Sunday Poster Session
Category: Interventional Endoscopy
P1428 - Go with the Flow: Novel Use of Lumen-Apposing Metal Stent for Drainage of Duodenal Abscess
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Varun Jain, MD (he/him/his)
University of Pittsburgh Medical Center
Pittsburgh, PA
Presenting Author(s)
Varun Jain, MD, Thomas Gonzales, MD, Sultan Mahmood, MD
University of Pittsburgh Medical Center, Pittsburgh, PA
Introduction: Duodenal diverticula are common and usually asymptomatic, though rarely lead to abscess formation. First-line treatment includes antibiotics and percutaneous drainage for abscesses >3 cm, often with interventional radiology (IR) or, increasingly, endoscopically with endoscopic ultrasound (EUS) guidance. When abscesses persist, surgery is often required. Lumen-apposing metal stents (LAMS) have been used to drain GI abscesses, though most commonly of the pancreas or gallbladder. We present a novel case of LAMS drainage for a duodenal diverticular abscess.
Case Description/
Methods: A 75-year-old female with COPD on home oxygen, GERD on PPI, and a large hiatal hernia was admitted for a COPD exacerbation and right-sided abdominal pain. Her WBC was 13. CT revealed a 5.1 cm long mass-like lesion in the pancreaticoduodenal groove. (Figure One) Endoscopy showed multiple duodenal diverticula. EUS identified a 4.4 x 4.0 cm cystic mass in the second duodenal portion, likely a diverticular abscess. Fine needle aspiration yielded 4 mL of cloudy, yellow, thick fluid, which grew Klebsiella pneumoniae. Piperacillin/tazobactam was started. Repeat imaging five days later showed no significant change. IR and surgery were consulted but deemed the lesion difficult to access, favoring endoscopic drainage.
Repeat EUS redemonstrated the lesion without change in size. Endoscopic cystoduodenostomy was performed using LAMS. Once an appropriate position in the duodenum was identified, color Doppler imaging was used to rule out interposed vessels. Cautery was applied to access the cavity and enlarge the stoma. An 8 x 8 mm LAMS was then deployed, with both flanges positioned securely between the cyst and the duodenal wall. The stent was successfully placed, and a large amount of pus drained through the stent and was suctioned. (Figure Two) The patient’s white blood count decreased to normal levels and abdominal pain resolved.
Discussion: This case highlights the expanding role of EUS-guided LAMS drainage of duodenal abscesses. The technical and clinical success shows LAMS’ potential as a minimally invasive alternative to surgery. EUS-guided LAMS drainage offers a safe, effective approach to duodenal abscesses when percutaneous endoscopic drainage fails, and IR and surgery are not feasible. This case suggests possible expansion to LAMS' successes in draining abscesses in other parts of the GI tract. Endoscopists should consider EUS-guided LAMS as an effective and minimally invasive alternative for managing duodenal abscesses.
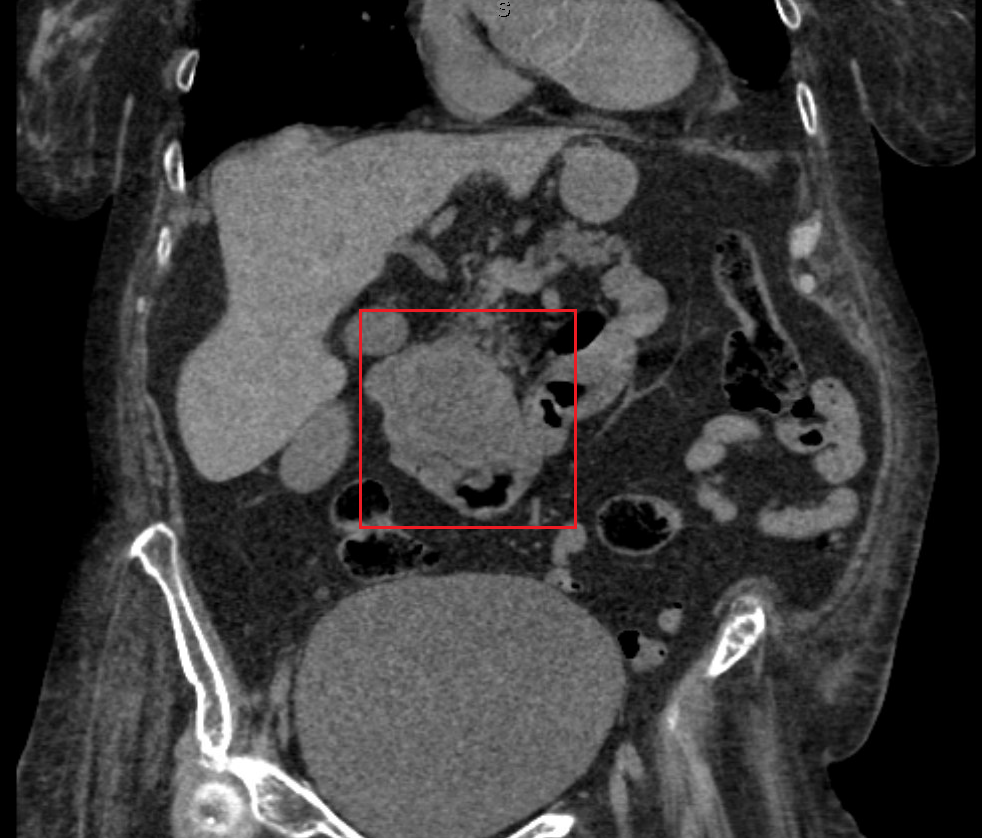
Figure: Figure One. CT abdomen with duodenal abscess by red box, measured at 5.1 cm.
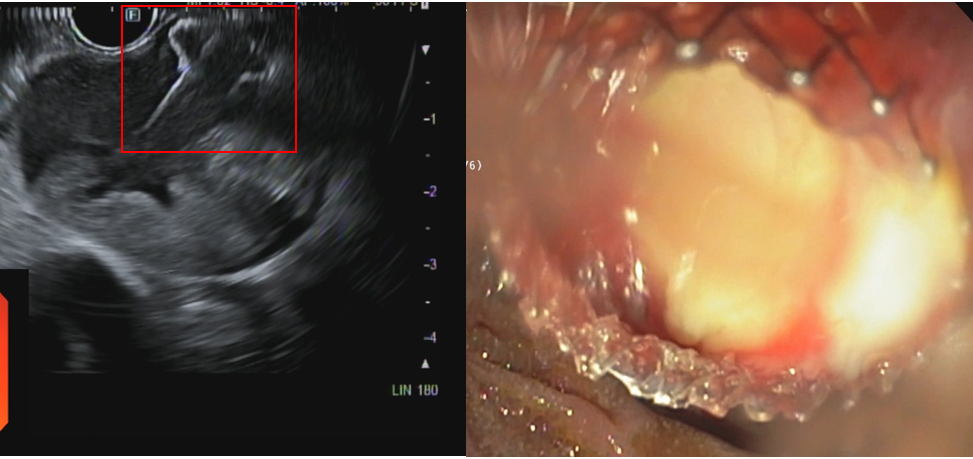
Figure: Figure Two. (left) EUS image of duodenal abscess with LAMS deployed, communicating between the abscess and the lumen. (right) Endoscopic image of LAMS from lumen side, with pus emerging from LAMS.
Disclosures:
Varun Jain indicated no relevant financial relationships.
Thomas Gonzales indicated no relevant financial relationships.
Sultan Mahmood indicated no relevant financial relationships.
Varun Jain, MD, Thomas Gonzales, MD, Sultan Mahmood, MD. P1428 - Go with the Flow: Novel Use of Lumen-Apposing Metal Stent for Drainage of Duodenal Abscess, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Pittsburgh Medical Center, Pittsburgh, PA
Introduction: Duodenal diverticula are common and usually asymptomatic, though rarely lead to abscess formation. First-line treatment includes antibiotics and percutaneous drainage for abscesses >3 cm, often with interventional radiology (IR) or, increasingly, endoscopically with endoscopic ultrasound (EUS) guidance. When abscesses persist, surgery is often required. Lumen-apposing metal stents (LAMS) have been used to drain GI abscesses, though most commonly of the pancreas or gallbladder. We present a novel case of LAMS drainage for a duodenal diverticular abscess.
Case Description/
Methods: A 75-year-old female with COPD on home oxygen, GERD on PPI, and a large hiatal hernia was admitted for a COPD exacerbation and right-sided abdominal pain. Her WBC was 13. CT revealed a 5.1 cm long mass-like lesion in the pancreaticoduodenal groove. (Figure One) Endoscopy showed multiple duodenal diverticula. EUS identified a 4.4 x 4.0 cm cystic mass in the second duodenal portion, likely a diverticular abscess. Fine needle aspiration yielded 4 mL of cloudy, yellow, thick fluid, which grew Klebsiella pneumoniae. Piperacillin/tazobactam was started. Repeat imaging five days later showed no significant change. IR and surgery were consulted but deemed the lesion difficult to access, favoring endoscopic drainage.
Repeat EUS redemonstrated the lesion without change in size. Endoscopic cystoduodenostomy was performed using LAMS. Once an appropriate position in the duodenum was identified, color Doppler imaging was used to rule out interposed vessels. Cautery was applied to access the cavity and enlarge the stoma. An 8 x 8 mm LAMS was then deployed, with both flanges positioned securely between the cyst and the duodenal wall. The stent was successfully placed, and a large amount of pus drained through the stent and was suctioned. (Figure Two) The patient’s white blood count decreased to normal levels and abdominal pain resolved.
Discussion: This case highlights the expanding role of EUS-guided LAMS drainage of duodenal abscesses. The technical and clinical success shows LAMS’ potential as a minimally invasive alternative to surgery. EUS-guided LAMS drainage offers a safe, effective approach to duodenal abscesses when percutaneous endoscopic drainage fails, and IR and surgery are not feasible. This case suggests possible expansion to LAMS' successes in draining abscesses in other parts of the GI tract. Endoscopists should consider EUS-guided LAMS as an effective and minimally invasive alternative for managing duodenal abscesses.
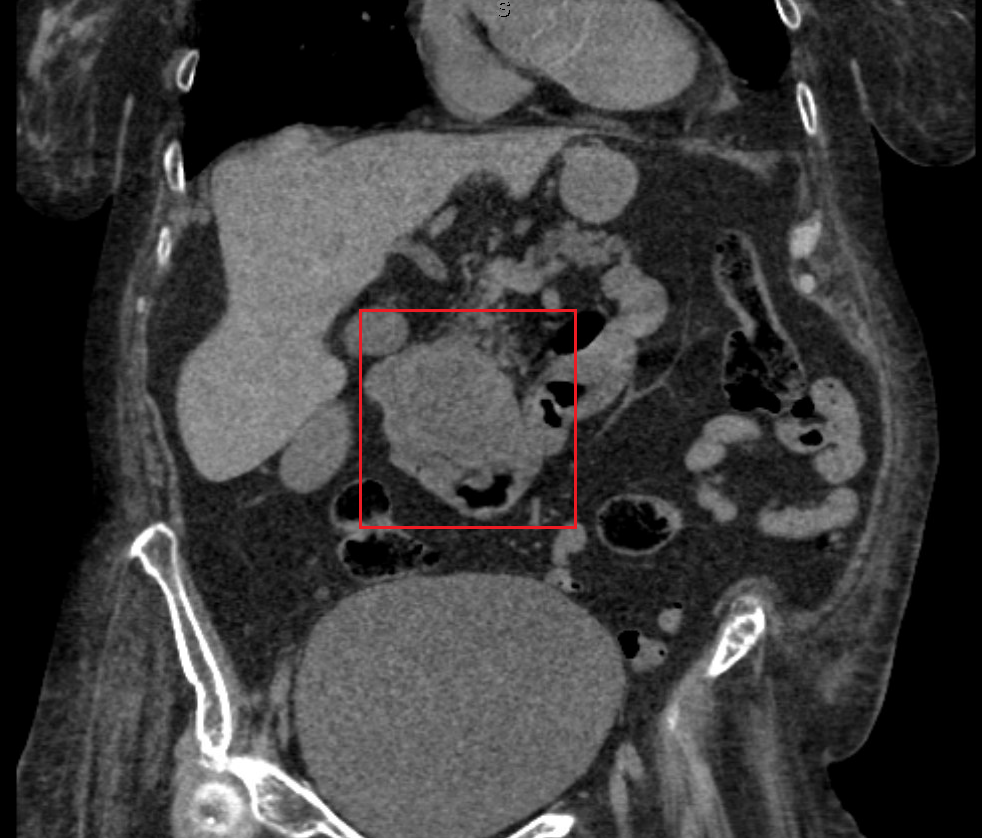
Figure: Figure One. CT abdomen with duodenal abscess by red box, measured at 5.1 cm.
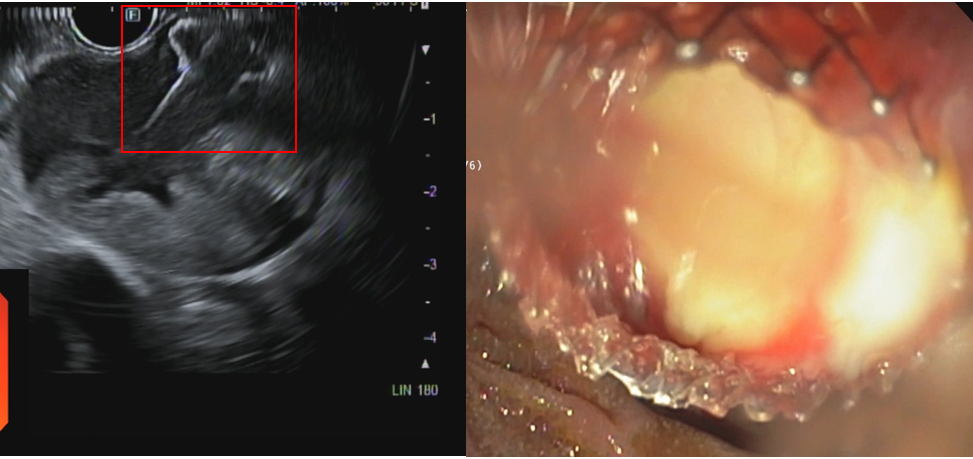
Figure: Figure Two. (left) EUS image of duodenal abscess with LAMS deployed, communicating between the abscess and the lumen. (right) Endoscopic image of LAMS from lumen side, with pus emerging from LAMS.
Disclosures:
Varun Jain indicated no relevant financial relationships.
Thomas Gonzales indicated no relevant financial relationships.
Sultan Mahmood indicated no relevant financial relationships.
Varun Jain, MD, Thomas Gonzales, MD, Sultan Mahmood, MD. P1428 - Go with the Flow: Novel Use of Lumen-Apposing Metal Stent for Drainage of Duodenal Abscess, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
