Sunday Poster Session
Category: Interventional Endoscopy
P1434 - A Rare Case of Choledocholithiasis Following Endoscopic Ultrasound-Guided Gallbladder Drainage for Acute Cholecystitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Wesley Chow, MD (he/him/his)
Scripps Mercy Hospital
San Diego, CA
Presenting Author(s)
Wesley Chow, MD1, Evan Wilder, MD2, Sushrut Thiruvengadam, MD2, Douglas Hunt, MD3
1Scripps Mercy Hospital, San Diego, CA; 2Scripps Green Hospital, La Jolla, CA; 3Scripps Clinic, La Jolla, CA
Introduction: Endoscopic ultrasound-guided gallbladder drainage (EUS-GBD) with a lumen-apposing metal stent (LAMS) has been increasingly utilized for gallbladder drainage in high-risk surgical candidates with acute cholecystitis. Well-documented complications include stent migration, bile stasis, and bleeding, but biliary obstruction has rarely been reported. Here, we present a case of acute calculous cholecystitis in a non-surgical candidate who underwent EUS-GBD with LAMS and developed biliary obstruction from choledocholithiasis on post-procedure day one.
Case Description/
Methods: An 86-year-old male with dementia, heart failure, chronic kidney disease, post-ablation atrial fibrillation and sick sinus syndrome with pacemaker presented for one day of right-sided abdominal pain, nausea and non-bilious emesis. His vitals were stable, and he had mild right upper quadrant tenderness. Labs revealed WBC 10.4K, AST 46 U/L, ALT 26 U/L, alkaline phosphatase (AP) 87 U/L, total bilirubin 1.0 mg/dL and lipase 113 U/L. CT abdomen identified a distended gallbladder, peri-cholecystic fluid, and layering sludge suggestive of acute cholecystitis. General surgery evaluated the patient, but he was deemed a poor surgical candidate therefore GI was consulted for endoscopic intervention.
He underwent EUS-GBD, creating a cholecystoduodenostomy in the second part of the duodenum, via deployment of a 10 × 10-mm LAMS and coaxially placed 7 French plastic double-pigtail stent. On post-procedure day one, he had an elevated AST 781 U/L, ALT 573 U/L, AP 173 U/L and total bilirubin 5.8 mg/dL. MRCP was limited by post-procedural pneumobilia and EUS confirmed choledocholithiasis. On endoscopy, the LAMS was widely patent. ERCP with sphincterotomy successfully removed two gallstones. He was discharged in stable condition after labs normalized.
Discussion: EUS-GBD with LAMS allows for effective gallbladder drainage and is well tolerated. While malignancy-related biliary obstruction has been reported following EUS-GBD, only one study has reported choledocholithiasis after EUS-GBD with LAMS. This is the first report of choledocholithiasis after EUS-GBD with both LAMS and a pigtail stent. Choledocholithiasis in this setting may result from dislodgement of a retained gallstone during stent placement, wire coiling in the gallbladder or saline flush into the cystic duct. Therefore, clinicians should consider post-EUS-GBD choledocholithiasis in calculous cholecystitis patients who develop post-procedural jaundice or transaminitis.
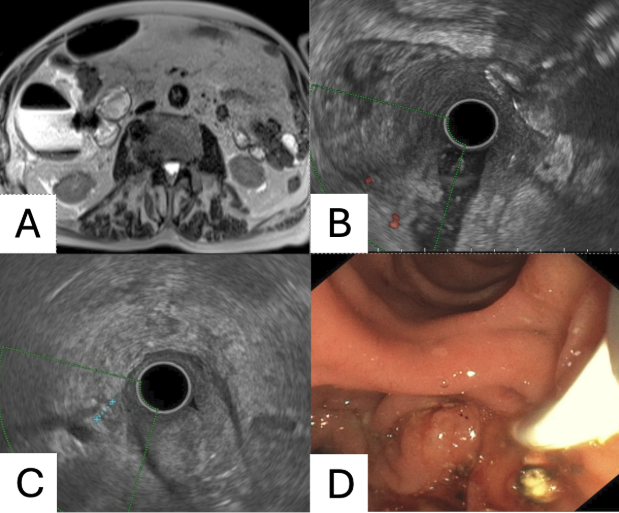
Figure: Figure 1. (A) MRCP after EUS-GBD with LAMS in appropriate position, gallbladder distention with layering sludge and pneumobilia. (B) EUS of LAMS. (C) EUS with non-shadowing hyperechoic foci air artifact and a 4 mm shadowing filling defect in the common bile duct consistent with choledocholithiasis. (D) Post-sphincterotomy with successful removal of a gallstone.
Disclosures:
Wesley Chow indicated no relevant financial relationships.
Evan Wilder indicated no relevant financial relationships.
Sushrut Thiruvengadam indicated no relevant financial relationships.
Douglas Hunt indicated no relevant financial relationships.
Wesley Chow, MD1, Evan Wilder, MD2, Sushrut Thiruvengadam, MD2, Douglas Hunt, MD3. P1434 - A Rare Case of Choledocholithiasis Following Endoscopic Ultrasound-Guided Gallbladder Drainage for Acute Cholecystitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Scripps Mercy Hospital, San Diego, CA; 2Scripps Green Hospital, La Jolla, CA; 3Scripps Clinic, La Jolla, CA
Introduction: Endoscopic ultrasound-guided gallbladder drainage (EUS-GBD) with a lumen-apposing metal stent (LAMS) has been increasingly utilized for gallbladder drainage in high-risk surgical candidates with acute cholecystitis. Well-documented complications include stent migration, bile stasis, and bleeding, but biliary obstruction has rarely been reported. Here, we present a case of acute calculous cholecystitis in a non-surgical candidate who underwent EUS-GBD with LAMS and developed biliary obstruction from choledocholithiasis on post-procedure day one.
Case Description/
Methods: An 86-year-old male with dementia, heart failure, chronic kidney disease, post-ablation atrial fibrillation and sick sinus syndrome with pacemaker presented for one day of right-sided abdominal pain, nausea and non-bilious emesis. His vitals were stable, and he had mild right upper quadrant tenderness. Labs revealed WBC 10.4K, AST 46 U/L, ALT 26 U/L, alkaline phosphatase (AP) 87 U/L, total bilirubin 1.0 mg/dL and lipase 113 U/L. CT abdomen identified a distended gallbladder, peri-cholecystic fluid, and layering sludge suggestive of acute cholecystitis. General surgery evaluated the patient, but he was deemed a poor surgical candidate therefore GI was consulted for endoscopic intervention.
He underwent EUS-GBD, creating a cholecystoduodenostomy in the second part of the duodenum, via deployment of a 10 × 10-mm LAMS and coaxially placed 7 French plastic double-pigtail stent. On post-procedure day one, he had an elevated AST 781 U/L, ALT 573 U/L, AP 173 U/L and total bilirubin 5.8 mg/dL. MRCP was limited by post-procedural pneumobilia and EUS confirmed choledocholithiasis. On endoscopy, the LAMS was widely patent. ERCP with sphincterotomy successfully removed two gallstones. He was discharged in stable condition after labs normalized.
Discussion: EUS-GBD with LAMS allows for effective gallbladder drainage and is well tolerated. While malignancy-related biliary obstruction has been reported following EUS-GBD, only one study has reported choledocholithiasis after EUS-GBD with LAMS. This is the first report of choledocholithiasis after EUS-GBD with both LAMS and a pigtail stent. Choledocholithiasis in this setting may result from dislodgement of a retained gallstone during stent placement, wire coiling in the gallbladder or saline flush into the cystic duct. Therefore, clinicians should consider post-EUS-GBD choledocholithiasis in calculous cholecystitis patients who develop post-procedural jaundice or transaminitis.
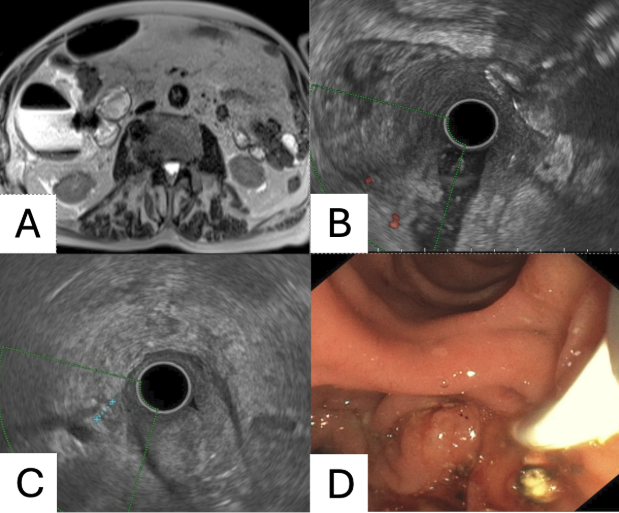
Figure: Figure 1. (A) MRCP after EUS-GBD with LAMS in appropriate position, gallbladder distention with layering sludge and pneumobilia. (B) EUS of LAMS. (C) EUS with non-shadowing hyperechoic foci air artifact and a 4 mm shadowing filling defect in the common bile duct consistent with choledocholithiasis. (D) Post-sphincterotomy with successful removal of a gallstone.
Disclosures:
Wesley Chow indicated no relevant financial relationships.
Evan Wilder indicated no relevant financial relationships.
Sushrut Thiruvengadam indicated no relevant financial relationships.
Douglas Hunt indicated no relevant financial relationships.
Wesley Chow, MD1, Evan Wilder, MD2, Sushrut Thiruvengadam, MD2, Douglas Hunt, MD3. P1434 - A Rare Case of Choledocholithiasis Following Endoscopic Ultrasound-Guided Gallbladder Drainage for Acute Cholecystitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

