Sunday Poster Session
Category: Liver
P1499 - SAFE vs FIB-4: A Comparative Analysis of Diagnostic Accuracy in Screening for Clinically Significant Fibrosis Using NHANES Data
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Adem Aydin, MD (he/him/his)
Saint Mary's Hospital
Chehire, CT
Presenting Author(s)
Adem Aydin, MD1
1Saint Mary's Hospital, Chehire, CT
Introduction: Steatotic liver disease (SLD), primarily driven by cardiometabolic dysfunction, affects nearly one-third of the global population and poses a growing public health challenge. Disease progression may lead to advanced liver fibrosis. Although liver biopsy remains the gold standard for assessing fibrosis, its invasive nature has prompted the adoption of non-invasive diagnostic tools. Among these, the Fibrosis-4 (FIB-4) index and the Steatosis-Associated Fibrosis Estimator (SAFE) score are commonly used in clinical and research settings. This study aimed to compare the diagnostic accuracy of FIB-4 and SAFE in detecting clinically significant fibrosis in individuals with cardiometabolic risk factors
Methods: We conducted a cross-sectional analysis using data from 2,196 adults in the NHANES 2017–2020 cycles. Participants aged 18–80 years with valid liver stiffness measurements (LSM) by FibroScan were included. We excluded individuals with known chronic liver disease, self-reported excessive alcohol use, or missing data required to calculate FIB-4 or SAFE scores. Clinically significant fibrosis was defined as LSM ≥ 8.0 kPa.We evaluated diagnostic performance using sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and ROC curve analysis. McNemar’s test assessed paired differences, and DeLong’s test compared AUCs. Generative AI tools (ChatGPT models O1, O3) were used to assist with code development, data visualization, and proofreading.
Results: The SAFE score demonstrated a higher AUC than FIB-4 (0.719 vs. 0.578, p < 0.001). As a rule-out test, SAFE showed superior sensitivity (78%) and NPV (95%) compared to FIB-4 (sensitivity: 41%, NPV: 91%). FIB-4 missed 58.6% of patients with significant fibrosis, while SAFE missed 22%. While both tests demonstrated high specificity for ruling in fibrosis (FIB-4: 97.8%, SAFE: 86.5%), their low sensitivity limits their reliability for confirming the disease.Subgroup analysis showed that SAFE maintained better diagnostic accuracy across age groups, sex, and presence of MASLD. In contrast, FIB-4 performed especially poorly in younger adults.
Discussion: These findings support the use of SAFE over FIB-4 as a non-invasive screening tool for significant fibrosis in patients with cardiometabolic risk factors. Further studies are warranted to improve and validate fibrosis screening tools, especially for those at risk for MASLD.
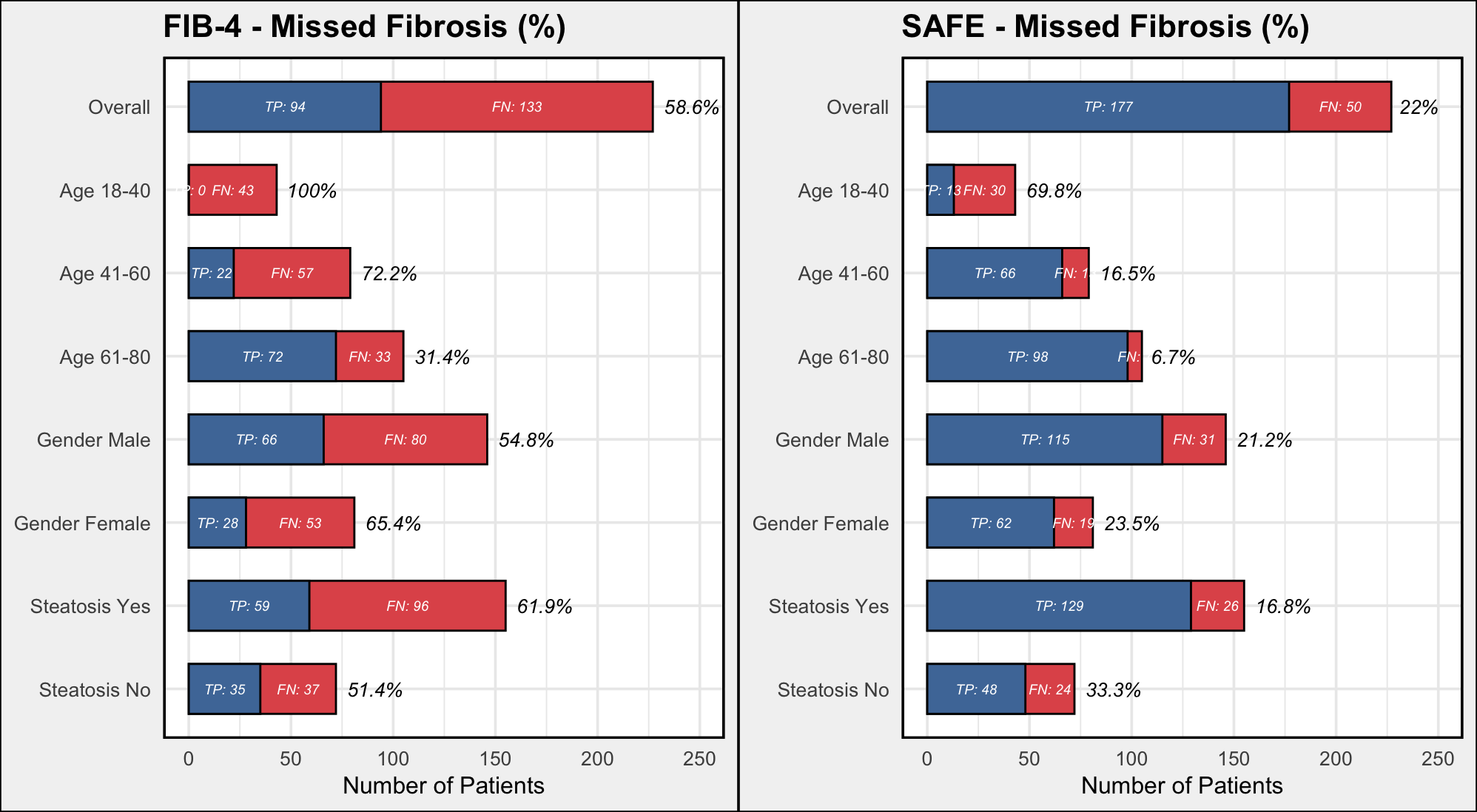
Figure: Figure 1. Percentage of Missed Fibrosis Cases: FIB-4 vs. SAFE
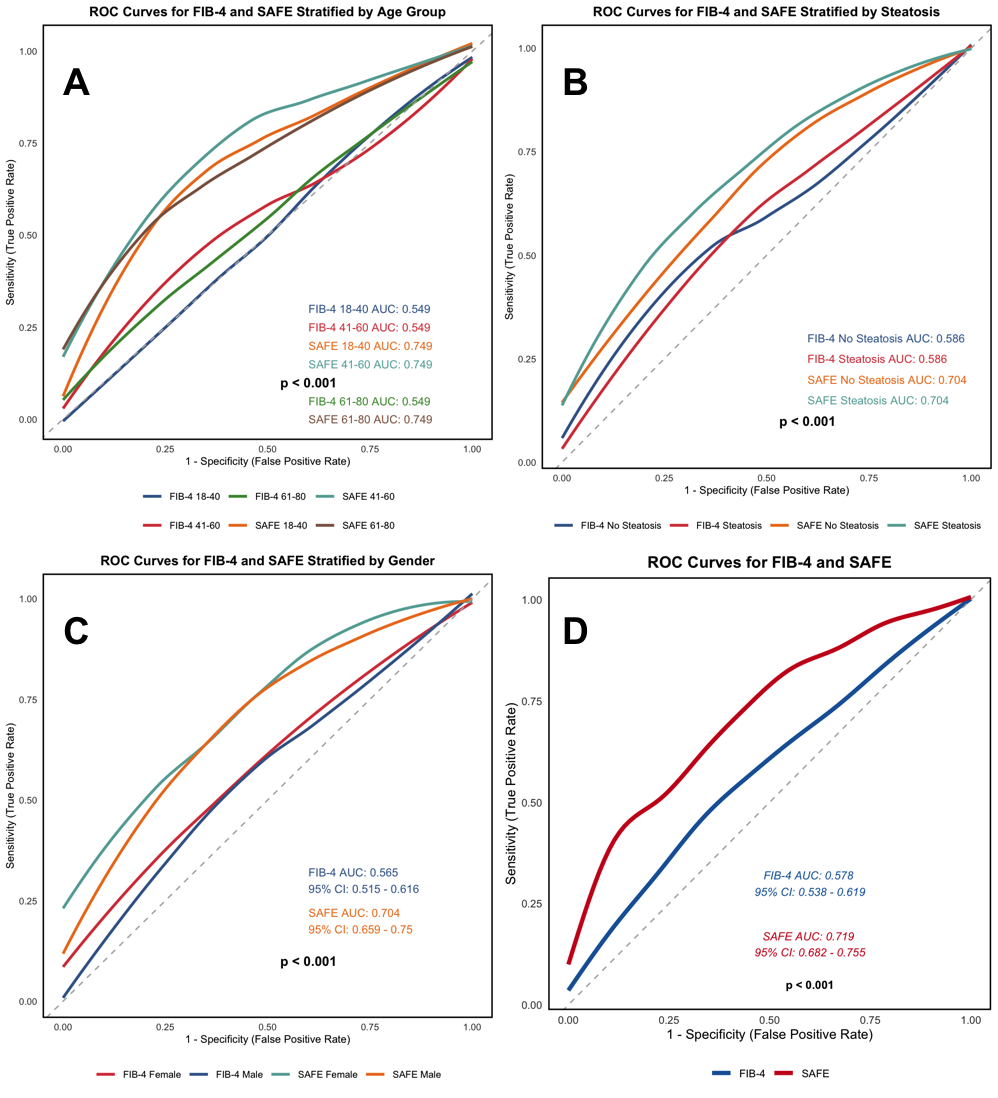
Figure: Figure 2. ROC Curves for SAFE vs. FIB-4 Stratified by Age, Gender, and MASLD
Disclosures:
Adem Aydin indicated no relevant financial relationships.
Adem Aydin, MD1. P1499 - SAFE vs FIB-4: A Comparative Analysis of Diagnostic Accuracy in Screening for Clinically Significant Fibrosis Using NHANES Data, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Saint Mary's Hospital, Chehire, CT
Introduction: Steatotic liver disease (SLD), primarily driven by cardiometabolic dysfunction, affects nearly one-third of the global population and poses a growing public health challenge. Disease progression may lead to advanced liver fibrosis. Although liver biopsy remains the gold standard for assessing fibrosis, its invasive nature has prompted the adoption of non-invasive diagnostic tools. Among these, the Fibrosis-4 (FIB-4) index and the Steatosis-Associated Fibrosis Estimator (SAFE) score are commonly used in clinical and research settings. This study aimed to compare the diagnostic accuracy of FIB-4 and SAFE in detecting clinically significant fibrosis in individuals with cardiometabolic risk factors
Methods: We conducted a cross-sectional analysis using data from 2,196 adults in the NHANES 2017–2020 cycles. Participants aged 18–80 years with valid liver stiffness measurements (LSM) by FibroScan were included. We excluded individuals with known chronic liver disease, self-reported excessive alcohol use, or missing data required to calculate FIB-4 or SAFE scores. Clinically significant fibrosis was defined as LSM ≥ 8.0 kPa.We evaluated diagnostic performance using sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and ROC curve analysis. McNemar’s test assessed paired differences, and DeLong’s test compared AUCs. Generative AI tools (ChatGPT models O1, O3) were used to assist with code development, data visualization, and proofreading.
Results: The SAFE score demonstrated a higher AUC than FIB-4 (0.719 vs. 0.578, p < 0.001). As a rule-out test, SAFE showed superior sensitivity (78%) and NPV (95%) compared to FIB-4 (sensitivity: 41%, NPV: 91%). FIB-4 missed 58.6% of patients with significant fibrosis, while SAFE missed 22%. While both tests demonstrated high specificity for ruling in fibrosis (FIB-4: 97.8%, SAFE: 86.5%), their low sensitivity limits their reliability for confirming the disease.Subgroup analysis showed that SAFE maintained better diagnostic accuracy across age groups, sex, and presence of MASLD. In contrast, FIB-4 performed especially poorly in younger adults.
Discussion: These findings support the use of SAFE over FIB-4 as a non-invasive screening tool for significant fibrosis in patients with cardiometabolic risk factors. Further studies are warranted to improve and validate fibrosis screening tools, especially for those at risk for MASLD.
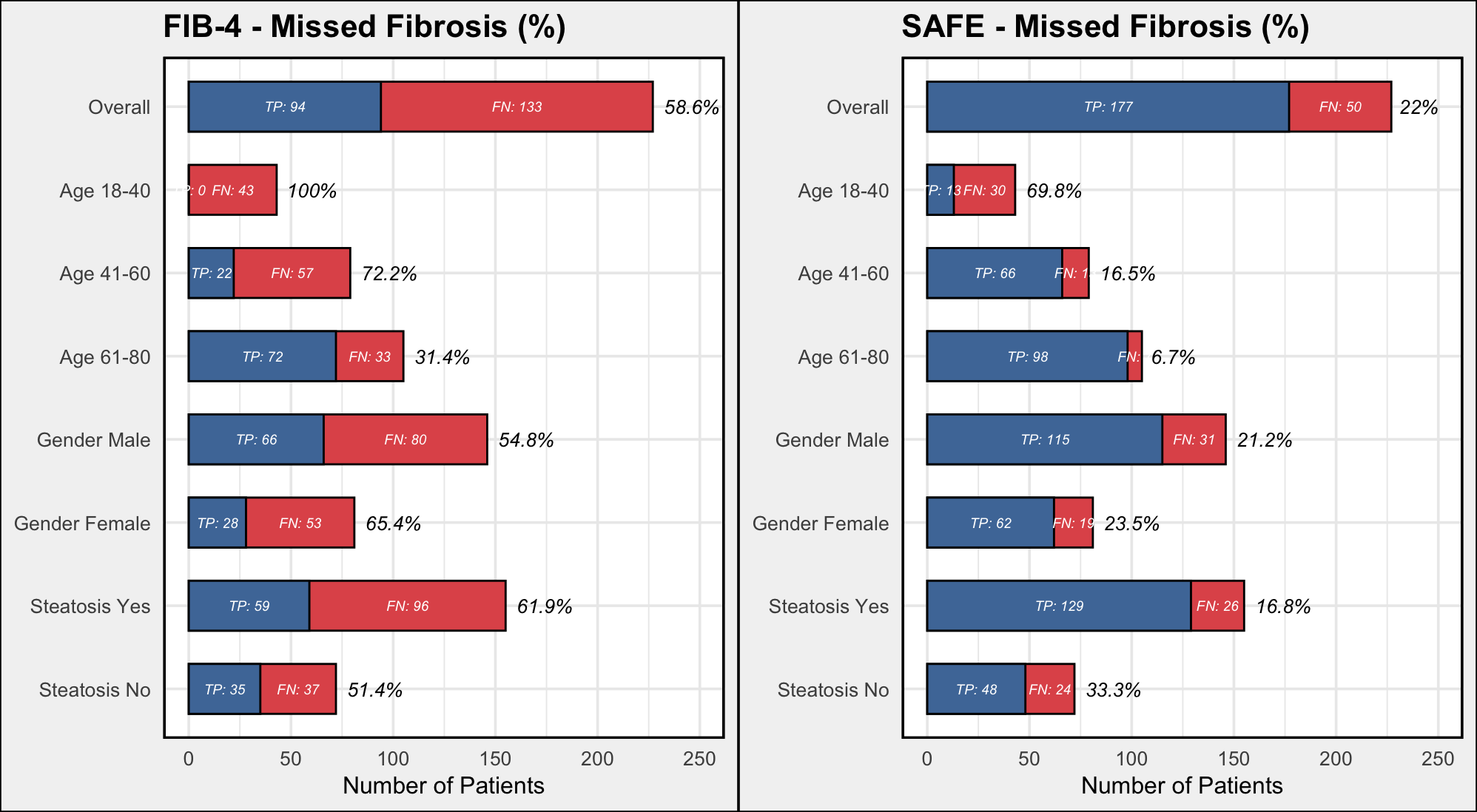
Figure: Figure 1. Percentage of Missed Fibrosis Cases: FIB-4 vs. SAFE
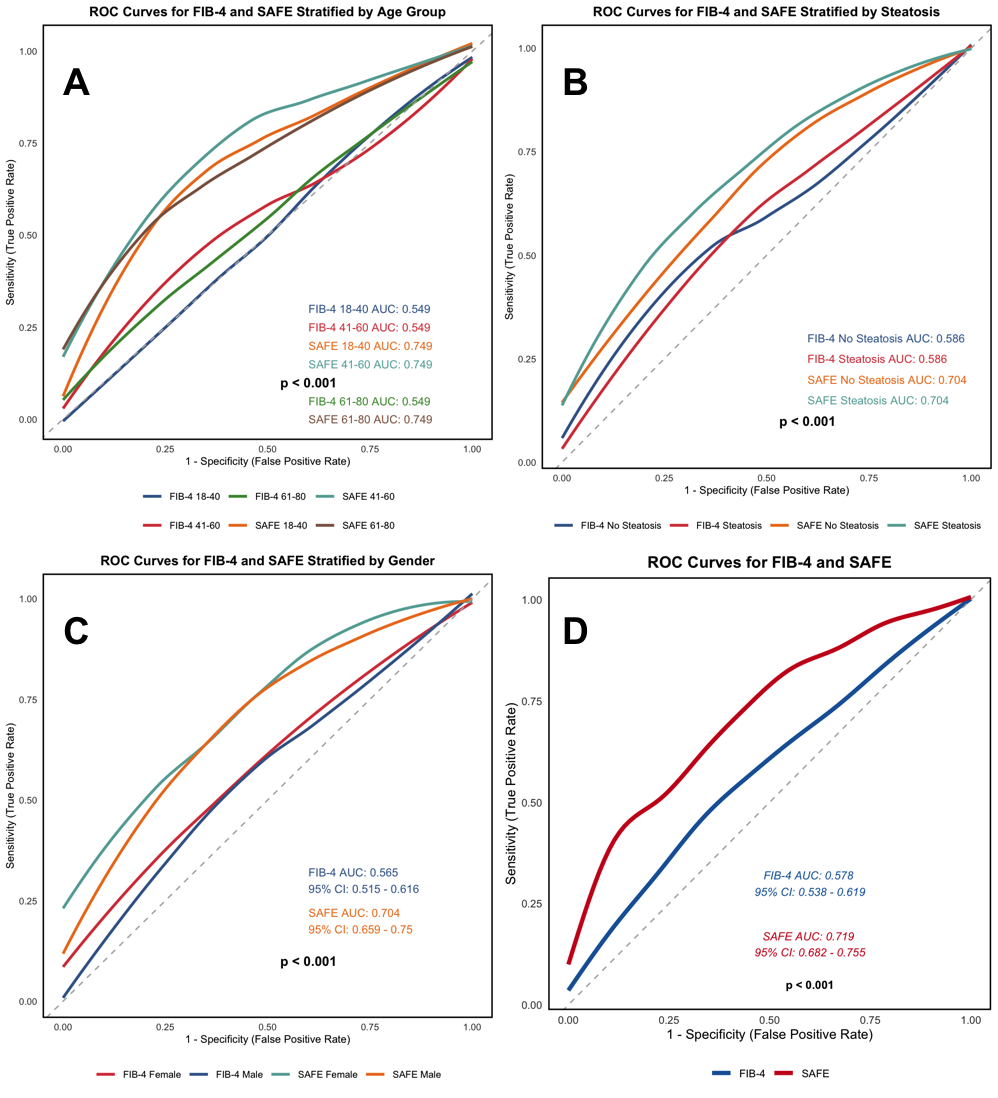
Figure: Figure 2. ROC Curves for SAFE vs. FIB-4 Stratified by Age, Gender, and MASLD
Disclosures:
Adem Aydin indicated no relevant financial relationships.
Adem Aydin, MD1. P1499 - SAFE vs FIB-4: A Comparative Analysis of Diagnostic Accuracy in Screening for Clinically Significant Fibrosis Using NHANES Data, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
