Sunday Poster Session
Category: Interventional Endoscopy
P1450 - Unmasking Gastric Adenocarcinoma: Diagnostic Yield of EUS-Guided Fine Needle Biopsy in a Patient with Negative Conventional Workup
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Amro Altarawneh, MD
Marshall University Joan C. Edwards School of Medicine
Huntington, WV
Presenting Author(s)
Amro Altarawneh, MD, Yasmeen Obeidat, MD, Ahmed Sherif, MD, Wesam Frandah, MD
Marshall University Joan C. Edwards School of Medicine, Huntington, WV
Introduction: Gastric adenocarcinoma can present insidiously, particularly when initial endoscopy and biopsies are non-revealing. This case highlights the diagnostic utility of endoscopic ultrasound-guided fine needle biopsy (EUS-FNB) in detecting infiltrative malignancy.
Case Description/
Methods: A 54-year-old male with a recent cholecystectomy presented with epigastric pain, nausea, vomiting, and weight loss. Liver enzymes and total bilirubin were normal. Initial upper endoscopy and colonoscopy with biopsies of the stomach and duodenum were negative. CT abdomen revealed distal gastric wall thickening and mild ascites. A gastric emptying study was normal. Due to persistent symptoms, repeat EGD showed diffuse moderate inflammation with congestion, erythema, and granularity throughout the stomach, and a clean-based antral ulcer (Forrest III). Biopsies again showed only reactive changes.
Given high suspicion for malignancy, EUS was performed, revealing diffuse thickening (11 mm) of the gastric wall with loss of normal wall layer differentiation. EUS-guided FNB using a 19 gauge needle was performed. Histopathology demonstrated poorly differentiated adenocarcinoma with positive CDX2 staining, confirming gastrointestinal origin.
Discussion: This case illustrates the limitations of mucosal biopsies in detecting subepithelial gastric cancer. Despite repeated negative biopsies, persistent symptoms and imaging findings warranted further evaluation. EUS not only revealed structural abnormalities but enabled definitive diagnosis through tissue acquisition. The use of CDX2 immunostaining supported the gastric origin of the adenocarcinoma.
Infiltrative gastric cancer may elude standard endoscopic biopsies. EUS-FNB is a crucial diagnostic tool in patients with concerning clinical features and inconclusive initial workup, facilitating timely diagnosis and treatment.
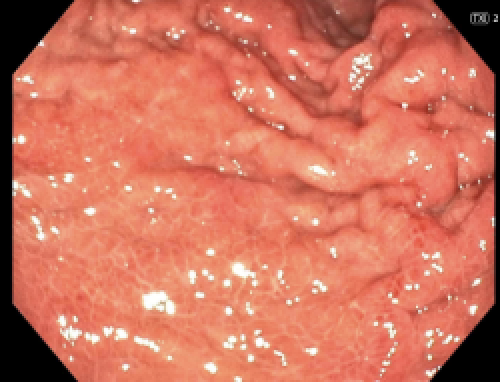
Figure: Endoscopic images showing diffuse mucosal erythema, granularity, and congestion throughout the gastric body and antrum, raising suspicion for infiltrative disease despite negative mucosal biopsies.
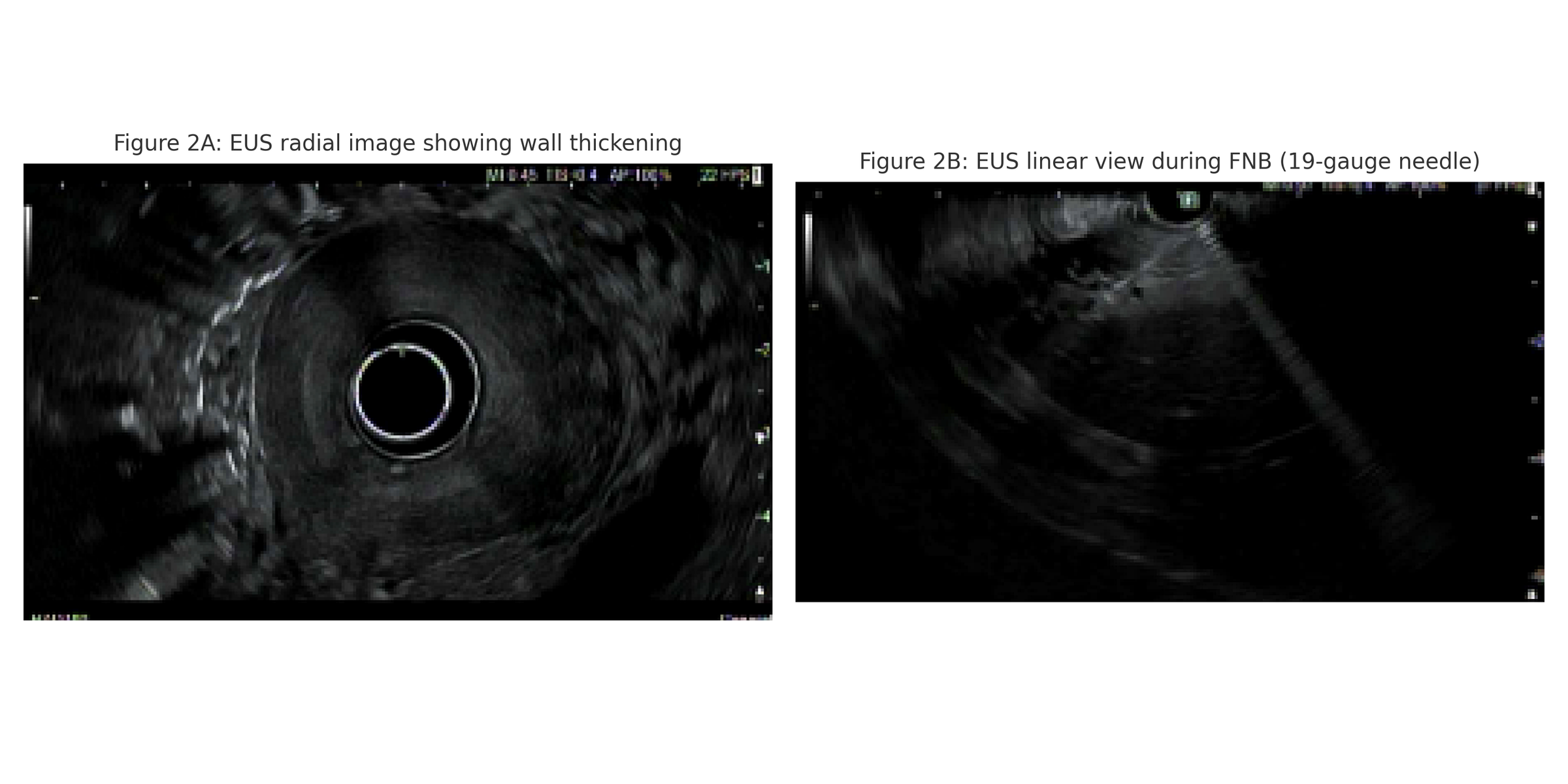
Figure: (A) Endoscopic ultrasound (EUS) radial image demonstrating marked gastric wall thickening with loss of normal stratified architecture.
(B) EUS linear image with 19-gauge fine needle biopsy in progress, targeting the thickened gastric wall for tissue acquisition.
Disclosures:
Amro Altarawneh indicated no relevant financial relationships.
Yasmeen Obeidat indicated no relevant financial relationships.
Ahmed Sherif indicated no relevant financial relationships.
Wesam Frandah: Boston Scientific – Advisor or Review Panel Member, Consultant. Merritt – Consultant. Olympus corporation of America – Consultant.
Amro Altarawneh, MD, Yasmeen Obeidat, MD, Ahmed Sherif, MD, Wesam Frandah, MD. P1450 - Unmasking Gastric Adenocarcinoma: Diagnostic Yield of EUS-Guided Fine Needle Biopsy in a Patient with Negative Conventional Workup, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Marshall University Joan C. Edwards School of Medicine, Huntington, WV
Introduction: Gastric adenocarcinoma can present insidiously, particularly when initial endoscopy and biopsies are non-revealing. This case highlights the diagnostic utility of endoscopic ultrasound-guided fine needle biopsy (EUS-FNB) in detecting infiltrative malignancy.
Case Description/
Methods: A 54-year-old male with a recent cholecystectomy presented with epigastric pain, nausea, vomiting, and weight loss. Liver enzymes and total bilirubin were normal. Initial upper endoscopy and colonoscopy with biopsies of the stomach and duodenum were negative. CT abdomen revealed distal gastric wall thickening and mild ascites. A gastric emptying study was normal. Due to persistent symptoms, repeat EGD showed diffuse moderate inflammation with congestion, erythema, and granularity throughout the stomach, and a clean-based antral ulcer (Forrest III). Biopsies again showed only reactive changes.
Given high suspicion for malignancy, EUS was performed, revealing diffuse thickening (11 mm) of the gastric wall with loss of normal wall layer differentiation. EUS-guided FNB using a 19 gauge needle was performed. Histopathology demonstrated poorly differentiated adenocarcinoma with positive CDX2 staining, confirming gastrointestinal origin.
Discussion: This case illustrates the limitations of mucosal biopsies in detecting subepithelial gastric cancer. Despite repeated negative biopsies, persistent symptoms and imaging findings warranted further evaluation. EUS not only revealed structural abnormalities but enabled definitive diagnosis through tissue acquisition. The use of CDX2 immunostaining supported the gastric origin of the adenocarcinoma.
Infiltrative gastric cancer may elude standard endoscopic biopsies. EUS-FNB is a crucial diagnostic tool in patients with concerning clinical features and inconclusive initial workup, facilitating timely diagnosis and treatment.
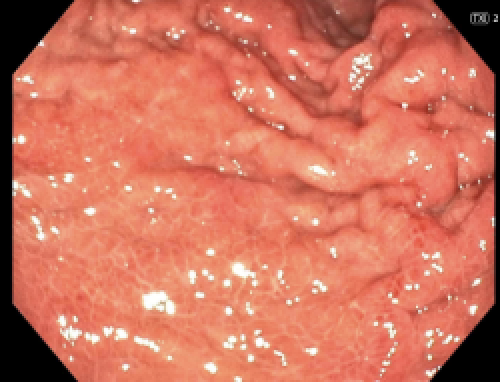
Figure: Endoscopic images showing diffuse mucosal erythema, granularity, and congestion throughout the gastric body and antrum, raising suspicion for infiltrative disease despite negative mucosal biopsies.
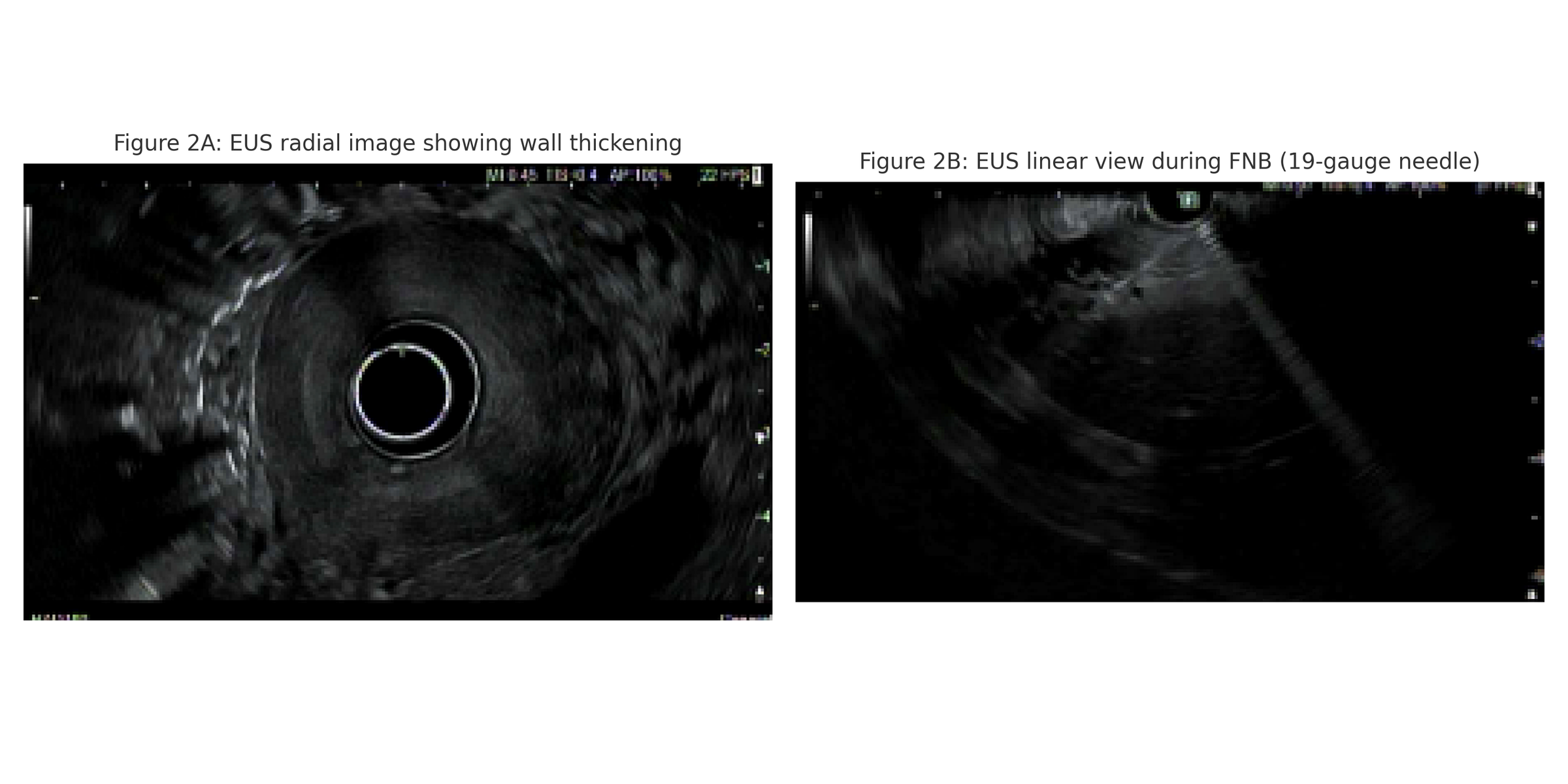
Figure: (A) Endoscopic ultrasound (EUS) radial image demonstrating marked gastric wall thickening with loss of normal stratified architecture.
(B) EUS linear image with 19-gauge fine needle biopsy in progress, targeting the thickened gastric wall for tissue acquisition.
Disclosures:
Amro Altarawneh indicated no relevant financial relationships.
Yasmeen Obeidat indicated no relevant financial relationships.
Ahmed Sherif indicated no relevant financial relationships.
Wesam Frandah: Boston Scientific – Advisor or Review Panel Member, Consultant. Merritt – Consultant. Olympus corporation of America – Consultant.
Amro Altarawneh, MD, Yasmeen Obeidat, MD, Ahmed Sherif, MD, Wesam Frandah, MD. P1450 - Unmasking Gastric Adenocarcinoma: Diagnostic Yield of EUS-Guided Fine Needle Biopsy in a Patient with Negative Conventional Workup, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
