Sunday Poster Session
Category: Interventional Endoscopy
P1447 - Snare Resection of a Polypoid Biliary Lesion via Cholangioscopy in a Patient With Cirrhotic Liver Disease
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Maria Krantz, BS, MPH
The Ohio State University Wexner Medical Center
Columbus, OH
Presenting Author(s)
Hong T. Lin, MD, Maria Krantz, BS, MPH, Fred Karaisz, MD, Fadi Hawa, MD, Jordan Burlen, MD
The Ohio State University Wexner Medical Center, Columbus, OH
Introduction: Cholangioscopy has become an increasingly valuable tool for the diagnosis and management of biliary strictures, driven by ongoing technological advancements. Intraductal biliary lesions can range from benign reactive changes to malignancy. In this report, we describe a unique case of snare resection via cholangioscopy to remove a polypoid biliary lesion in a patient with cirrhosis.
Case Description/
Methods: A 63-year-old man with metabolic dysfunction-associated steatohepatitis (MASH) cirrhosis and non-occlusive portal vein thrombosis (PVT) presented with cholangitis. Initial computed tomography (CT) revealed congenital gallbladder agenesis, distal common bile duct (CBD) choledocholithiasis, pneumobilia, and hepatic abscesses (Figure 1A). He underwent endoscopic retrograde cholangiopancreatography (ERCP) with sphincterotomy, stone extraction, and plastic stent placement. Six months later, repeat ERCP was performed for stent removal and extraction of residual bile duct stones. Cholangioscopy identified multiple polypoid lesions in the mid-CBD (Figure 1B). Biopsies showed polypoid biliary mucosa with inflammatory changes. Given the concern for possible underlying malignancy, a follow-up ERCP with cholangioscopy was performed. A SpyGlass® snare was used to resect a larger tissue sample of the polypoid lesion (Figure 1C) for histological analysis, confirming its benign inflammatory nature. The patient remains under close surveillance with serial liver function tests.
Discussion: Advances in cholangioscopy have broadened its diagnostic and therapeutic role, particularly in biliary strictures, where biopsy sensitivity for malignancy remains limited (72%). While the SpyGlass® snare is typically used for stone extraction and stent removal, our case highlights its potential for resecting intraductal polypoid lesions. Cirrhosis substantially elevates cholangiocarcinoma risk via chronic inflammation, biliary stasis, and gut dysbiosis. Given the constraints of standard biliary sampling techniques, cholangioscopic snare polypectomy offers a therapeutic option in select biliary obstructions and for excluding malignancy. In this patient, the polypoid biliary mucosa with epithelial hyperplasia represented a benign reactive process, typically linked to chronic inflammation or biliary irritation, and was likely driven by choledocholithiasis and underlying cirrhotic liver disease.
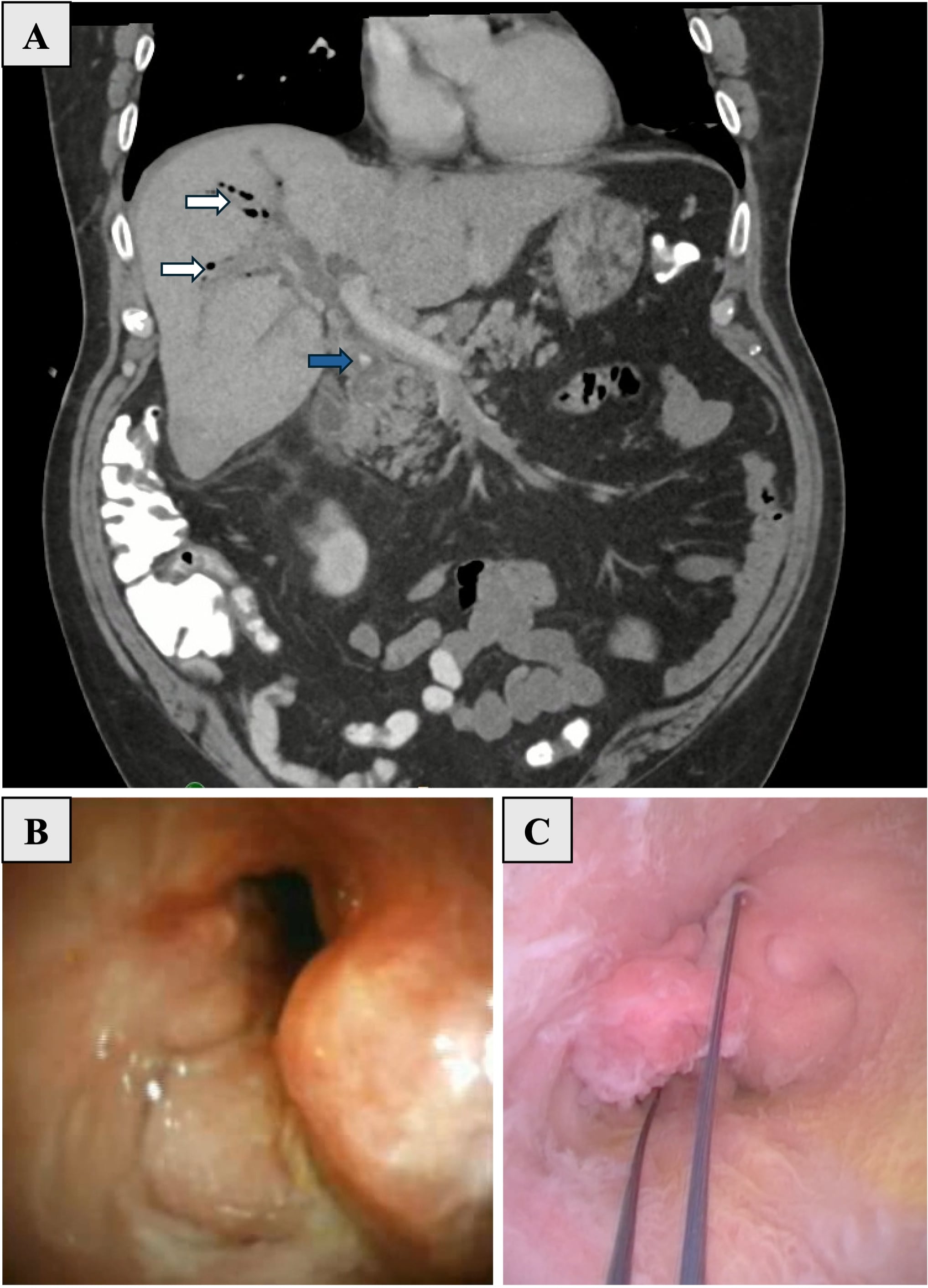
Figure: Figure 1: Coronal CT (Panel A) demonstrating choledocholithiasis (blue arrow) associated with pneumobilia (white arrows), portal vein thrombosis, and possible hepatic abscesses. Cholangioscopy (Panel B) with abnormal polypoid biliary mucosa. Snare resection of mid-CBD polypoid lesion (Panel C).
Disclosures:
Hong Lin indicated no relevant financial relationships.
Maria Krantz indicated no relevant financial relationships.
Fred Karaisz indicated no relevant financial relationships.
Fadi Hawa indicated no relevant financial relationships.
Jordan Burlen indicated no relevant financial relationships.
Hong T. Lin, MD, Maria Krantz, BS, MPH, Fred Karaisz, MD, Fadi Hawa, MD, Jordan Burlen, MD. P1447 - Snare Resection of a Polypoid Biliary Lesion via Cholangioscopy in a Patient With Cirrhotic Liver Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
The Ohio State University Wexner Medical Center, Columbus, OH
Introduction: Cholangioscopy has become an increasingly valuable tool for the diagnosis and management of biliary strictures, driven by ongoing technological advancements. Intraductal biliary lesions can range from benign reactive changes to malignancy. In this report, we describe a unique case of snare resection via cholangioscopy to remove a polypoid biliary lesion in a patient with cirrhosis.
Case Description/
Methods: A 63-year-old man with metabolic dysfunction-associated steatohepatitis (MASH) cirrhosis and non-occlusive portal vein thrombosis (PVT) presented with cholangitis. Initial computed tomography (CT) revealed congenital gallbladder agenesis, distal common bile duct (CBD) choledocholithiasis, pneumobilia, and hepatic abscesses (Figure 1A). He underwent endoscopic retrograde cholangiopancreatography (ERCP) with sphincterotomy, stone extraction, and plastic stent placement. Six months later, repeat ERCP was performed for stent removal and extraction of residual bile duct stones. Cholangioscopy identified multiple polypoid lesions in the mid-CBD (Figure 1B). Biopsies showed polypoid biliary mucosa with inflammatory changes. Given the concern for possible underlying malignancy, a follow-up ERCP with cholangioscopy was performed. A SpyGlass® snare was used to resect a larger tissue sample of the polypoid lesion (Figure 1C) for histological analysis, confirming its benign inflammatory nature. The patient remains under close surveillance with serial liver function tests.
Discussion: Advances in cholangioscopy have broadened its diagnostic and therapeutic role, particularly in biliary strictures, where biopsy sensitivity for malignancy remains limited (72%). While the SpyGlass® snare is typically used for stone extraction and stent removal, our case highlights its potential for resecting intraductal polypoid lesions. Cirrhosis substantially elevates cholangiocarcinoma risk via chronic inflammation, biliary stasis, and gut dysbiosis. Given the constraints of standard biliary sampling techniques, cholangioscopic snare polypectomy offers a therapeutic option in select biliary obstructions and for excluding malignancy. In this patient, the polypoid biliary mucosa with epithelial hyperplasia represented a benign reactive process, typically linked to chronic inflammation or biliary irritation, and was likely driven by choledocholithiasis and underlying cirrhotic liver disease.
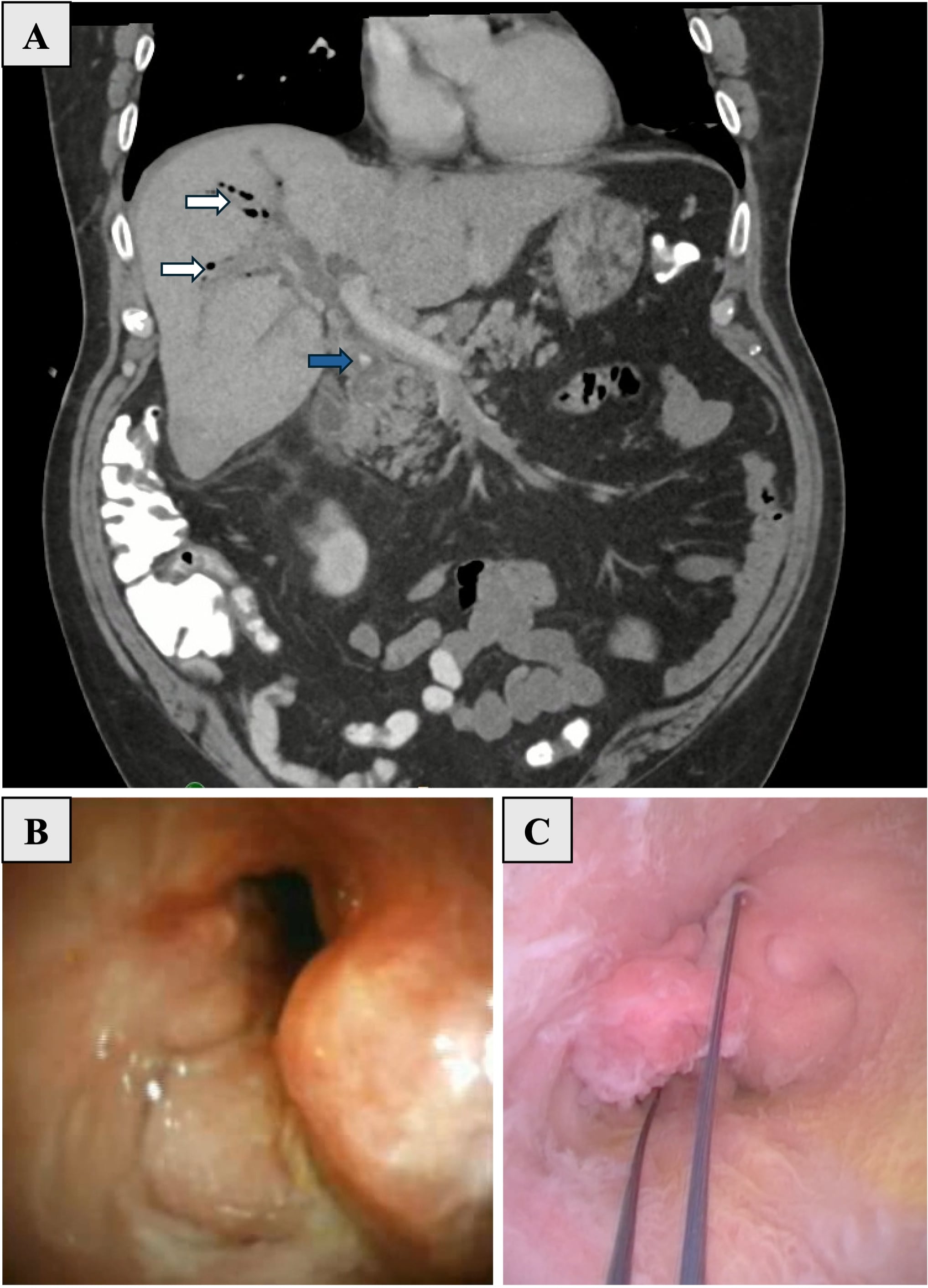
Figure: Figure 1: Coronal CT (Panel A) demonstrating choledocholithiasis (blue arrow) associated with pneumobilia (white arrows), portal vein thrombosis, and possible hepatic abscesses. Cholangioscopy (Panel B) with abnormal polypoid biliary mucosa. Snare resection of mid-CBD polypoid lesion (Panel C).
Disclosures:
Hong Lin indicated no relevant financial relationships.
Maria Krantz indicated no relevant financial relationships.
Fred Karaisz indicated no relevant financial relationships.
Fadi Hawa indicated no relevant financial relationships.
Jordan Burlen indicated no relevant financial relationships.
Hong T. Lin, MD, Maria Krantz, BS, MPH, Fred Karaisz, MD, Fadi Hawa, MD, Jordan Burlen, MD. P1447 - Snare Resection of a Polypoid Biliary Lesion via Cholangioscopy in a Patient With Cirrhotic Liver Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
