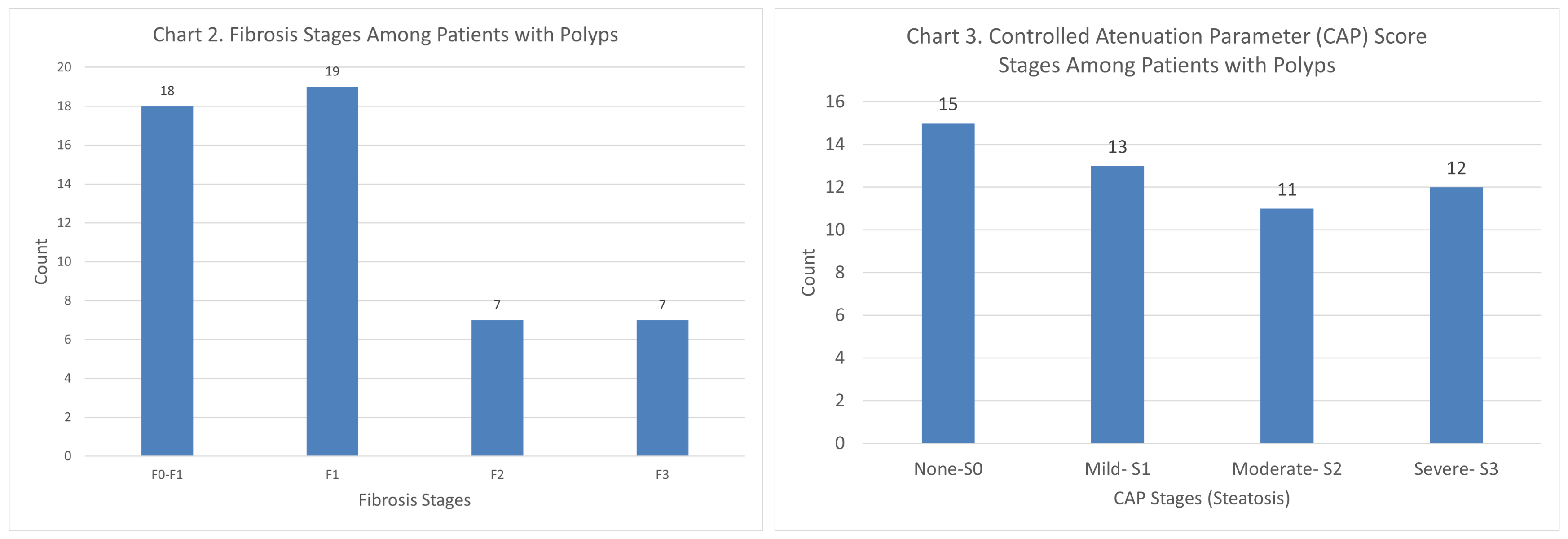
Figure: Chart 1: Post-Colonoscopy Polyp Findings by Gender.
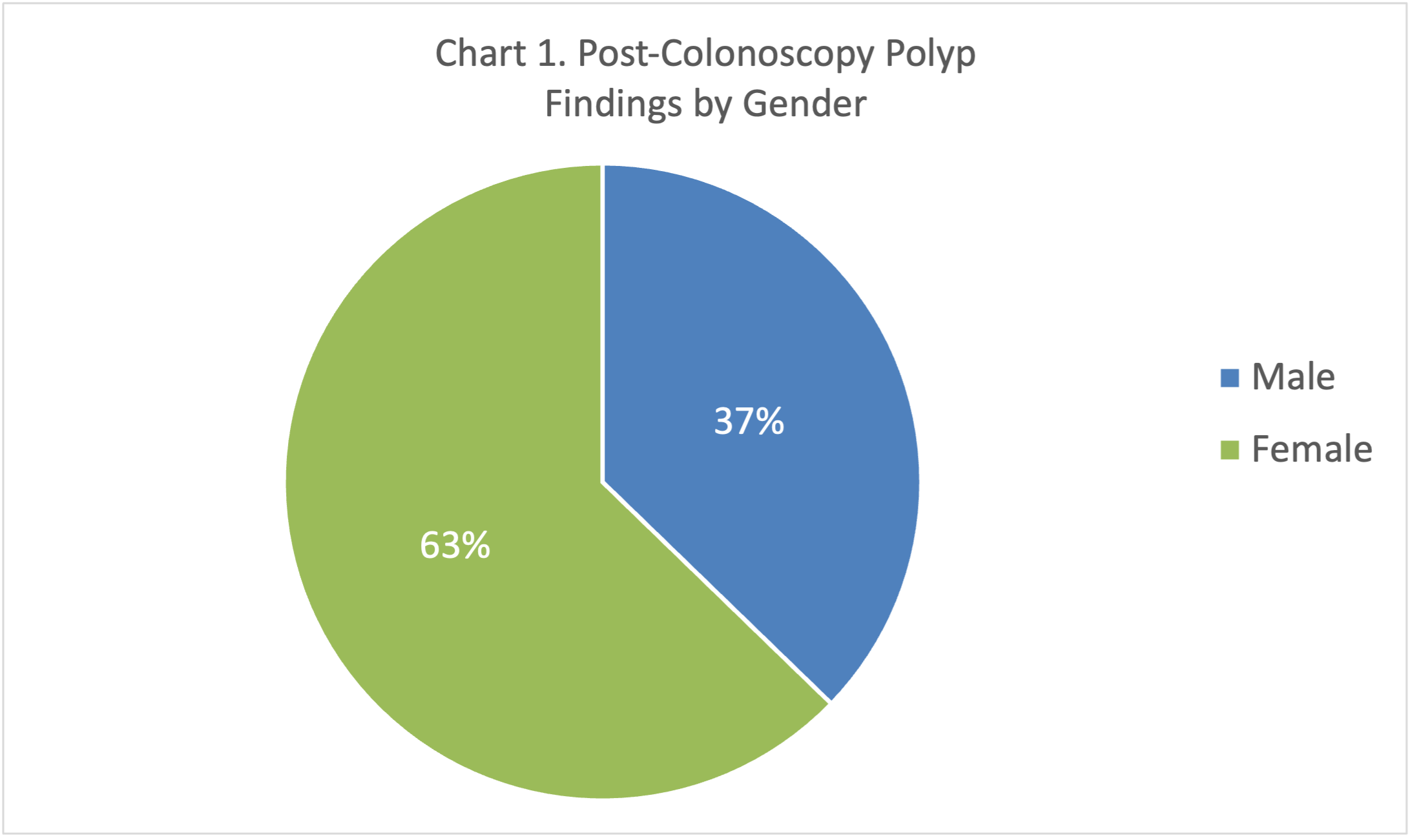
Figure: Chart 2: Fibrosis Stages Among Patients with Polyps; Chart 3: Controlled Attenuation Parameter (CAP) Score Stages Among Patients with Polyps.
Disclosures:
Natalia Rodriguez-Martino indicated no relevant financial relationships.
Barbara Rosado-Carrion indicated no relevant financial relationships.
Gladymar Gonzalez-Marrero indicated no relevant financial relationships.
Nicole Fontanet-Gomez indicated no relevant financial relationships.
Natalia Rodriguez-Martino, MD1, Barbara Rosado-Carrion, MD2, Gladymar Gonzalez-Marrero, MD3, Nicole Fontanet-Gomez, MD4. P1535 - Metabolic Dysfunction-Associated Steatotic Liver Disease and Colorectal Adenomatous Polyp Risk: A Puerto Rican Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
