Sunday Poster Session
Category: Liver
P1530 - Assessing Gastrointestinal Bleeding Risk in Cirrhosis: A Multivariable Analysis Using a Nationally Representative Cohort
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- VB
Viknesh Baskar, BA
SUNY Downstate Health Sciences University
Brooklyn, NY
Presenting Author(s)
Viknesh Baskar, BA1, Rebhi Rabah, MD1, Sanjana Baskar, BS2, Sushil K. Ahlawat, MD3
1SUNY Downstate Health Sciences University, Brooklyn, NY; 2Binghamton University, Binghamton, NY; 3SUNY Downstate Medical Center, Brooklyn, NY
Introduction: Gastrointestinal (GI) bleeding is a common and potentially life-threatening complication of cirrhosis. While portal hypertension is a well-known driver, the role of comorbid conditions and social determinants in bleeding risk is less clearly defined. Using the diverse and nationally representative All of Us Research Program, we sought to identify clinical and demographic predictors of GI bleeding among patients with cirrhosis.
Methods: A cross-sectional analysis was performed using the All of Us Registered Tier Dataset version 7. Adults with cirrhosis were identified using ICD-10 codes and stratified into two cohorts: those with a diagnosis of GI bleeding following their cirrhosis diagnosis and those without a diagnosis of GI bleeding. A multivariable logistic regression model was constructed to assess associations between clinical and demographic factors and the likelihood of GI bleeding in cirrhosis. Demographic variables included age, sex, race, and income. Clinical factors included smoking, alcohol use, obesity, diabetes, hypertension, hyperlipidemia, and heart disease.
Results: 7,297 participants with cirrhosis were included, of whom 2,386 had a documented GI bleed following cirrhosis diagnosis and 4,911 did not. Patients with GI bleeding were older and more likely to be female. Several comorbidities were independently associated with increased odds of GI bleeding, including hypertension (OR 1.61, 95% CI 1.36–1.90, p < 0.001), heart disease (OR 1.72, 95% CI 1.42–2.10, p < 0.001), hyperlipidemia (OR 1.19, 95% CI 1.04–1.37, p = 0.014), and obesity (OR 1.17, 95% CI 1.03–1.33, p = 0.014). Female sex (OR 1.31, 95% CI 1.17–1.48, p < 0.001) was also associated with greater bleeding risk. Higher income was associated with lower odds of GI bleeding, with those earning over $100,000 having significantly reduced odds (OR 0.71, 95% CI 0.55–0.91, p = 0.007). Smoking, diabetes, and racial groups were not significantly associated.
Discussion: Our study found that common cardiovascular comorbidities including hypertension, heart disease, hyperlipidemia, and obesity were strongly associated with increased odds of GI bleeding. The protective effect of higher income underscores the role of socioeconomic status in shaping clinical outcomes, reflecting differences in access to care, surveillance, and management of chronic disease. Future work is needed to explore whether targeting modifiable comorbidities and addressing social determinants of health can mitigate bleeding risk in cirrhotic populations.
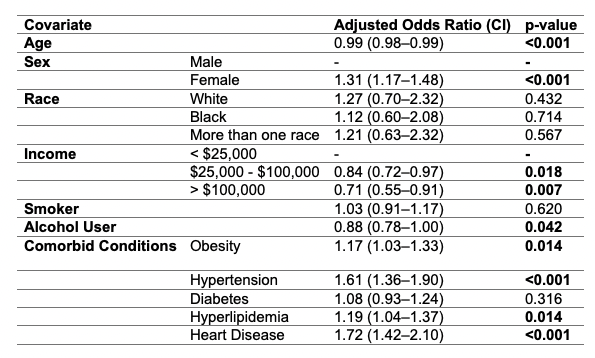
Figure: Table 1. – Multivariable analysis of predictors of gastrointestinal bleeding in cirrhosis
Disclosures:
Viknesh Baskar indicated no relevant financial relationships.
Rebhi Rabah indicated no relevant financial relationships.
Sanjana Baskar indicated no relevant financial relationships.
Sushil Ahlawat indicated no relevant financial relationships.
Viknesh Baskar, BA1, Rebhi Rabah, MD1, Sanjana Baskar, BS2, Sushil K. Ahlawat, MD3. P1530 - Assessing Gastrointestinal Bleeding Risk in Cirrhosis: A Multivariable Analysis Using a Nationally Representative Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SUNY Downstate Health Sciences University, Brooklyn, NY; 2Binghamton University, Binghamton, NY; 3SUNY Downstate Medical Center, Brooklyn, NY
Introduction: Gastrointestinal (GI) bleeding is a common and potentially life-threatening complication of cirrhosis. While portal hypertension is a well-known driver, the role of comorbid conditions and social determinants in bleeding risk is less clearly defined. Using the diverse and nationally representative All of Us Research Program, we sought to identify clinical and demographic predictors of GI bleeding among patients with cirrhosis.
Methods: A cross-sectional analysis was performed using the All of Us Registered Tier Dataset version 7. Adults with cirrhosis were identified using ICD-10 codes and stratified into two cohorts: those with a diagnosis of GI bleeding following their cirrhosis diagnosis and those without a diagnosis of GI bleeding. A multivariable logistic regression model was constructed to assess associations between clinical and demographic factors and the likelihood of GI bleeding in cirrhosis. Demographic variables included age, sex, race, and income. Clinical factors included smoking, alcohol use, obesity, diabetes, hypertension, hyperlipidemia, and heart disease.
Results: 7,297 participants with cirrhosis were included, of whom 2,386 had a documented GI bleed following cirrhosis diagnosis and 4,911 did not. Patients with GI bleeding were older and more likely to be female. Several comorbidities were independently associated with increased odds of GI bleeding, including hypertension (OR 1.61, 95% CI 1.36–1.90, p < 0.001), heart disease (OR 1.72, 95% CI 1.42–2.10, p < 0.001), hyperlipidemia (OR 1.19, 95% CI 1.04–1.37, p = 0.014), and obesity (OR 1.17, 95% CI 1.03–1.33, p = 0.014). Female sex (OR 1.31, 95% CI 1.17–1.48, p < 0.001) was also associated with greater bleeding risk. Higher income was associated with lower odds of GI bleeding, with those earning over $100,000 having significantly reduced odds (OR 0.71, 95% CI 0.55–0.91, p = 0.007). Smoking, diabetes, and racial groups were not significantly associated.
Discussion: Our study found that common cardiovascular comorbidities including hypertension, heart disease, hyperlipidemia, and obesity were strongly associated with increased odds of GI bleeding. The protective effect of higher income underscores the role of socioeconomic status in shaping clinical outcomes, reflecting differences in access to care, surveillance, and management of chronic disease. Future work is needed to explore whether targeting modifiable comorbidities and addressing social determinants of health can mitigate bleeding risk in cirrhotic populations.
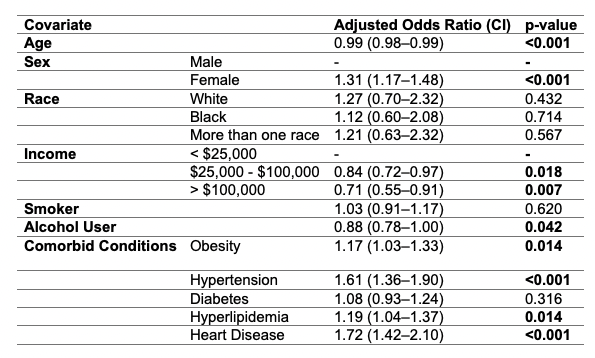
Figure: Table 1. – Multivariable analysis of predictors of gastrointestinal bleeding in cirrhosis
Disclosures:
Viknesh Baskar indicated no relevant financial relationships.
Rebhi Rabah indicated no relevant financial relationships.
Sanjana Baskar indicated no relevant financial relationships.
Sushil Ahlawat indicated no relevant financial relationships.
Viknesh Baskar, BA1, Rebhi Rabah, MD1, Sanjana Baskar, BS2, Sushil K. Ahlawat, MD3. P1530 - Assessing Gastrointestinal Bleeding Risk in Cirrhosis: A Multivariable Analysis Using a Nationally Representative Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
