Sunday Poster Session
Category: Interventional Endoscopy
P1418 - Endoscopic Negative Intracavitary Pressure (Endo-Nip): A Simplified Management Approach for Resistant Leaks or Fistulas
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Preeyati Chopra, MBBS (she/her/hers)
Mayo Clinic
Hartford, CT
Presenting Author(s)
Preeyati Chopra, MBBS1, Mayank Goyal, MBBS1, Ashwariya Ohri, MBBS2, Moksha Manglani, 1, Shiva Goyal, 1, Navtej Buttar, MD1
1Mayo Clinic, Rochester, MN; 2Mayo Clinic, Indianapolis, IN
Introduction: Gastrointestinal (GI) leaks and fistulae, lead to considerable morbidity and mortality. Mostly because of post-surgical complications, success of leaks with conservative/ radiological intervention is highly variable from 16-46%. Advances in endoscopy have shifted the management of GI wall defects from surgery to minimally invasive approaches.
We describe Endoscopic Negative Intracavitary Pressure (EndoNIP), an endoscopic technique of luminal drain placement via the GI wall defect to create negative intracavitary pressure to manage cases where conventional management failed or was not feasible (figure 1A,1B,1C,1D).
Methods: We analyzed a database of patients who underwent EndoNIP. The following data was collected: demographic details, defect location, drain placement technique and procedure outcomes. Favorable response was: (a) complete endoscopic response (CER) (b) endoscopic bridge to surgery (EBS) (c) endoscopic maintenance with stents (EMS).
Results: A total of 85 patients (mean age, 56.7 years; 60% male) underwent EndoNIP and had GI defect for a mean of 137 days prior to EndoNIP. Majority (64.7%, 55/85) of patients had fistula and the defects were in the thoracic region (36.5%, 31/85). Nearly half of the patients (44/85, 51.8%) had trans-prosthetic (PEG/PEJ) and in others EndoNIP drain placement was via natural orifices. The most common drain size used was 12 Fr (35.3%, 30/85).
Favorable response was seen in 84.7% (72/85) patients. Of patients with favorable response, CER was noted in 76.4% with resolution of symptoms at a mean of 169.5 days. EBS led to a complete response in 16.6%. EMS was required in 6.9% patients (Table 1). Of the 13 patients with unfavorable response, 8 were EndoNIP dependent and 5 had persistent symptoms. CER was significantly more common in patients undergoing EndoNIP as the primary intervention compared to when it was the secondary intervention (24/29 vs 32/56 patients, p =0.018) as well as for supradiaphragmatic vs infradiaphragmatic lesions (p=0.006).
Discussion: Endo-NIP is a novel, promising alternative to conventional management of challenging and resistant leaks or fistulas. It is a simplified approach that unlike Endoscopic Vacuum Therapy doesn’t require frequent exchanges/procedures and could be delivered via PEG/PEJ. It provides a definitive management strategy in most patients with previously failed procedures and in others allow nutritional optimization, control of inflammation as a bridge to surgery.
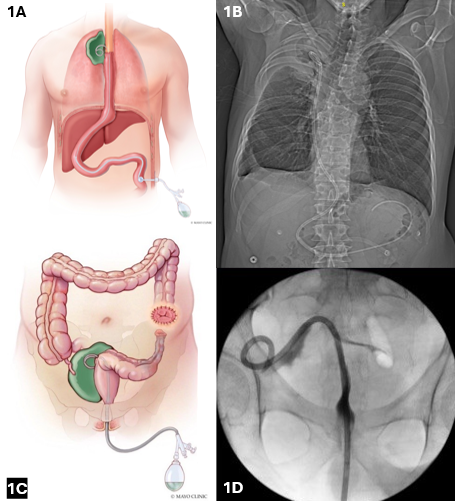
Figure: 1A: Illustration showing placement of retrograde luminal drain via PEJ tube for mediastinal GI wall defect, connected to suction for EndoNIP
1B: X-Ray: Trans-prosthetic placement of retrograde luminal drain in a mediastinal GI wall defect
1C: Illustration showing placement of trans-anal luminal drain for pelvic abscess cavity, connected to suction for EndoNIP
1D: Fluoroscopy: Trans-anal locking loop drain placement in the cavity over the guidewire
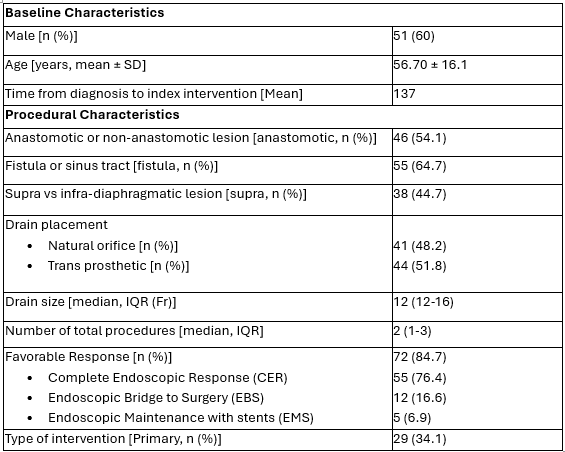
Figure: Table 1: Baseline and Procedural Characteristics
Disclosures:
Preeyati Chopra indicated no relevant financial relationships.
Mayank Goyal indicated no relevant financial relationships.
Ashwariya Ohri indicated no relevant financial relationships.
Moksha Manglani indicated no relevant financial relationships.
Shiva Goyal indicated no relevant financial relationships.
Navtej Buttar indicated no relevant financial relationships.
Preeyati Chopra, MBBS1, Mayank Goyal, MBBS1, Ashwariya Ohri, MBBS2, Moksha Manglani, 1, Shiva Goyal, 1, Navtej Buttar, MD1. P1418 - Endoscopic Negative Intracavitary Pressure (Endo-Nip): A Simplified Management Approach for Resistant Leaks or Fistulas, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mayo Clinic, Rochester, MN; 2Mayo Clinic, Indianapolis, IN
Introduction: Gastrointestinal (GI) leaks and fistulae, lead to considerable morbidity and mortality. Mostly because of post-surgical complications, success of leaks with conservative/ radiological intervention is highly variable from 16-46%. Advances in endoscopy have shifted the management of GI wall defects from surgery to minimally invasive approaches.
We describe Endoscopic Negative Intracavitary Pressure (EndoNIP), an endoscopic technique of luminal drain placement via the GI wall defect to create negative intracavitary pressure to manage cases where conventional management failed or was not feasible (figure 1A,1B,1C,1D).
Methods: We analyzed a database of patients who underwent EndoNIP. The following data was collected: demographic details, defect location, drain placement technique and procedure outcomes. Favorable response was: (a) complete endoscopic response (CER) (b) endoscopic bridge to surgery (EBS) (c) endoscopic maintenance with stents (EMS).
Results: A total of 85 patients (mean age, 56.7 years; 60% male) underwent EndoNIP and had GI defect for a mean of 137 days prior to EndoNIP. Majority (64.7%, 55/85) of patients had fistula and the defects were in the thoracic region (36.5%, 31/85). Nearly half of the patients (44/85, 51.8%) had trans-prosthetic (PEG/PEJ) and in others EndoNIP drain placement was via natural orifices. The most common drain size used was 12 Fr (35.3%, 30/85).
Favorable response was seen in 84.7% (72/85) patients. Of patients with favorable response, CER was noted in 76.4% with resolution of symptoms at a mean of 169.5 days. EBS led to a complete response in 16.6%. EMS was required in 6.9% patients (Table 1). Of the 13 patients with unfavorable response, 8 were EndoNIP dependent and 5 had persistent symptoms. CER was significantly more common in patients undergoing EndoNIP as the primary intervention compared to when it was the secondary intervention (24/29 vs 32/56 patients, p =0.018) as well as for supradiaphragmatic vs infradiaphragmatic lesions (p=0.006).
Discussion: Endo-NIP is a novel, promising alternative to conventional management of challenging and resistant leaks or fistulas. It is a simplified approach that unlike Endoscopic Vacuum Therapy doesn’t require frequent exchanges/procedures and could be delivered via PEG/PEJ. It provides a definitive management strategy in most patients with previously failed procedures and in others allow nutritional optimization, control of inflammation as a bridge to surgery.
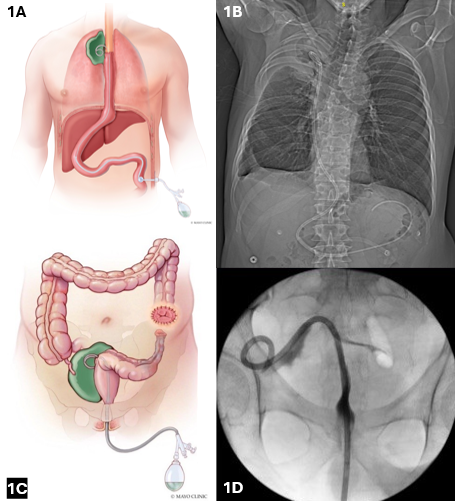
Figure: 1A: Illustration showing placement of retrograde luminal drain via PEJ tube for mediastinal GI wall defect, connected to suction for EndoNIP
1B: X-Ray: Trans-prosthetic placement of retrograde luminal drain in a mediastinal GI wall defect
1C: Illustration showing placement of trans-anal luminal drain for pelvic abscess cavity, connected to suction for EndoNIP
1D: Fluoroscopy: Trans-anal locking loop drain placement in the cavity over the guidewire
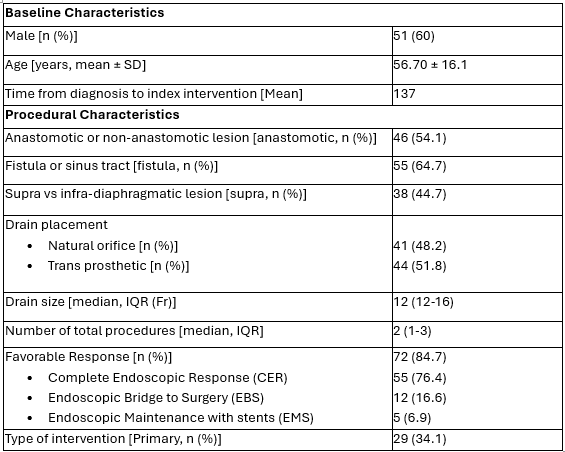
Figure: Table 1: Baseline and Procedural Characteristics
Disclosures:
Preeyati Chopra indicated no relevant financial relationships.
Mayank Goyal indicated no relevant financial relationships.
Ashwariya Ohri indicated no relevant financial relationships.
Moksha Manglani indicated no relevant financial relationships.
Shiva Goyal indicated no relevant financial relationships.
Navtej Buttar indicated no relevant financial relationships.
Preeyati Chopra, MBBS1, Mayank Goyal, MBBS1, Ashwariya Ohri, MBBS2, Moksha Manglani, 1, Shiva Goyal, 1, Navtej Buttar, MD1. P1418 - Endoscopic Negative Intracavitary Pressure (Endo-Nip): A Simplified Management Approach for Resistant Leaks or Fistulas, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
