Sunday Poster Session
Category: Interventional Endoscopy
P1433 - Rectal Endometriosis Uncovered by EUS-FNA: The Value of Persistent Clinical Suspicion
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Ramez M. Ibrahim, MD
SUNY Downstate Health Sciences University
Brooklyn, NY
Presenting Author(s)
Ramez M.. Ibrahim, MD1, Tarah Magloire, MD2, Alexander J. Kaye, MD1, Dalia Mahmoud Hassan Elamin, MD3, Qi Yu, MD4, Yaniuska Lescaille, MD, MPH5
1SUNY Downstate Health Sciences University, Brooklyn, NY; 2SUNY Downstate Medical Center, Brooklyn, NY; 3NYC Health + Hospitals/Woodhull, Brooklyn, NY; 4SUNY Downstate, Brooklyn, NY; 5NYC Health + Hospitals/Kings County, Brooklyn, NY
Introduction: Endometriosis is a benign gynecologic condition affecting ~10% of reproductive-age women and involves the bowel in up to 12% of cases, mainly the rectosigmoid. Symptoms like dyschezia, constipation, dyspareunia, bloating, and rectal bleeding may be nonspecific, but their association with menses should raise suspicion. We report a case of rectal endometriosis diagnosed via endoscopic ultrasound (EUS) after an inconclusive workup.
Case Description/
Methods: A 36-year-old nulligravid woman with hypertension, type 2 diabetes, and class III obesity initially presented with abdominal bloating and LUQ pain. Imaging revealed multiple large fibroids. She underwent myomectomy via midline vertical incision. One month later, she developed severe dysmenorrhea and new-onset hematochezia, described as painful, blood-tinged mucus and bloody stools occurring 1–2 days before and during menses, with complete resolution afterward. She denied constipation, prior rectal bleeding, or hemorrhoids.
She was referred to gastroenterology to rule out luminal pathology. Colonoscopy revealed internal hemorrhoids and a localized area of nodular mucosa in the rectosigmoid. Histology showed only benign hyperplastic changes. Given persistent symptoms and their menstrual association, rectal endometriosis remained on the differential. However, the referring ream was skeptical, citing absence of intraoperative findings, and negative colonoscopy biopsies. Flexible sigmoidoscopy was again non-diagnostic, and subsequent abdominal MRI was inconclusive.
Given the symptoms’ cyclical nature, EUS was pursued and revealed a 13 mm hypoechoic, subepithelial, partially circumferential lesion in the anterior rectal wall, arising from the muscularis propria and extending into the submucosa and deep mucosa. EUS-FNA confirmed rectal endometriosis, with cytology showing endometrial glands and stroma. Pelvic MRI subsequently corroborated the diagnosis.
Discussion: The most common location of intestinal endometriosis is intramural, presenting a diagnostic challenge, as first line modalities like MRI and colonoscopy/biopsy often miss deep wall lesions. In such cases, EUS/FNA is pivotal: EUS offers high-resolution visualization of bowel wall layers, enabling assessment of lesion depth and extent, while FNA enables targeted tissue sampling. In our case, colonoscopy and MRI failed to detect endometriosis, delaying diagnosis. This highlights the role of EUS and the need to maintain high clinical suspicion despite inconclusive initial investigations.
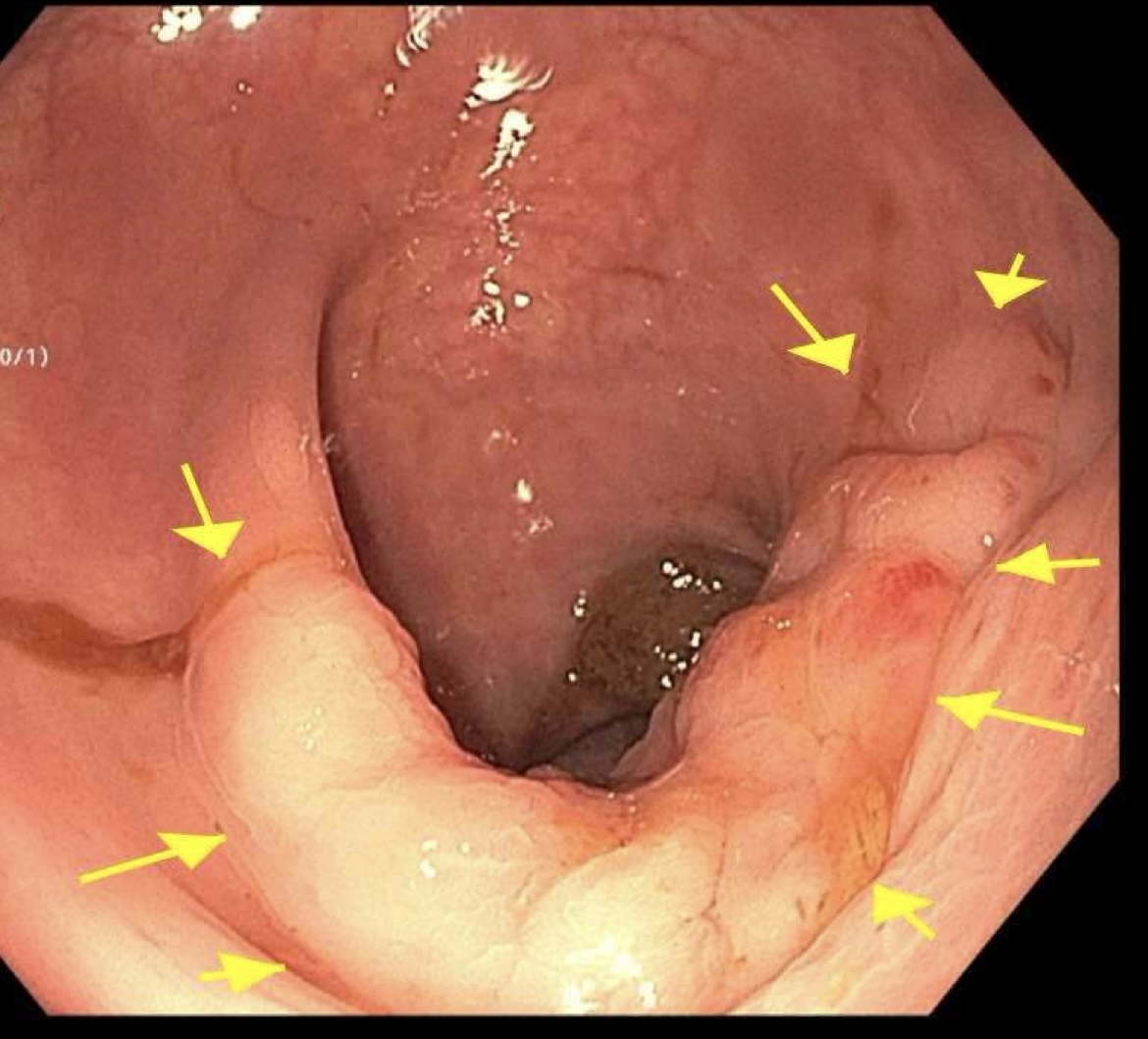
Figure: Intramural Lesion on EUS
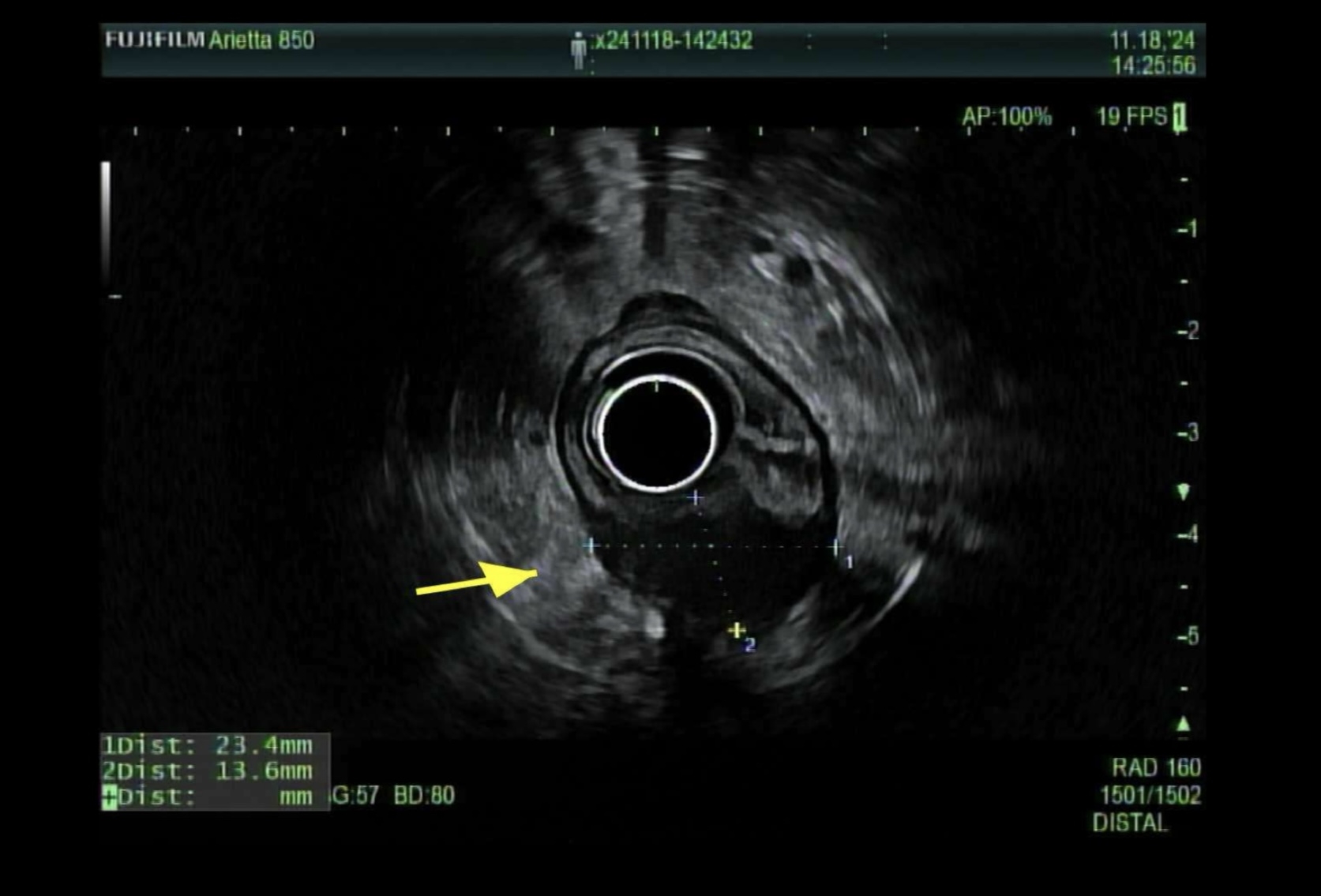
Figure: Rectosigmoid Junction: Nodular Mucosa
Disclosures:
Ramez Ibrahim indicated no relevant financial relationships.
Tarah Magloire indicated no relevant financial relationships.
Alexander Kaye indicated no relevant financial relationships.
Dalia Mahmoud Hassan Elamin indicated no relevant financial relationships.
Qi Yu indicated no relevant financial relationships.
Yaniuska Lescaille indicated no relevant financial relationships.
Ramez M.. Ibrahim, MD1, Tarah Magloire, MD2, Alexander J. Kaye, MD1, Dalia Mahmoud Hassan Elamin, MD3, Qi Yu, MD4, Yaniuska Lescaille, MD, MPH5. P1433 - Rectal Endometriosis Uncovered by EUS-FNA: The Value of Persistent Clinical Suspicion, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SUNY Downstate Health Sciences University, Brooklyn, NY; 2SUNY Downstate Medical Center, Brooklyn, NY; 3NYC Health + Hospitals/Woodhull, Brooklyn, NY; 4SUNY Downstate, Brooklyn, NY; 5NYC Health + Hospitals/Kings County, Brooklyn, NY
Introduction: Endometriosis is a benign gynecologic condition affecting ~10% of reproductive-age women and involves the bowel in up to 12% of cases, mainly the rectosigmoid. Symptoms like dyschezia, constipation, dyspareunia, bloating, and rectal bleeding may be nonspecific, but their association with menses should raise suspicion. We report a case of rectal endometriosis diagnosed via endoscopic ultrasound (EUS) after an inconclusive workup.
Case Description/
Methods: A 36-year-old nulligravid woman with hypertension, type 2 diabetes, and class III obesity initially presented with abdominal bloating and LUQ pain. Imaging revealed multiple large fibroids. She underwent myomectomy via midline vertical incision. One month later, she developed severe dysmenorrhea and new-onset hematochezia, described as painful, blood-tinged mucus and bloody stools occurring 1–2 days before and during menses, with complete resolution afterward. She denied constipation, prior rectal bleeding, or hemorrhoids.
She was referred to gastroenterology to rule out luminal pathology. Colonoscopy revealed internal hemorrhoids and a localized area of nodular mucosa in the rectosigmoid. Histology showed only benign hyperplastic changes. Given persistent symptoms and their menstrual association, rectal endometriosis remained on the differential. However, the referring ream was skeptical, citing absence of intraoperative findings, and negative colonoscopy biopsies. Flexible sigmoidoscopy was again non-diagnostic, and subsequent abdominal MRI was inconclusive.
Given the symptoms’ cyclical nature, EUS was pursued and revealed a 13 mm hypoechoic, subepithelial, partially circumferential lesion in the anterior rectal wall, arising from the muscularis propria and extending into the submucosa and deep mucosa. EUS-FNA confirmed rectal endometriosis, with cytology showing endometrial glands and stroma. Pelvic MRI subsequently corroborated the diagnosis.
Discussion: The most common location of intestinal endometriosis is intramural, presenting a diagnostic challenge, as first line modalities like MRI and colonoscopy/biopsy often miss deep wall lesions. In such cases, EUS/FNA is pivotal: EUS offers high-resolution visualization of bowel wall layers, enabling assessment of lesion depth and extent, while FNA enables targeted tissue sampling. In our case, colonoscopy and MRI failed to detect endometriosis, delaying diagnosis. This highlights the role of EUS and the need to maintain high clinical suspicion despite inconclusive initial investigations.
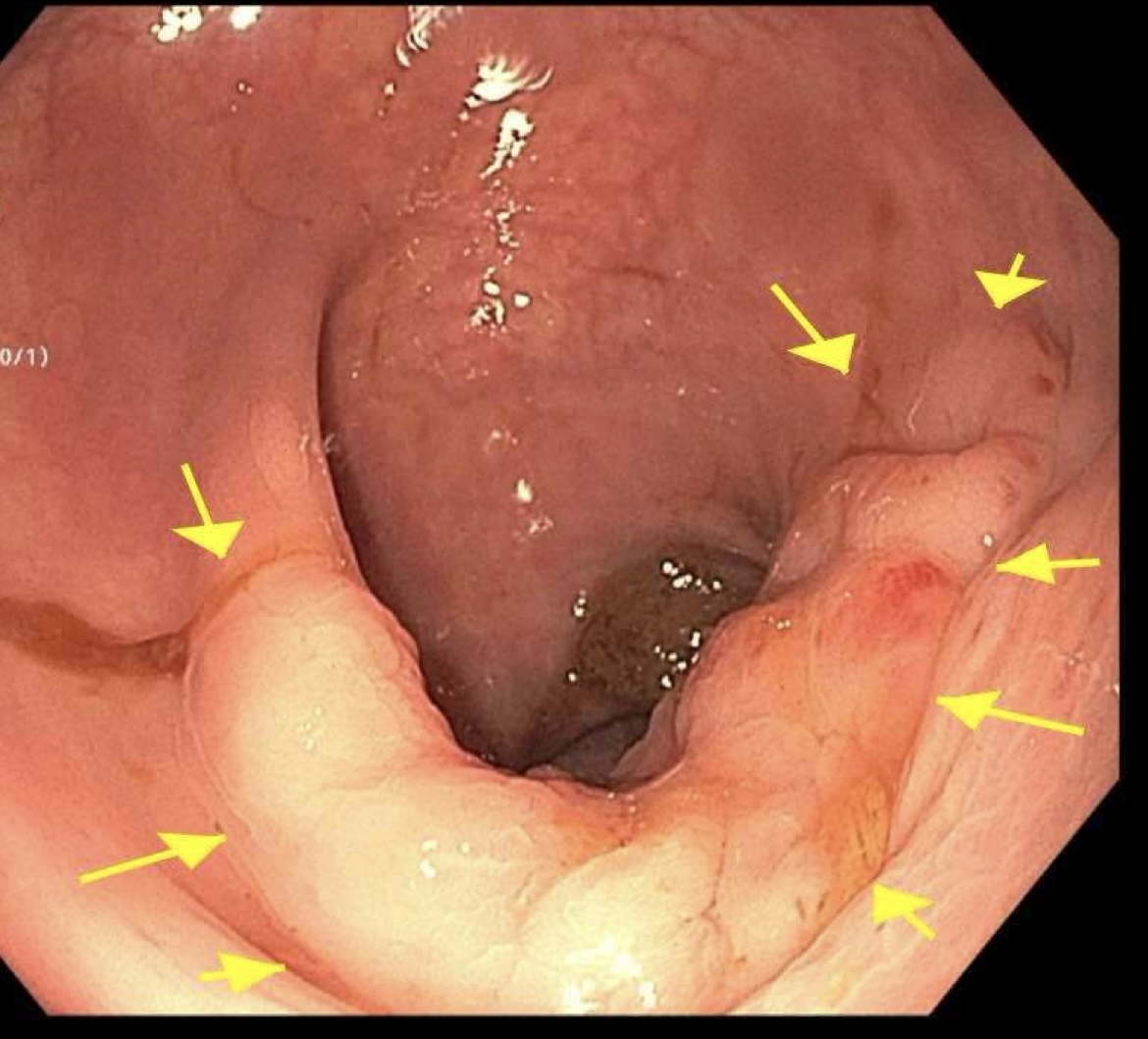
Figure: Intramural Lesion on EUS
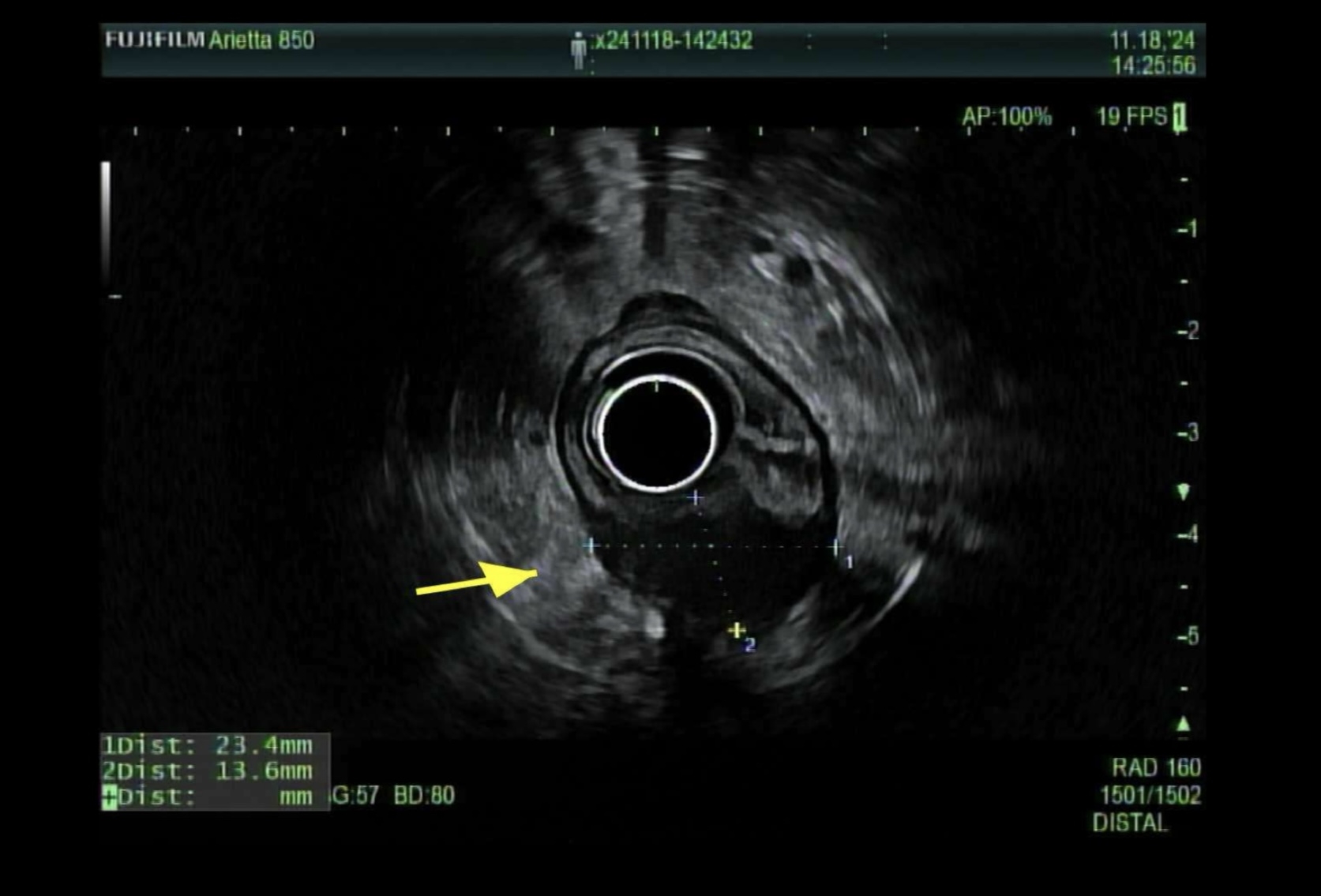
Figure: Rectosigmoid Junction: Nodular Mucosa
Disclosures:
Ramez Ibrahim indicated no relevant financial relationships.
Tarah Magloire indicated no relevant financial relationships.
Alexander Kaye indicated no relevant financial relationships.
Dalia Mahmoud Hassan Elamin indicated no relevant financial relationships.
Qi Yu indicated no relevant financial relationships.
Yaniuska Lescaille indicated no relevant financial relationships.
Ramez M.. Ibrahim, MD1, Tarah Magloire, MD2, Alexander J. Kaye, MD1, Dalia Mahmoud Hassan Elamin, MD3, Qi Yu, MD4, Yaniuska Lescaille, MD, MPH5. P1433 - Rectal Endometriosis Uncovered by EUS-FNA: The Value of Persistent Clinical Suspicion, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
