Sunday Poster Session
Category: Liver
P1526 - Gender Disparities in Liver Transplantation: A Systematic Review and Meta-Analysis of Access, Waitlist Outcomes, and Post-Transplant Survival
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- JA
John K. Appiah, MD
Geisinger Wyoming Valley Medical Center
Wilkes-Barre, PA
Presenting Author(s)
John K. Appiah, MD1, George S. Blewusi, MD2, Ewurabena N. Plange-Kaye, DDS3, Richeal Asante, MD4, Edward A. Danso, MD5, Emmanuel Asiedu, MD6
1Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 2Johns Hopkins Bloomberg School of Public Health, Baltimore, MD; 3Columbia University, Dumont, NJ; 4Geisinger Wyoming Valley Medical Center, Kingston, PA; 5Korle-Bu Teaching Hospital, Accra, Greater Accra, Ghana; 6Mother and Child Hospital, Accra, Central, Ghana
Introduction: Gender disparities in liver transplantation have emerged as a critical equity issue, with growing evidence suggesting systematic disadvantages for women throughout the transplant process. While individual studies have reported gender differences in waitlist mortality, transplant access, and post-transplant outcomes, comprehensive quantitative synthesis of this evidence remains lacking. Understanding the magnitude and consistency of these disparities is essential for informing policy reforms and clinical practice improvements.
Methods: We systematically searched PubMed, Cochrane, and Google Scholar databases (2005–2024) for studies reporting gender-stratified outcomes in adult liver transplant candidates or recipients. This review was registered with PROSPERO (CRD420251039195). We included original peer-reviewed studies reporting adjusted effect estimates for transplant rate, waitlist mortality, or post-transplant outcomes. Pooled hazard ratios (HRs) were calculated using random-effects models where appropriate.
Results: Eleven studies encompassing 377,789 participants were included. Waitlist mortality (5 studies) showed a significantly increased risk for women (pooled HR 1.16, 95% CI: 1.11–1.20; p < 0.001; I² = 48%). The effect was particularly pronounced for frail men versus non-frail women (HR 3.4; p = 0.03), but became non-significant after adjusting for height (HR 1.05, 95% CI: 0.98–1.12).
Transplantation access (3 studies) revealed reduced access for women (pooled HR 0.88, 95% CI: 0.86–0.90; p < 0.001), with substantial heterogeneity (I² = 94%) reflecting variation in access pathways. Women had decreased odds of receiving deceased donor transplantation (HR 0.86, 95% CI: 0.84–0.88) and over twice the risk of not accessing living donor transplantation when MELD-Na < 20 (HR 2.04, 95% CI: 1.31–3.14).
Post-transplant outcomes demonstrated time-dependent effects: women experienced 5% longer hospital stays (adjusted IRR 1.05, 95% CI: 1.02–1.08), a 22% higher short-term mortality risk (HR 1.22, 95% CI: 1.03–1.44), but a 6% lower long-term mortality risk (HR 0.94, 95% CI: 0.89–0.99).
Discussion: Across the liver transplant continuum, women face significant and consistent disadvantages, including elevated waitlist mortality and reduced access to transplantation. Although post-transplant outcomes vary over time, the overall findings highlight the need for gender-sensitive policies and clinical decision-making to reduce disparities in liver transplantation.
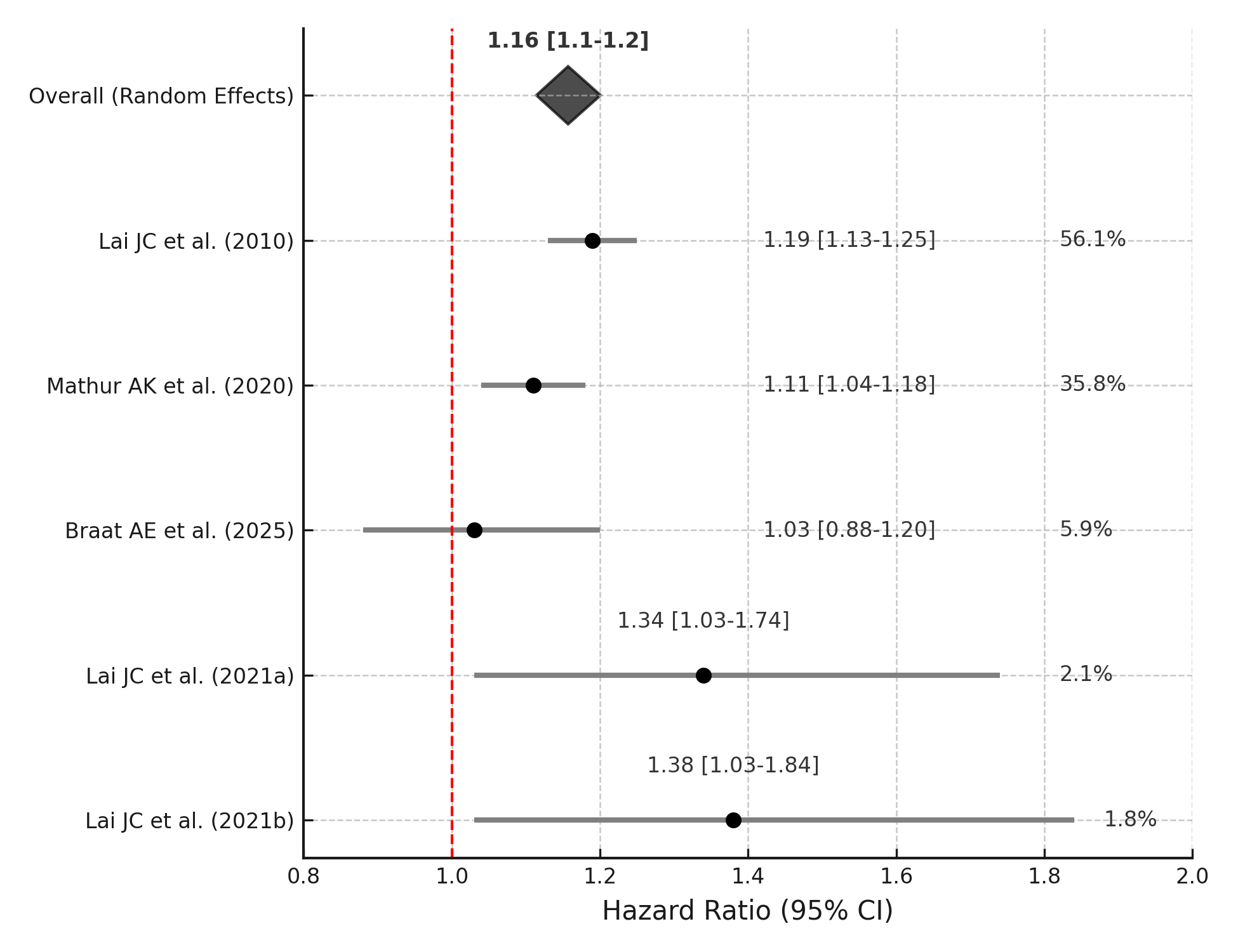
Figure: Figure 1. PRISMA Flow Diagram
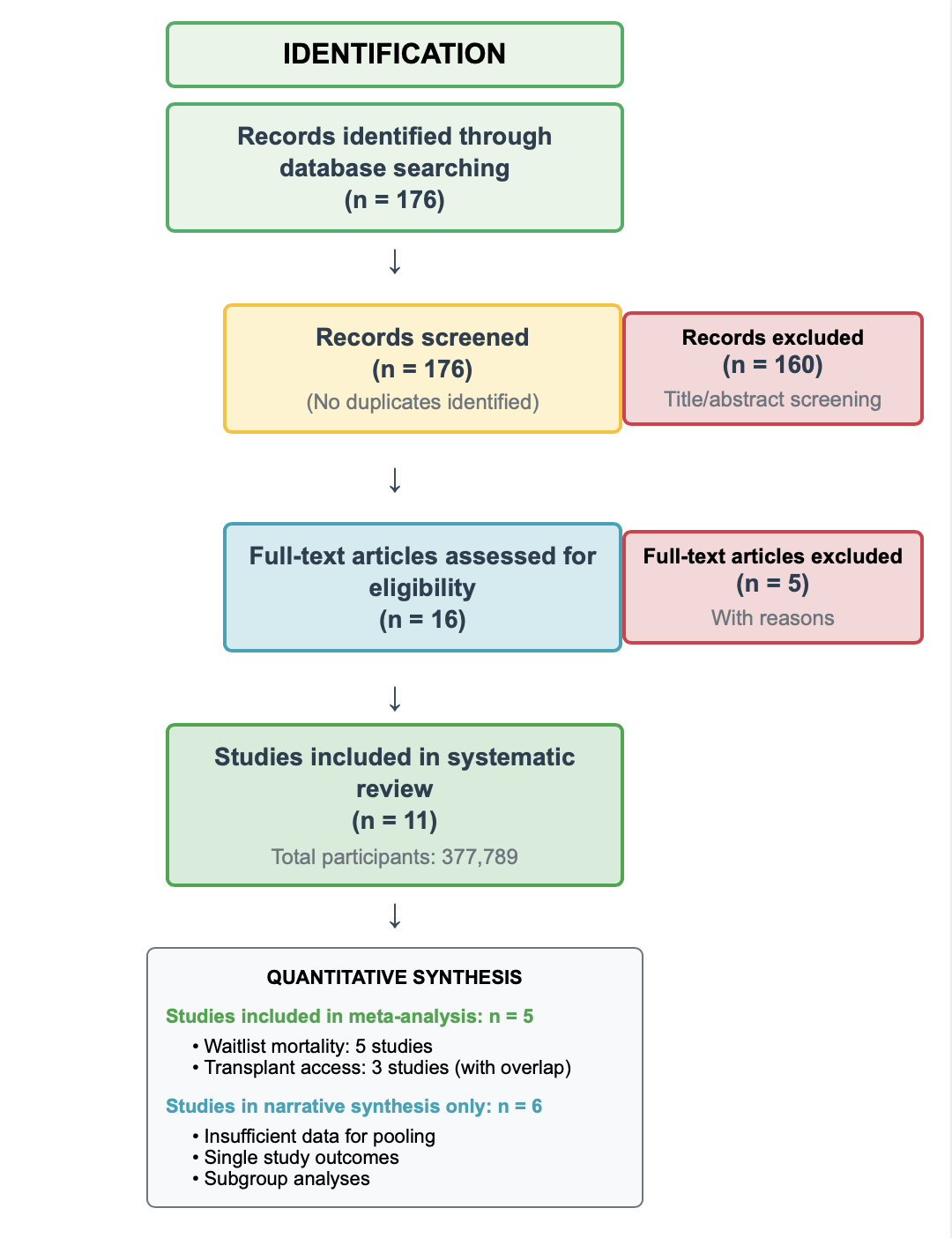
Figure: Figure 2. Forest plot showing higher waitlist mortality risk for women (pooled HR 1.16, 95% CI: 1.11–1.20). Pooled estimate shown as a diamond; red line indicates no effect (HR = 1).
Disclosures:
John Appiah indicated no relevant financial relationships.
George Blewusi indicated no relevant financial relationships.
Ewurabena Plange-Kaye indicated no relevant financial relationships.
Richeal Asante indicated no relevant financial relationships.
Edward Danso indicated no relevant financial relationships.
Emmanuel Asiedu indicated no relevant financial relationships.
John K. Appiah, MD1, George S. Blewusi, MD2, Ewurabena N. Plange-Kaye, DDS3, Richeal Asante, MD4, Edward A. Danso, MD5, Emmanuel Asiedu, MD6. P1526 - Gender Disparities in Liver Transplantation: A Systematic Review and Meta-Analysis of Access, Waitlist Outcomes, and Post-Transplant Survival, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 2Johns Hopkins Bloomberg School of Public Health, Baltimore, MD; 3Columbia University, Dumont, NJ; 4Geisinger Wyoming Valley Medical Center, Kingston, PA; 5Korle-Bu Teaching Hospital, Accra, Greater Accra, Ghana; 6Mother and Child Hospital, Accra, Central, Ghana
Introduction: Gender disparities in liver transplantation have emerged as a critical equity issue, with growing evidence suggesting systematic disadvantages for women throughout the transplant process. While individual studies have reported gender differences in waitlist mortality, transplant access, and post-transplant outcomes, comprehensive quantitative synthesis of this evidence remains lacking. Understanding the magnitude and consistency of these disparities is essential for informing policy reforms and clinical practice improvements.
Methods: We systematically searched PubMed, Cochrane, and Google Scholar databases (2005–2024) for studies reporting gender-stratified outcomes in adult liver transplant candidates or recipients. This review was registered with PROSPERO (CRD420251039195). We included original peer-reviewed studies reporting adjusted effect estimates for transplant rate, waitlist mortality, or post-transplant outcomes. Pooled hazard ratios (HRs) were calculated using random-effects models where appropriate.
Results: Eleven studies encompassing 377,789 participants were included. Waitlist mortality (5 studies) showed a significantly increased risk for women (pooled HR 1.16, 95% CI: 1.11–1.20; p < 0.001; I² = 48%). The effect was particularly pronounced for frail men versus non-frail women (HR 3.4; p = 0.03), but became non-significant after adjusting for height (HR 1.05, 95% CI: 0.98–1.12).
Transplantation access (3 studies) revealed reduced access for women (pooled HR 0.88, 95% CI: 0.86–0.90; p < 0.001), with substantial heterogeneity (I² = 94%) reflecting variation in access pathways. Women had decreased odds of receiving deceased donor transplantation (HR 0.86, 95% CI: 0.84–0.88) and over twice the risk of not accessing living donor transplantation when MELD-Na < 20 (HR 2.04, 95% CI: 1.31–3.14).
Post-transplant outcomes demonstrated time-dependent effects: women experienced 5% longer hospital stays (adjusted IRR 1.05, 95% CI: 1.02–1.08), a 22% higher short-term mortality risk (HR 1.22, 95% CI: 1.03–1.44), but a 6% lower long-term mortality risk (HR 0.94, 95% CI: 0.89–0.99).
Discussion: Across the liver transplant continuum, women face significant and consistent disadvantages, including elevated waitlist mortality and reduced access to transplantation. Although post-transplant outcomes vary over time, the overall findings highlight the need for gender-sensitive policies and clinical decision-making to reduce disparities in liver transplantation.
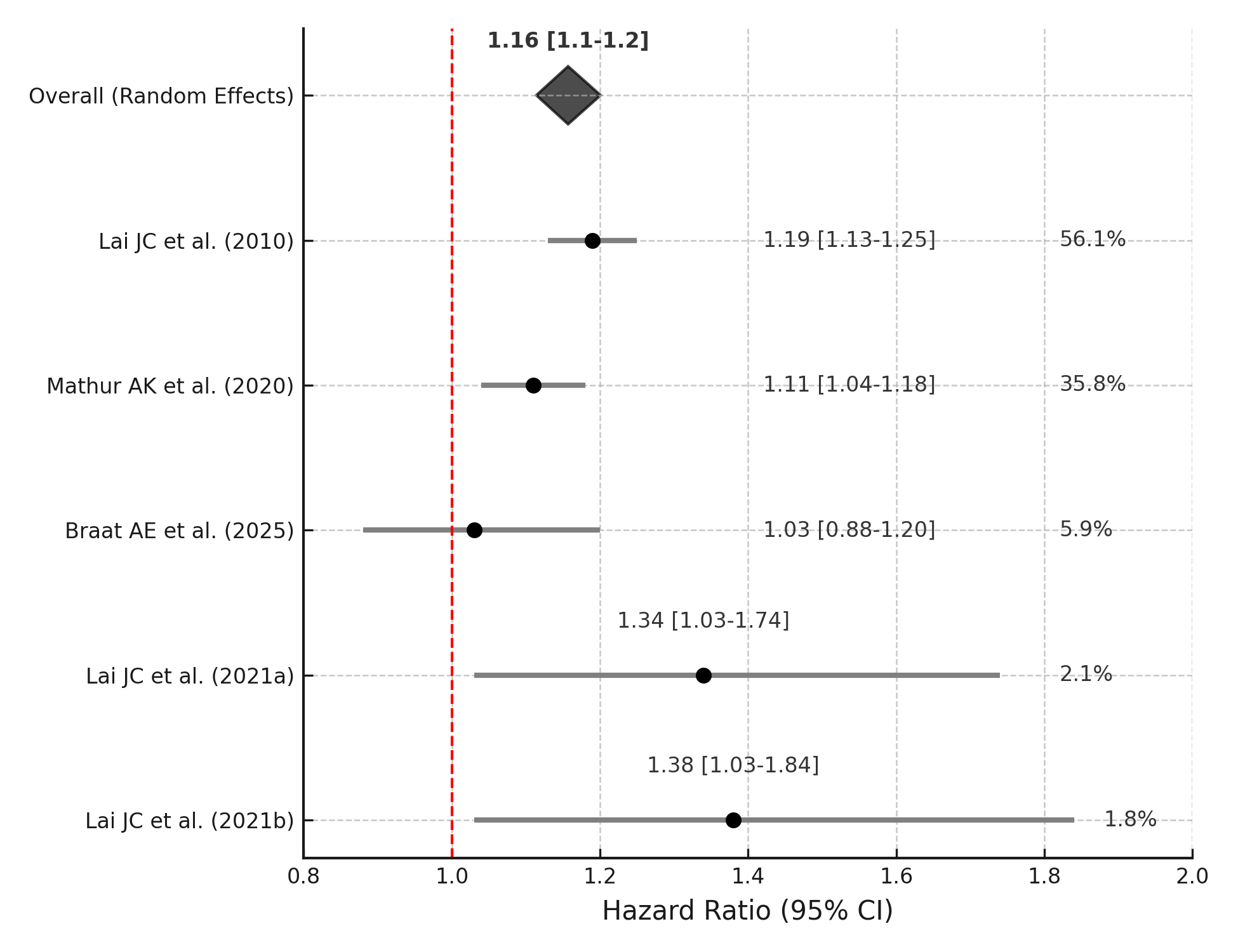
Figure: Figure 1. PRISMA Flow Diagram
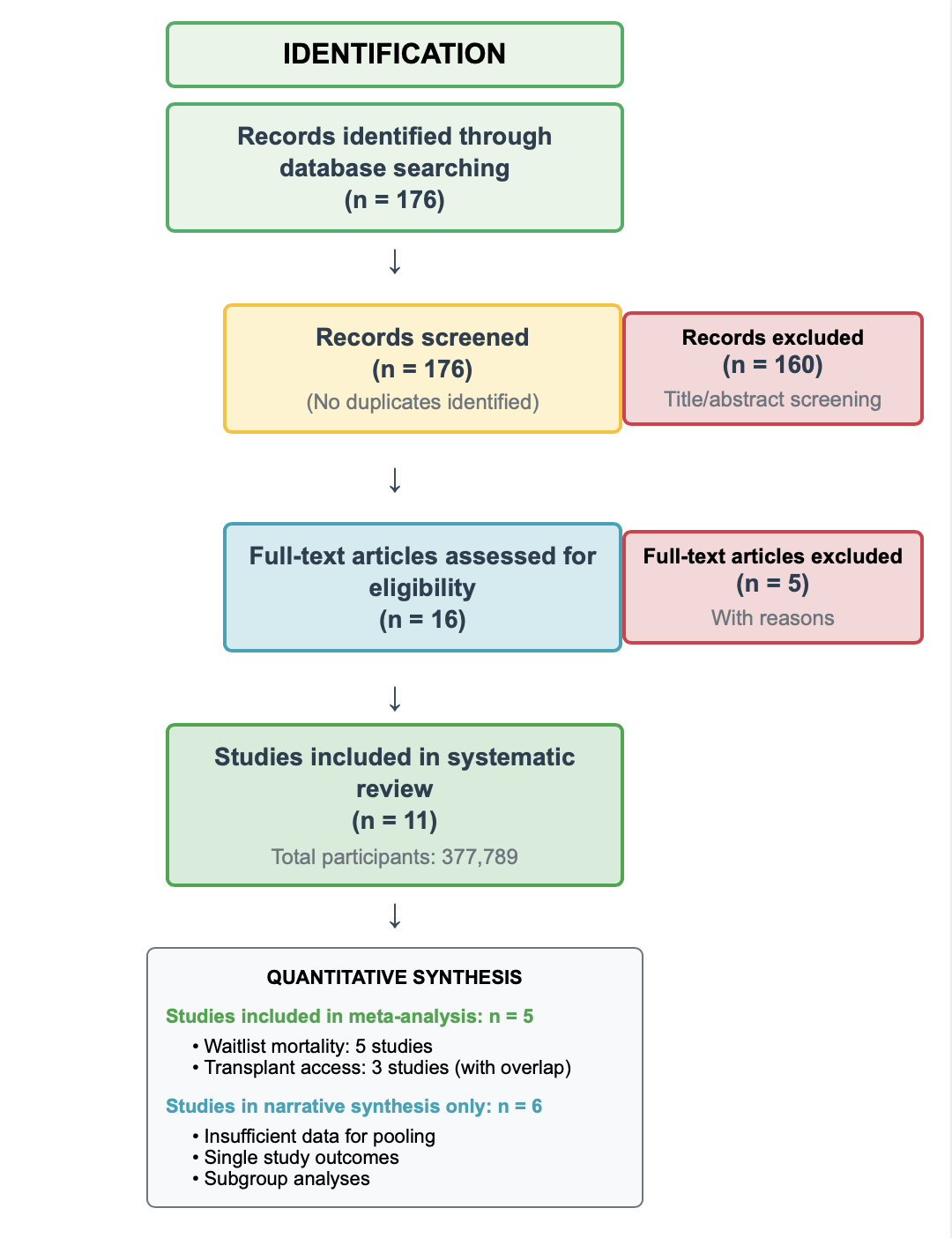
Figure: Figure 2. Forest plot showing higher waitlist mortality risk for women (pooled HR 1.16, 95% CI: 1.11–1.20). Pooled estimate shown as a diamond; red line indicates no effect (HR = 1).
Disclosures:
John Appiah indicated no relevant financial relationships.
George Blewusi indicated no relevant financial relationships.
Ewurabena Plange-Kaye indicated no relevant financial relationships.
Richeal Asante indicated no relevant financial relationships.
Edward Danso indicated no relevant financial relationships.
Emmanuel Asiedu indicated no relevant financial relationships.
John K. Appiah, MD1, George S. Blewusi, MD2, Ewurabena N. Plange-Kaye, DDS3, Richeal Asante, MD4, Edward A. Danso, MD5, Emmanuel Asiedu, MD6. P1526 - Gender Disparities in Liver Transplantation: A Systematic Review and Meta-Analysis of Access, Waitlist Outcomes, and Post-Transplant Survival, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

