Sunday Poster Session
Category: Interventional Endoscopy
P1425 - Recurrent Ileocolonic Anastomotic Stricture Following Small Bowel Resection: Successful Palliation With EUS-Guided Axios Stent Placement
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Sunny Kumar, MD (he/him/his)
Wright Center for Graduate Medical Education
Scranton, PA
Presenting Author(s)
Sunny Kumar, MD1, Ashok Kumar, MD2, Rahul Kumar, MD3, Avinash Nankani, MBBS4, Vikash Kumar, MD5, Amla Patel, MBBS6, Hany Eskarous, MD7, Aman Ali, MD8
1Wright Center for Graduate Medical Education, Scranton, PA; 2Ascension Saint Joseph Hospital, Chicago, IL; 3North Central Bronx Hospital, Bronx, NY; 4Dow University of Health Sciences, Karachi, Sindh, Pakistan; 5Creighton University School of Medicine, Phoenix, AZ; 6Creighton University, Phoenix, Phoenix, AZ; 7The Wright Center for Graduate Medical Education, Scranton, PA; 8Wilkes-Barre General Hospital, Scranton, PA
Introduction: Ileocolonic anastomotic strictures are a common complication after bowel surgery, often caused by inflammation, ischemia, or scar formation. While endoscopic balloon dilation is typically the first-line treatment, some strictures are recurrent or refractory, posing significant management challenges. Repeat dilations may be required, though efficacy often diminishes, and risks like perforation or bleeding increase. For patients who are poor surgical candidates or have failed conventional therapy, advanced endoscopic approaches such as stent placement offer valuable alternatives. This case highlights the successful use of a lumen-apposing metal stent (LAMS) in a patient with a recurrent ileocolonic stricture, demonstrating its safety and effectiveness in complex post-surgical cases.
Case Description/
Methods: A 53-year-old woman with GERD and migraines developed recurrent bowel obstruction one year after small bowel resection with ileocecal anastomosis due to adhesions. Colonoscopy revealed a 3–4 mm non-traversable ileocolonic stricture, even with a pediatric scope. Biopsies from the terminal ileum and colon ruled out Crohn’s and other inflammatory conditions. Balloon dilation to 12 mm provided temporary relief, but placement of a fully covered self-expandable metal stent (FCSEMS) was unsuccessful due to limited scope reach.
Patient presents for symptom recurrence, a therapeutic gastroscope was used to access the stricture, measuring 3-4 mm, confirmed by enterogram. A 20 x 10 mm LAMS (Axios) was successfully placed. Fluoroscopy showed successful Axios stent placement, improving symptoms. The patient was advised to maintain soft stools and follow up with CT enterography in two months; stent removal was planned after approximately three months.
Discussion: Recurrent ileocolonic anastomotic strictures are challenging, particularly in patients with prior surgeries. Balloon dilation often offers only temporary relief, with high recurrence rates. FCSEMS placement carries risks of migration due to limited anchoring, especially in short or angulated strictures. LAMS (Axios) provides superior anchorage via bilateral flanges, reducing migration risk. Although off-label in the lower GI tract, LAMS are a promising option. In this case, LAMS placement succeeded where FCSEMS failed, offering safe, effective, and durable symptom relief. Further studies are needed to clarify their optimal role.
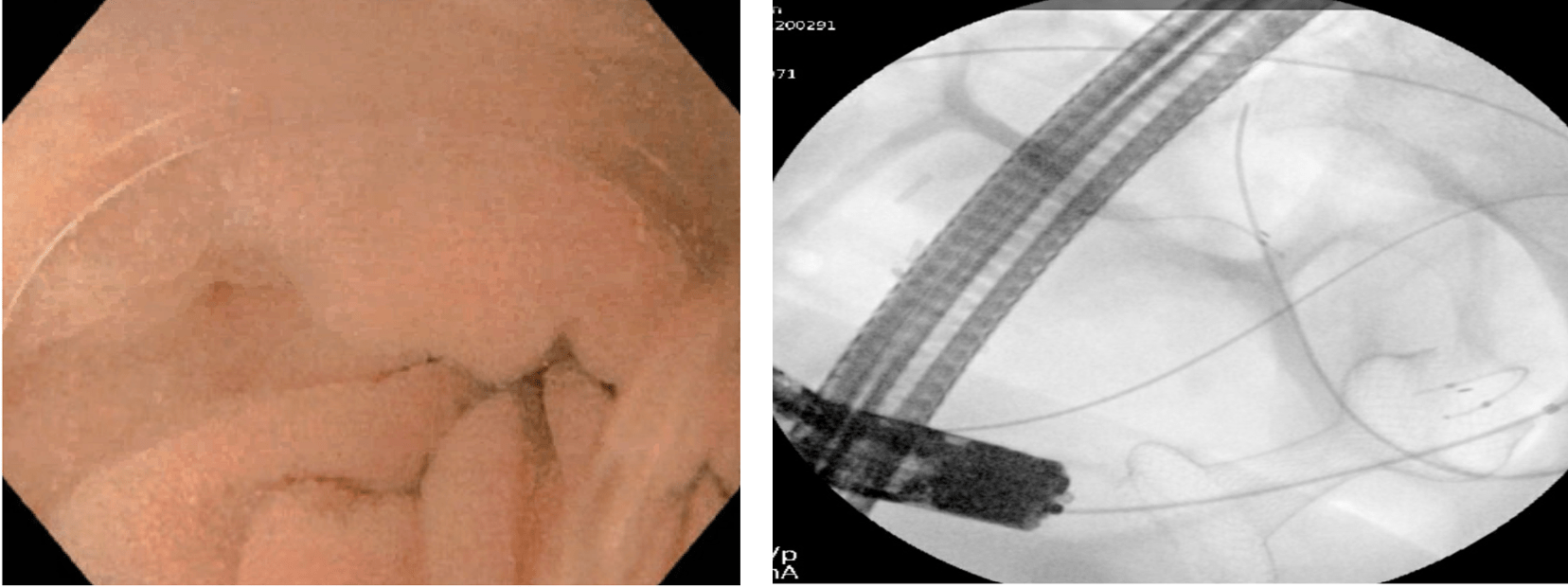
Figure: Colonoscopy revealed a tight ileocolonic anastomotic stricture that was not traversable with a pediatric scope. Balloon dilation to 12 mm.
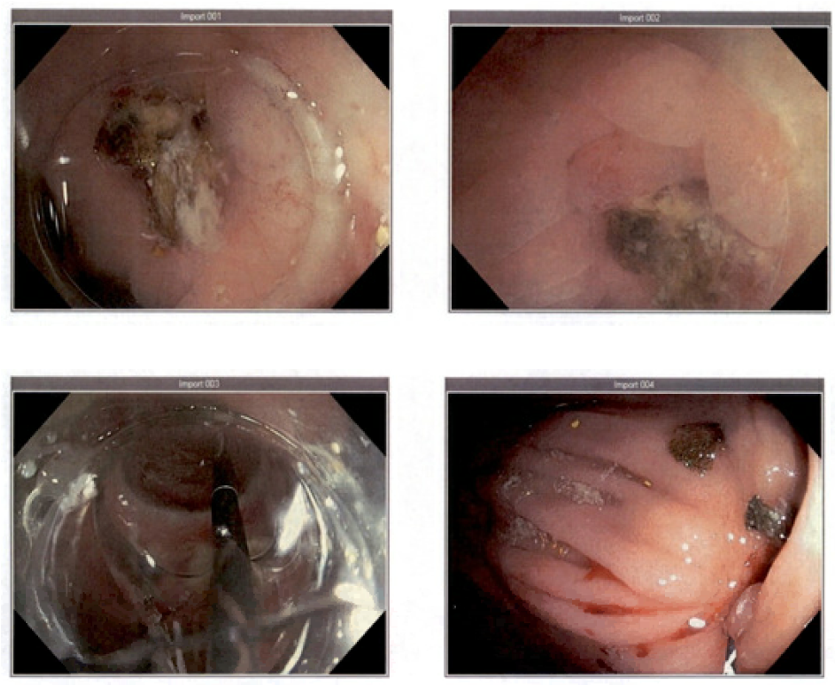
Figure: Image 1: Therapeutic gastroscope, a focal 3–4 mm ileocolonic stricture was identified.Image 2: Fluoroscopy after successful Axios stent placement.
Disclosures:
Sunny Kumar indicated no relevant financial relationships.
Ashok Kumar indicated no relevant financial relationships.
Rahul Kumar indicated no relevant financial relationships.
Avinash Nankani indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Amla Patel indicated no relevant financial relationships.
Hany Eskarous indicated no relevant financial relationships.
Aman Ali indicated no relevant financial relationships.
Sunny Kumar, MD1, Ashok Kumar, MD2, Rahul Kumar, MD3, Avinash Nankani, MBBS4, Vikash Kumar, MD5, Amla Patel, MBBS6, Hany Eskarous, MD7, Aman Ali, MD8. P1425 - Recurrent Ileocolonic Anastomotic Stricture Following Small Bowel Resection: Successful Palliation With EUS-Guided Axios Stent Placement, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Wright Center for Graduate Medical Education, Scranton, PA; 2Ascension Saint Joseph Hospital, Chicago, IL; 3North Central Bronx Hospital, Bronx, NY; 4Dow University of Health Sciences, Karachi, Sindh, Pakistan; 5Creighton University School of Medicine, Phoenix, AZ; 6Creighton University, Phoenix, Phoenix, AZ; 7The Wright Center for Graduate Medical Education, Scranton, PA; 8Wilkes-Barre General Hospital, Scranton, PA
Introduction: Ileocolonic anastomotic strictures are a common complication after bowel surgery, often caused by inflammation, ischemia, or scar formation. While endoscopic balloon dilation is typically the first-line treatment, some strictures are recurrent or refractory, posing significant management challenges. Repeat dilations may be required, though efficacy often diminishes, and risks like perforation or bleeding increase. For patients who are poor surgical candidates or have failed conventional therapy, advanced endoscopic approaches such as stent placement offer valuable alternatives. This case highlights the successful use of a lumen-apposing metal stent (LAMS) in a patient with a recurrent ileocolonic stricture, demonstrating its safety and effectiveness in complex post-surgical cases.
Case Description/
Methods: A 53-year-old woman with GERD and migraines developed recurrent bowel obstruction one year after small bowel resection with ileocecal anastomosis due to adhesions. Colonoscopy revealed a 3–4 mm non-traversable ileocolonic stricture, even with a pediatric scope. Biopsies from the terminal ileum and colon ruled out Crohn’s and other inflammatory conditions. Balloon dilation to 12 mm provided temporary relief, but placement of a fully covered self-expandable metal stent (FCSEMS) was unsuccessful due to limited scope reach.
Patient presents for symptom recurrence, a therapeutic gastroscope was used to access the stricture, measuring 3-4 mm, confirmed by enterogram. A 20 x 10 mm LAMS (Axios) was successfully placed. Fluoroscopy showed successful Axios stent placement, improving symptoms. The patient was advised to maintain soft stools and follow up with CT enterography in two months; stent removal was planned after approximately three months.
Discussion: Recurrent ileocolonic anastomotic strictures are challenging, particularly in patients with prior surgeries. Balloon dilation often offers only temporary relief, with high recurrence rates. FCSEMS placement carries risks of migration due to limited anchoring, especially in short or angulated strictures. LAMS (Axios) provides superior anchorage via bilateral flanges, reducing migration risk. Although off-label in the lower GI tract, LAMS are a promising option. In this case, LAMS placement succeeded where FCSEMS failed, offering safe, effective, and durable symptom relief. Further studies are needed to clarify their optimal role.
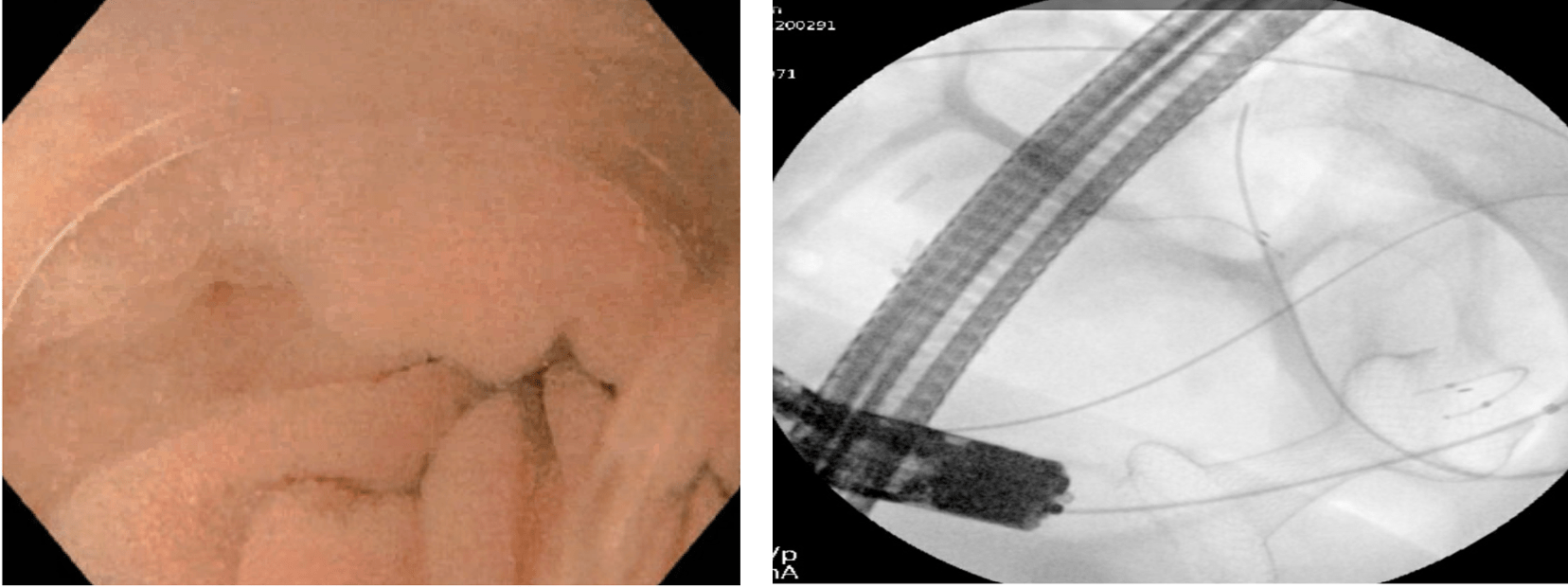
Figure: Colonoscopy revealed a tight ileocolonic anastomotic stricture that was not traversable with a pediatric scope. Balloon dilation to 12 mm.
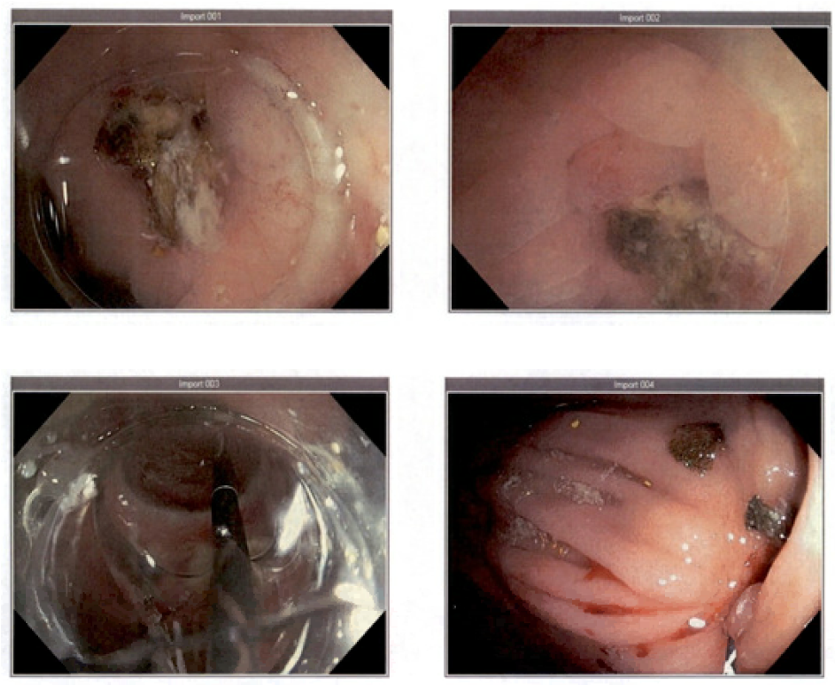
Figure: Image 1: Therapeutic gastroscope, a focal 3–4 mm ileocolonic stricture was identified.Image 2: Fluoroscopy after successful Axios stent placement.
Disclosures:
Sunny Kumar indicated no relevant financial relationships.
Ashok Kumar indicated no relevant financial relationships.
Rahul Kumar indicated no relevant financial relationships.
Avinash Nankani indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Amla Patel indicated no relevant financial relationships.
Hany Eskarous indicated no relevant financial relationships.
Aman Ali indicated no relevant financial relationships.
Sunny Kumar, MD1, Ashok Kumar, MD2, Rahul Kumar, MD3, Avinash Nankani, MBBS4, Vikash Kumar, MD5, Amla Patel, MBBS6, Hany Eskarous, MD7, Aman Ali, MD8. P1425 - Recurrent Ileocolonic Anastomotic Stricture Following Small Bowel Resection: Successful Palliation With EUS-Guided Axios Stent Placement, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
