Sunday Poster Session
Category: Liver
P1534 - An Updated Systematic Review and Meta-Analysis on the Effects of Intermittent Fasting on NAFLD Progression
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Urmimala Chaudhuri, DO
Wright State University
Centerville, OH
Presenting Author(s)
Urmimala Chaudhuri, DO1, Sangeeta Agrawal, MD2
1Wright State University, Centerville, OH; 2Wright State University Boonshoft School of Medicine, Dayton, OH
Introduction: Non-alcoholic fatty liver disease (NAFLD), the hepatic manifestation of metabolic syndrome, is characterized by excess intrahepatic fat accumulation. With no approved pharmacologic therapies, lifestyle interventions remain the cornerstone of treatment. Intermittent fasting (IF) is a dietary strategy that cycles between periods of eating and fasting, which has gained interest for its potential to reduce hepatic fat and improve metabolic parameters. This study aimed to conduct an updated systematic review and meta-analysis assessing the effects of IF on liver-related biomarkers and fibrosis in adults with NAFLD.
Methods: A systematic search was conducted in PubMed, ClinicalTrials.gov, and DOAJ to identify studies assessing the effects of IF (time-restricted feeding (TRF), alternate-day fasting (ADF), and 5:2 IF) in adults with NAFLD. Eligible studies reported the pre- and post-intervention values for liver enzymes, liver stiffness, or BMI. Meta-analysis was performed using a random-effects model in JASP (v0.19.3) with heterogeneity assessed using the I-squared and Cochran’s Q statistics.
Results: Eight studies (seven randomized controlled trials and one prospective intervention) comprising 412 adults met inclusion criteria. Compared to control groups, IF was associated with a significant reduction in BMI (-0.73, p=0.014) while reductions in ALT (-0.45) and liver stiffness (-0.46) were observed but not statistically significant. Within-group analysis of IF participants showed significant post-intervention improvements: BMI decreased by 1.61 points, liver stiffness by 1.42 kPa, ALT by 7.45 U/L, and AST by 5.51 U/L.
Discussion: Our findings suggest that IF yields clinically meaningful improvements in liver health among adults with NAFLD. While between-group differences were not consistently significant, IF consistently trended toward benefit. This analysis builds on prior literature by including recent trials and evaluating both enzymatic and fibrotic endpoints. The observed improvements may be driven by reductions in hepatic insulin resistance and de novo lipogenesis, which have been proposed as key mechanisms underlying IF’s metabolic benefits. As NAFLD prevalence continues to rise globally, IF represents an accessible and potentially impactful intervention. Future large-scale trials, particularly across diverse populations, are essential to continue validating these findings.
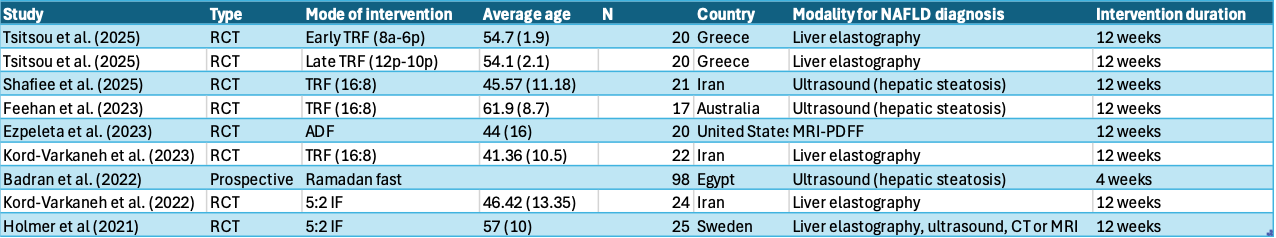
Figure: Table 1. Summary of Studies Included in the Systematic Review and Meta-Analysis. This table outlines characteristics of the studies included in the analysis. Interventions included time-restricted feeding, alternate-day fasting, 5:2 intermittent fasting, and Ramadan fasting. NAFLD was diagnosed using various modalities. Most interventions lasted 12 weeks.
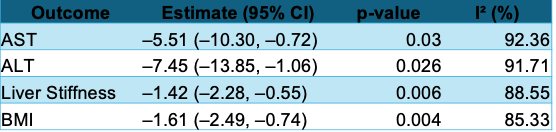
Figure: Table 2. Within-Group Changes in Liver-Related Biomarkers and BMI. Pooled analysis showed significant reductions in AST, ALT, liver stiffness, and BMI among participants undergoing intermittent fasting.
Disclosures:
Urmimala Chaudhuri indicated no relevant financial relationships.
Sangeeta Agrawal indicated no relevant financial relationships.
Urmimala Chaudhuri, DO1, Sangeeta Agrawal, MD2. P1534 - An Updated Systematic Review and Meta-Analysis on the Effects of Intermittent Fasting on NAFLD Progression, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Wright State University, Centerville, OH; 2Wright State University Boonshoft School of Medicine, Dayton, OH
Introduction: Non-alcoholic fatty liver disease (NAFLD), the hepatic manifestation of metabolic syndrome, is characterized by excess intrahepatic fat accumulation. With no approved pharmacologic therapies, lifestyle interventions remain the cornerstone of treatment. Intermittent fasting (IF) is a dietary strategy that cycles between periods of eating and fasting, which has gained interest for its potential to reduce hepatic fat and improve metabolic parameters. This study aimed to conduct an updated systematic review and meta-analysis assessing the effects of IF on liver-related biomarkers and fibrosis in adults with NAFLD.
Methods: A systematic search was conducted in PubMed, ClinicalTrials.gov, and DOAJ to identify studies assessing the effects of IF (time-restricted feeding (TRF), alternate-day fasting (ADF), and 5:2 IF) in adults with NAFLD. Eligible studies reported the pre- and post-intervention values for liver enzymes, liver stiffness, or BMI. Meta-analysis was performed using a random-effects model in JASP (v0.19.3) with heterogeneity assessed using the I-squared and Cochran’s Q statistics.
Results: Eight studies (seven randomized controlled trials and one prospective intervention) comprising 412 adults met inclusion criteria. Compared to control groups, IF was associated with a significant reduction in BMI (-0.73, p=0.014) while reductions in ALT (-0.45) and liver stiffness (-0.46) were observed but not statistically significant. Within-group analysis of IF participants showed significant post-intervention improvements: BMI decreased by 1.61 points, liver stiffness by 1.42 kPa, ALT by 7.45 U/L, and AST by 5.51 U/L.
Discussion: Our findings suggest that IF yields clinically meaningful improvements in liver health among adults with NAFLD. While between-group differences were not consistently significant, IF consistently trended toward benefit. This analysis builds on prior literature by including recent trials and evaluating both enzymatic and fibrotic endpoints. The observed improvements may be driven by reductions in hepatic insulin resistance and de novo lipogenesis, which have been proposed as key mechanisms underlying IF’s metabolic benefits. As NAFLD prevalence continues to rise globally, IF represents an accessible and potentially impactful intervention. Future large-scale trials, particularly across diverse populations, are essential to continue validating these findings.
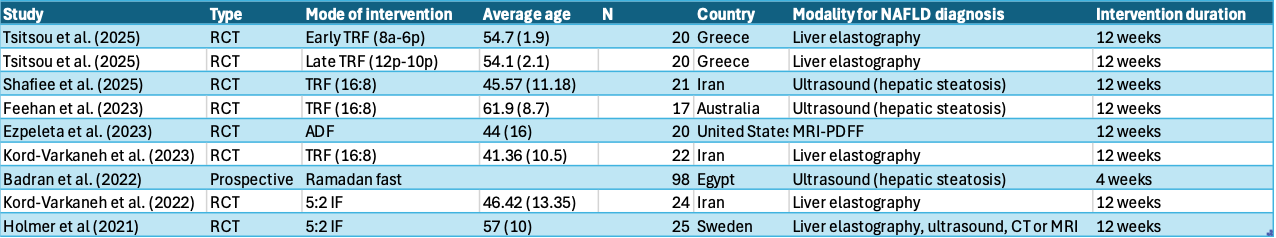
Figure: Table 1. Summary of Studies Included in the Systematic Review and Meta-Analysis. This table outlines characteristics of the studies included in the analysis. Interventions included time-restricted feeding, alternate-day fasting, 5:2 intermittent fasting, and Ramadan fasting. NAFLD was diagnosed using various modalities. Most interventions lasted 12 weeks.
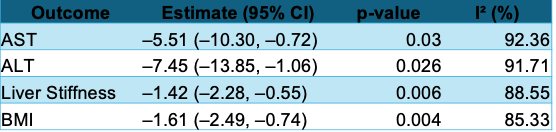
Figure: Table 2. Within-Group Changes in Liver-Related Biomarkers and BMI. Pooled analysis showed significant reductions in AST, ALT, liver stiffness, and BMI among participants undergoing intermittent fasting.
Disclosures:
Urmimala Chaudhuri indicated no relevant financial relationships.
Sangeeta Agrawal indicated no relevant financial relationships.
Urmimala Chaudhuri, DO1, Sangeeta Agrawal, MD2. P1534 - An Updated Systematic Review and Meta-Analysis on the Effects of Intermittent Fasting on NAFLD Progression, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

