Sunday Poster Session
Category: Liver
P1532 - Missed Opportunities: Gaps and Disparities in Pharmacologic Treatment for Alcohol Use Disorder
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
WonKyung Cho, MD, MPH
Long Island Jewish Forest Hills Hospital - Northwell Health
Queens, NY
Presenting Author(s)
WonKyung Cho, MD, MPH1, Matthew Leiman, DO2, Sumeeta Sajnani, MD2
1Long Island Jewish Forest Hills Hospital - Northwell Health, Queens, NY; 2Long Island Jewish Forest Hills Hospital - Northwell Health, Forest Hills, NY
Introduction: Alcohol use disorder (AUD) affects nearly 30 million individuals in the U.S., contributing to significant medical and societal burdens. Although multiple pharmacologic treatments are available—FDA-approved (acamprosate, disulfiram, naltrexone) and off-label (gabapentin, topiramate)—fewer than 2% of patients receive medication. This study examined prescribing patterns for AUD pharmacotherapy and identified factors associated with medication receipt within a large hospital system.
Methods: A retrospective analysis was conducted using the Northwestern ICU (NWICU) database, identifying adults with ICD-10 codes for alcohol-related disorders who received care at Northwestern Memorial HealthCare from 2020–2022. Receipt of FDA-approved or off-label alcohol cessation medications was evaluated. To reduce confounding, SSRI prescriptions in patients with documented mental health diagnoses and gabapentin prescriptions in those with chronic pain, neuropathy, or diabetes were excluded from the analysis. Logistic regression models adjusted for age, sex, and race was utilized to identify factors associated with treatment.
Results: Among 1,331 patients (mean age 52; 28.0% female), only 3.7% received FDA-approved pharmacotherapy for AUD. Off-label use was more frequent, with 19.6% receiving gabapentin and 6.7% SSRIs. Factors associated with increased likelihood of receiving FDA-approved treatment included younger age (OR 1.03, 95% CI 1.007–1.059), presence of mental health comorbidities (OR 2.46, 95% CI 1.37–4.42), and frequent hospitalizations (OR 4.09, 95% CI 2.04–8.19). A secondary analysis including off-label prescriptions demonstrated similar trends. Notably, Spanish-speaking patients were significantly less likely to receive any pharmacologic treatment compared to English speakers (OR 3.31, 95% CI 1.06–10.34). There were no differences by race or sex in the receipt of FDA-approved medications. Additionally, patients with liver disease were not more likely to receive treatment despite heightened clinical risk.
Discussion: Pharmacologic treatment for AUD remains underwhelming, and notable disparities in care persist, particularly among Spanish-speaking and older patients. These findings highlight a need to improve equitable access to evidence-based AUD treatments. Hospitalization presents a key opportunity to engage patients and initiate therapy. Addressing language barriers and integrating culturally appropriate interventions may help close persistent treatment gaps.
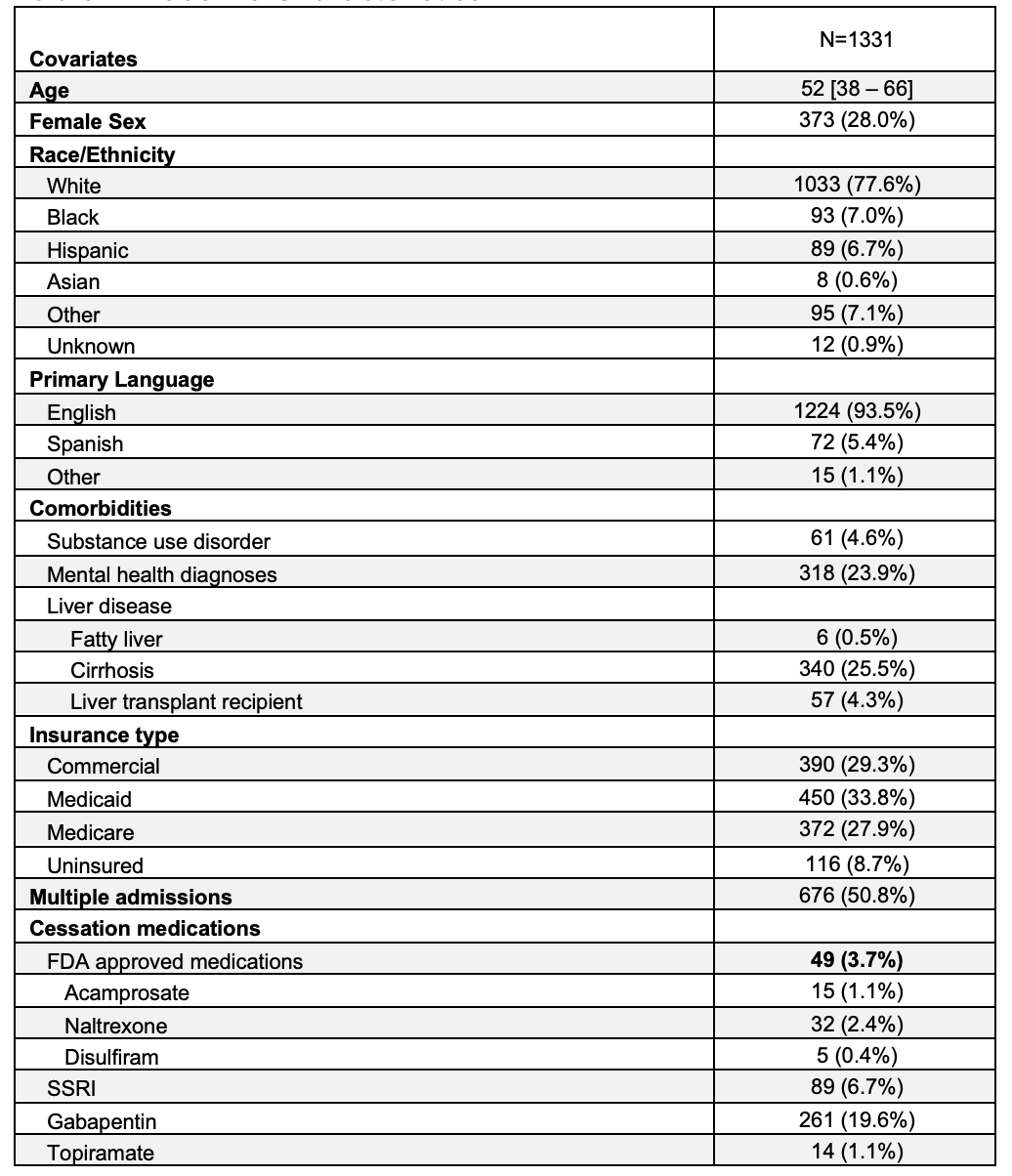
Figure: Baseline Characteristics
Disclosures:
WonKyung Cho indicated no relevant financial relationships.
Matthew Leiman indicated no relevant financial relationships.
Sumeeta Sajnani indicated no relevant financial relationships.
WonKyung Cho, MD, MPH1, Matthew Leiman, DO2, Sumeeta Sajnani, MD2. P1532 - Missed Opportunities: Gaps and Disparities in Pharmacologic Treatment for Alcohol Use Disorder, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Long Island Jewish Forest Hills Hospital - Northwell Health, Queens, NY; 2Long Island Jewish Forest Hills Hospital - Northwell Health, Forest Hills, NY
Introduction: Alcohol use disorder (AUD) affects nearly 30 million individuals in the U.S., contributing to significant medical and societal burdens. Although multiple pharmacologic treatments are available—FDA-approved (acamprosate, disulfiram, naltrexone) and off-label (gabapentin, topiramate)—fewer than 2% of patients receive medication. This study examined prescribing patterns for AUD pharmacotherapy and identified factors associated with medication receipt within a large hospital system.
Methods: A retrospective analysis was conducted using the Northwestern ICU (NWICU) database, identifying adults with ICD-10 codes for alcohol-related disorders who received care at Northwestern Memorial HealthCare from 2020–2022. Receipt of FDA-approved or off-label alcohol cessation medications was evaluated. To reduce confounding, SSRI prescriptions in patients with documented mental health diagnoses and gabapentin prescriptions in those with chronic pain, neuropathy, or diabetes were excluded from the analysis. Logistic regression models adjusted for age, sex, and race was utilized to identify factors associated with treatment.
Results: Among 1,331 patients (mean age 52; 28.0% female), only 3.7% received FDA-approved pharmacotherapy for AUD. Off-label use was more frequent, with 19.6% receiving gabapentin and 6.7% SSRIs. Factors associated with increased likelihood of receiving FDA-approved treatment included younger age (OR 1.03, 95% CI 1.007–1.059), presence of mental health comorbidities (OR 2.46, 95% CI 1.37–4.42), and frequent hospitalizations (OR 4.09, 95% CI 2.04–8.19). A secondary analysis including off-label prescriptions demonstrated similar trends. Notably, Spanish-speaking patients were significantly less likely to receive any pharmacologic treatment compared to English speakers (OR 3.31, 95% CI 1.06–10.34). There were no differences by race or sex in the receipt of FDA-approved medications. Additionally, patients with liver disease were not more likely to receive treatment despite heightened clinical risk.
Discussion: Pharmacologic treatment for AUD remains underwhelming, and notable disparities in care persist, particularly among Spanish-speaking and older patients. These findings highlight a need to improve equitable access to evidence-based AUD treatments. Hospitalization presents a key opportunity to engage patients and initiate therapy. Addressing language barriers and integrating culturally appropriate interventions may help close persistent treatment gaps.
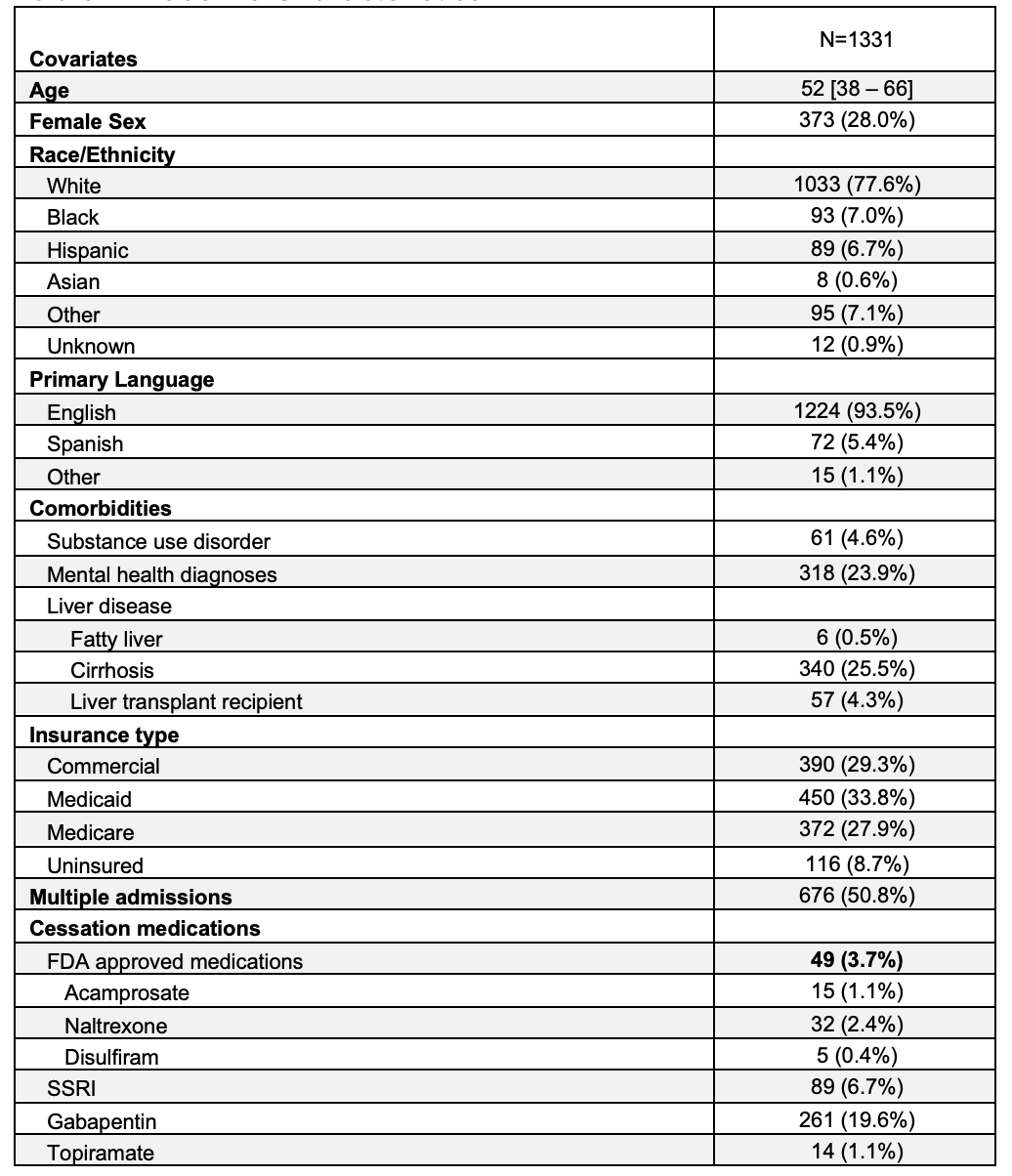
Figure: Baseline Characteristics
Disclosures:
WonKyung Cho indicated no relevant financial relationships.
Matthew Leiman indicated no relevant financial relationships.
Sumeeta Sajnani indicated no relevant financial relationships.
WonKyung Cho, MD, MPH1, Matthew Leiman, DO2, Sumeeta Sajnani, MD2. P1532 - Missed Opportunities: Gaps and Disparities in Pharmacologic Treatment for Alcohol Use Disorder, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.


