Sunday Poster Session
Category: Interventional Endoscopy
P1423 - Palliative EUS-Guided Enterocolostomy (EUS-EC) for Management of Malignant Small Bowel Obstruction (MSBO) from Metastatic Gastric Cancer
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Brenton Davis, MD (he/him/his)
Kaiser Permanente
San Francisco, CA
Presenting Author(s)
Brenton Davis, MD1, Maen Masadeh, MD2
1Kaiser Permanente, San Francisco, CA; 2Kaiser Permanente, San Jose, CA
Introduction: Malignant small bowel obstruction (MSBO) challenges management in advanced GI malignancies. Surgery carries high morbidity, especially with peritoneal carcinomatosis. EUS-guided enterocolostomy (EUS-EC) offers minimally invasive palliation when surgery isn't feasible.
Case Description/
Methods: 55-year-old male with prediabetes presented with abdominal symptoms in 2024. Imaging showed hydronephrosis, misty small bowel, and retroperitoneal lymphadenopathy. December EGD/Colonoscopy revealed poorly differentiated gastric carcinoma with signet cells and ascending colon obstruction due to extrinsic compression. One month after starting palliative FOLFOX, he developed abdominal distension with small bowel dilation and ascites requiring TPN and nasogastric decompression concerning for MBSO. Large volume paracentesis provided temporary relief, but MSBO persisted despite additional chemotherapy cycles. February imaging showed distended small bowel (11cm) and malignant ascites with peritoneal thickening from which the patient was still symptomatic (FIGURE 1 A-C). Multidisciplinary tumor board deemed chemotherapy ineffective, and the patient was not a surgical candidate. Given ongoing symptoms, the decision was made to proceed with EUS-EC for palliation of MSBO. After a 4.8L paracentesis, an unprepped lower EUS was performed. A dilated small bowel loop was identified.
There was a small amount of intervening ascites, but a suitable window was located to perform EUS-EC. Under both sonographic and fluoroscopic guidance, the small bowel loop was accessed using a 19-gauge needle, liquid stool was aspirated then a 15 x 10mm free hand cautery enhanced lumen-apposing metal stent was used to create an enterocolostomy with immediate decompression of bowel noted endoscopically (FIGURE 2 A-D). Within 24 hours, nasogastric tube was removed and patient tolerated clear liquids. On day 3, normal bowel movements resumed, and he was advanced to pureed diet. Per pt preference he was transitioned to hospice and passed away 13 days later without recurrence of MSBO.
Discussion: This case demonstrates utility of EUS-EC for palliative MSBO management. With advancing EUS capabilities and increasing GI malignancies, more non-surgical candidates will benefit from EUS-EC when conventional stenting isn't possible. Our case highlights the importance of multidisciplinary management and pre-procedural paracentesis prior to EUS directed therapy.
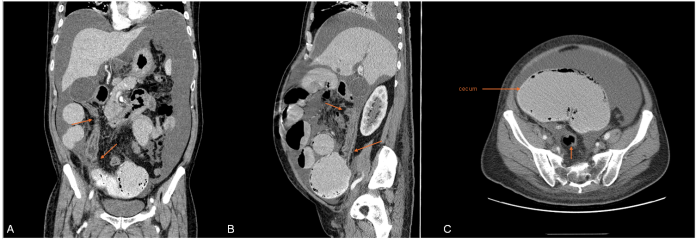
Figure: Figure 1. A) Coronal view, arrows denoting greater omental metastasis causing tethering of bowel B) Sagittal view, greater omental met tethered to gallbladder and cecum causing dilatation C) Axial view, markedly dilated cecum (11.5cm in greatest dimension) and posteriorly decompressed descending/sigmoid colon
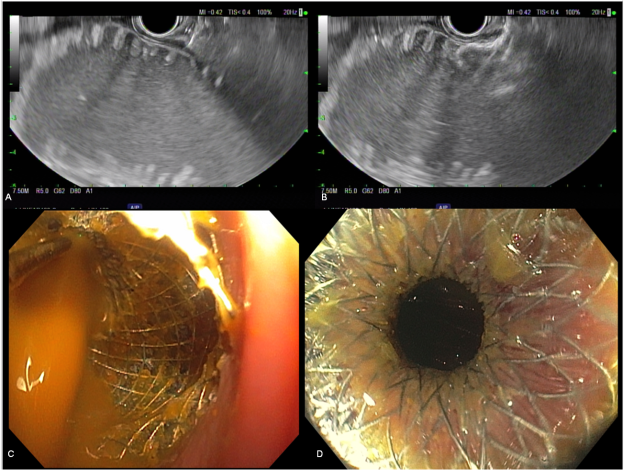
Figure: Figure 2. A) Linear EUS image of distended loop of small bowel adjacent to transverse colon B) Deployment of proximal flange within lumen of distended bowel C) endoscopic confirmation of bowel decompression D) patent enterocolostomy with slightly visible small bowel plica
Disclosures:
Brenton Davis indicated no relevant financial relationships.
Maen Masadeh indicated no relevant financial relationships.
Brenton Davis, MD1, Maen Masadeh, MD2. P1423 - Palliative EUS-Guided Enterocolostomy (EUS-EC) for Management of Malignant Small Bowel Obstruction (MSBO) from Metastatic Gastric Cancer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Kaiser Permanente, San Francisco, CA; 2Kaiser Permanente, San Jose, CA
Introduction: Malignant small bowel obstruction (MSBO) challenges management in advanced GI malignancies. Surgery carries high morbidity, especially with peritoneal carcinomatosis. EUS-guided enterocolostomy (EUS-EC) offers minimally invasive palliation when surgery isn't feasible.
Case Description/
Methods: 55-year-old male with prediabetes presented with abdominal symptoms in 2024. Imaging showed hydronephrosis, misty small bowel, and retroperitoneal lymphadenopathy. December EGD/Colonoscopy revealed poorly differentiated gastric carcinoma with signet cells and ascending colon obstruction due to extrinsic compression. One month after starting palliative FOLFOX, he developed abdominal distension with small bowel dilation and ascites requiring TPN and nasogastric decompression concerning for MBSO. Large volume paracentesis provided temporary relief, but MSBO persisted despite additional chemotherapy cycles. February imaging showed distended small bowel (11cm) and malignant ascites with peritoneal thickening from which the patient was still symptomatic (FIGURE 1 A-C). Multidisciplinary tumor board deemed chemotherapy ineffective, and the patient was not a surgical candidate. Given ongoing symptoms, the decision was made to proceed with EUS-EC for palliation of MSBO. After a 4.8L paracentesis, an unprepped lower EUS was performed. A dilated small bowel loop was identified.
There was a small amount of intervening ascites, but a suitable window was located to perform EUS-EC. Under both sonographic and fluoroscopic guidance, the small bowel loop was accessed using a 19-gauge needle, liquid stool was aspirated then a 15 x 10mm free hand cautery enhanced lumen-apposing metal stent was used to create an enterocolostomy with immediate decompression of bowel noted endoscopically (FIGURE 2 A-D). Within 24 hours, nasogastric tube was removed and patient tolerated clear liquids. On day 3, normal bowel movements resumed, and he was advanced to pureed diet. Per pt preference he was transitioned to hospice and passed away 13 days later without recurrence of MSBO.
Discussion: This case demonstrates utility of EUS-EC for palliative MSBO management. With advancing EUS capabilities and increasing GI malignancies, more non-surgical candidates will benefit from EUS-EC when conventional stenting isn't possible. Our case highlights the importance of multidisciplinary management and pre-procedural paracentesis prior to EUS directed therapy.
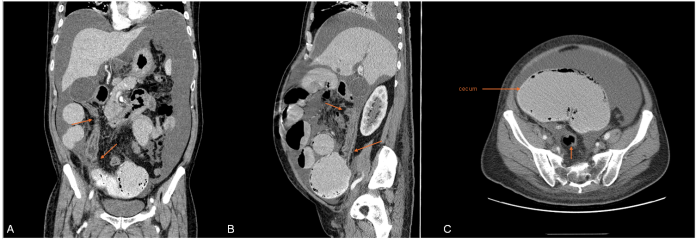
Figure: Figure 1. A) Coronal view, arrows denoting greater omental metastasis causing tethering of bowel B) Sagittal view, greater omental met tethered to gallbladder and cecum causing dilatation C) Axial view, markedly dilated cecum (11.5cm in greatest dimension) and posteriorly decompressed descending/sigmoid colon
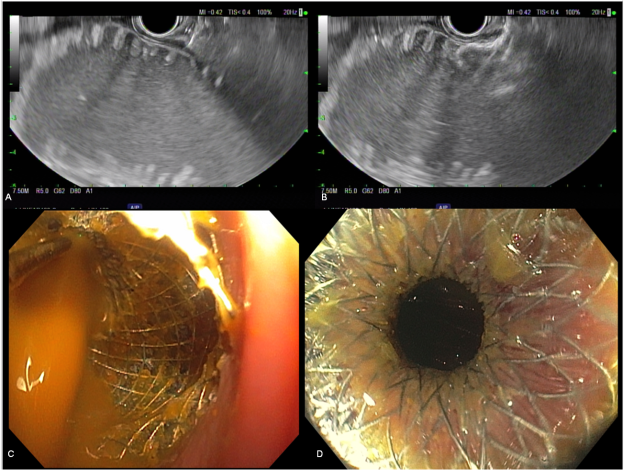
Figure: Figure 2. A) Linear EUS image of distended loop of small bowel adjacent to transverse colon B) Deployment of proximal flange within lumen of distended bowel C) endoscopic confirmation of bowel decompression D) patent enterocolostomy with slightly visible small bowel plica
Disclosures:
Brenton Davis indicated no relevant financial relationships.
Maen Masadeh indicated no relevant financial relationships.
Brenton Davis, MD1, Maen Masadeh, MD2. P1423 - Palliative EUS-Guided Enterocolostomy (EUS-EC) for Management of Malignant Small Bowel Obstruction (MSBO) from Metastatic Gastric Cancer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
