Sunday Poster Session
Category: Interventional Endoscopy
P1402 - How Many Dilations Are Too Many? A Meta-Analysis of Endoscopic Balloon Dilation Outcomes and Surgical Conversion in Gastric Sleeve Stenosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Harsimran Kalsi, MD (she/her/hers)
University of Central Florida
Gainesville, FL
Presenting Author(s)
Harsimran Kalsi, MD1, Nihal I. Khan, MD2, Sanjeevani Tomar, MD3, Hassam Ali, MD4, Rahul Karna, MD5, Kobina Essilfie-Quaye, MD6, Yeshika Thapa, MD1, Yaseen Perbtani, DO6, Tony Brar, MD1, Babu Mohan, MD7, Rabindra Watson, MD8, Rashmi Advani, MD9
1University of Central Florida, Gainesville, FL; 2AdventHealth Orlando, Orlando, FL; 3AdventHealth, Orlando, FL; 4East Carolina University/Brody School of Medicine, Greenville, NC; 5University of Minnesota Medical Center, Minneapolis, MN; 6University of Central Florida, HCA Healthcare GME, Gainesville, FL; 7Orlando Gastroenterology, PA, Orlando, FL; 8Cedars-Sinai Medical Center, Santa Monica, CA; 9Mount Sinai South Nassau,Icahn School of Medicine at Mount Sinai, Oceanside, NY
Introduction: Gastric sleeve stenosis (GSS) is a recognized complication following laparoscopic sleeve gastrectomy (LSG), often resulting in nausea, vomiting, and oral intolerance. Endoscopic balloon dilation (EBD) is the first-line therapeutic option, yet the number of sessions required for symptom resolution and the threshold for considering surgical conversion remain unclear. We performed a systematic review and meta-analysis that evaluates the efficacy of EBD, and the rates of escalation to stenting or Roux-en-Y gastric bypass (RYGB).
Methods: We performed a systematic review of PubMed, Ovid, Cochrane and Google Scholar to identify studies reporting EBD in adult patients with GSS post-LSG. Primary outcomes were clinical success, mean number of dilations, recurrence, and need for further interventions such as endoscopic stenting or RYGB. Pooled outcomes were calculated using a random-effects model. Heterogeneity was assessed using the I² statistic.
Results: Twenty-six studies comprising 948 patients (83.5% females) were included. The pooled clinical success rate of EBD was 81.6% (95% CI: 72.93–88.92), with a mean of 1.78 dilation sessions (95% CI: 1.63–1.92) required for resolution. (Figure-1) Despite initial success, recurrence/restenosis occurred in 21.97%. 17.52% required reintervention with a different modality which included stent placement (8.93%; success rate: 67.08%) or RYGB (10.79%, success rate: 100%). Adverse events were rare at a pooled rate of 5.6%, including perforation (0.53%) and life-threatening bleeding (0.24%).
Discussion: Most patients with GSS respond to one or two EBD sessions, with diminishing returns from additional dilations. Recurrence and reintervention remain common, suggesting that persistent symptoms beyond two dilation attempts may warrant early consideration of stenting or surgical conversion. These findings offer a practical framework for when to escalate therapy in the management of post-LSG sleeve stenosis.
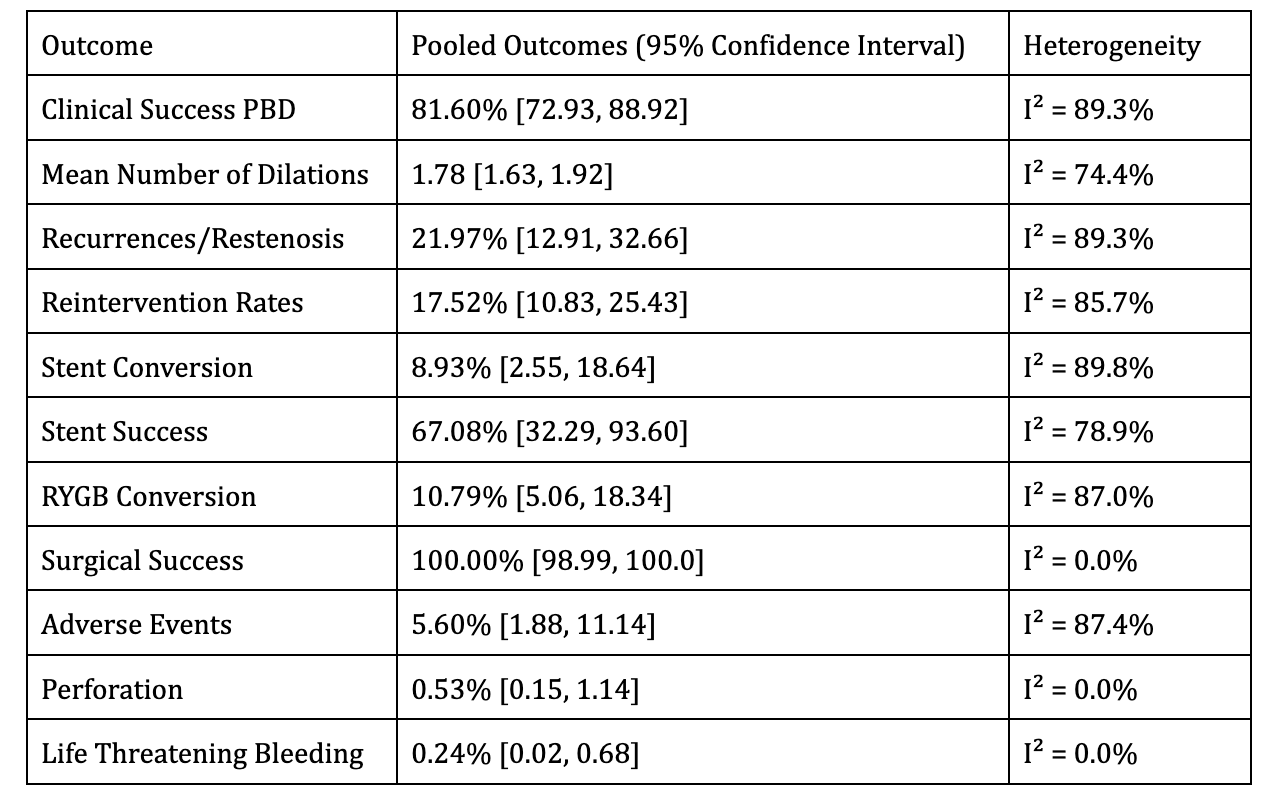
Figure: Table 1: Pooled clinical outcomes of endoscopic balloon dilation for gastric sleeve stenosis
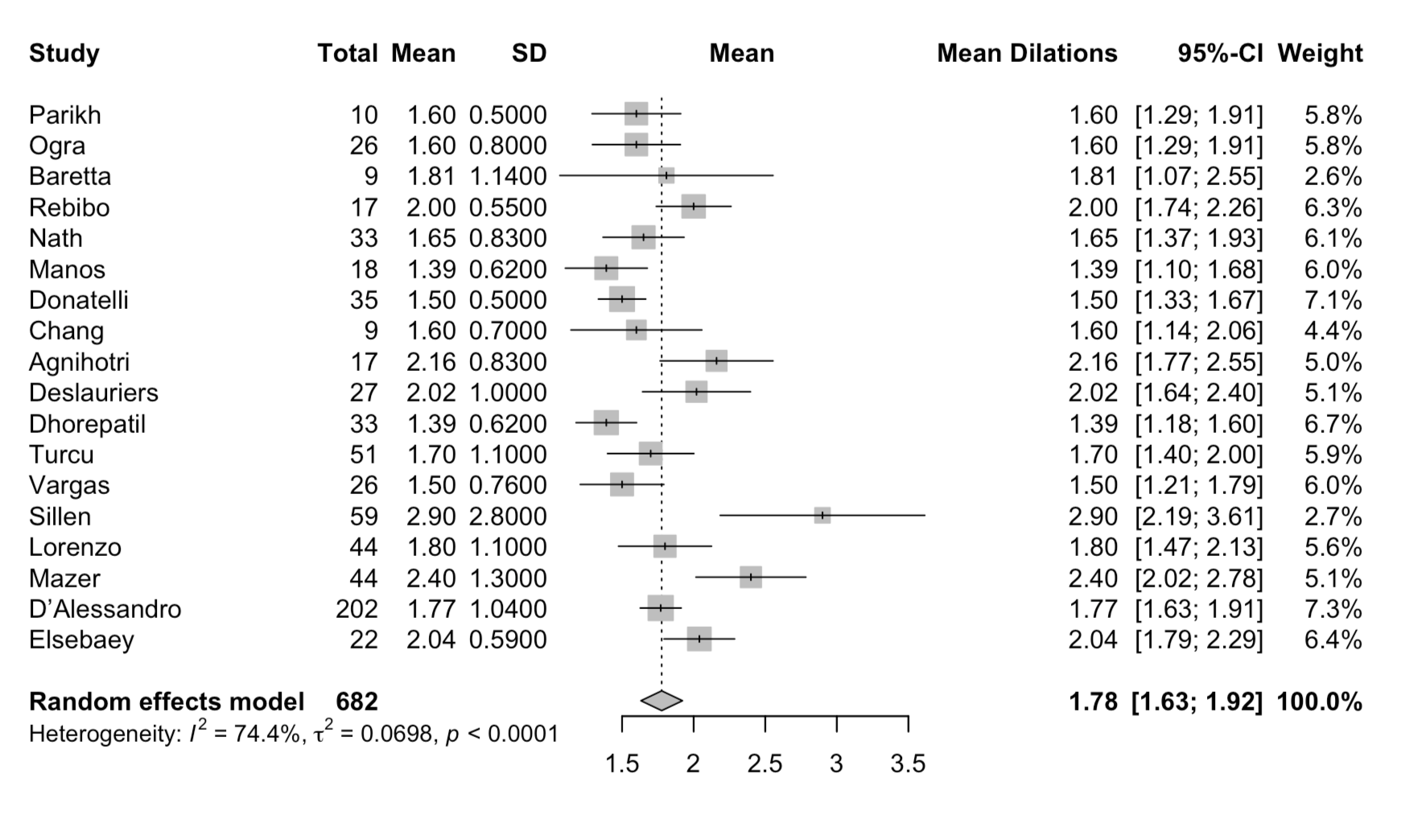
Figure: Figure 1: Forest Plot of Mean Number of Balloon Dilations for Gastric Sleeve Stenosis
Disclosures:
Harsimran Kalsi indicated no relevant financial relationships.
Nihal Khan indicated no relevant financial relationships.
Sanjeevani Tomar indicated no relevant financial relationships.
Hassam Ali indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Kobina Essilfie-Quaye indicated no relevant financial relationships.
Yeshika Thapa indicated no relevant financial relationships.
Yaseen Perbtani indicated no relevant financial relationships.
Tony Brar indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Rabindra Watson indicated no relevant financial relationships.
Rashmi Advani indicated no relevant financial relationships.
Harsimran Kalsi, MD1, Nihal I. Khan, MD2, Sanjeevani Tomar, MD3, Hassam Ali, MD4, Rahul Karna, MD5, Kobina Essilfie-Quaye, MD6, Yeshika Thapa, MD1, Yaseen Perbtani, DO6, Tony Brar, MD1, Babu Mohan, MD7, Rabindra Watson, MD8, Rashmi Advani, MD9. P1402 - How Many Dilations Are Too Many? A Meta-Analysis of Endoscopic Balloon Dilation Outcomes and Surgical Conversion in Gastric Sleeve Stenosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Central Florida, Gainesville, FL; 2AdventHealth Orlando, Orlando, FL; 3AdventHealth, Orlando, FL; 4East Carolina University/Brody School of Medicine, Greenville, NC; 5University of Minnesota Medical Center, Minneapolis, MN; 6University of Central Florida, HCA Healthcare GME, Gainesville, FL; 7Orlando Gastroenterology, PA, Orlando, FL; 8Cedars-Sinai Medical Center, Santa Monica, CA; 9Mount Sinai South Nassau,Icahn School of Medicine at Mount Sinai, Oceanside, NY
Introduction: Gastric sleeve stenosis (GSS) is a recognized complication following laparoscopic sleeve gastrectomy (LSG), often resulting in nausea, vomiting, and oral intolerance. Endoscopic balloon dilation (EBD) is the first-line therapeutic option, yet the number of sessions required for symptom resolution and the threshold for considering surgical conversion remain unclear. We performed a systematic review and meta-analysis that evaluates the efficacy of EBD, and the rates of escalation to stenting or Roux-en-Y gastric bypass (RYGB).
Methods: We performed a systematic review of PubMed, Ovid, Cochrane and Google Scholar to identify studies reporting EBD in adult patients with GSS post-LSG. Primary outcomes were clinical success, mean number of dilations, recurrence, and need for further interventions such as endoscopic stenting or RYGB. Pooled outcomes were calculated using a random-effects model. Heterogeneity was assessed using the I² statistic.
Results: Twenty-six studies comprising 948 patients (83.5% females) were included. The pooled clinical success rate of EBD was 81.6% (95% CI: 72.93–88.92), with a mean of 1.78 dilation sessions (95% CI: 1.63–1.92) required for resolution. (Figure-1) Despite initial success, recurrence/restenosis occurred in 21.97%. 17.52% required reintervention with a different modality which included stent placement (8.93%; success rate: 67.08%) or RYGB (10.79%, success rate: 100%). Adverse events were rare at a pooled rate of 5.6%, including perforation (0.53%) and life-threatening bleeding (0.24%).
Discussion: Most patients with GSS respond to one or two EBD sessions, with diminishing returns from additional dilations. Recurrence and reintervention remain common, suggesting that persistent symptoms beyond two dilation attempts may warrant early consideration of stenting or surgical conversion. These findings offer a practical framework for when to escalate therapy in the management of post-LSG sleeve stenosis.
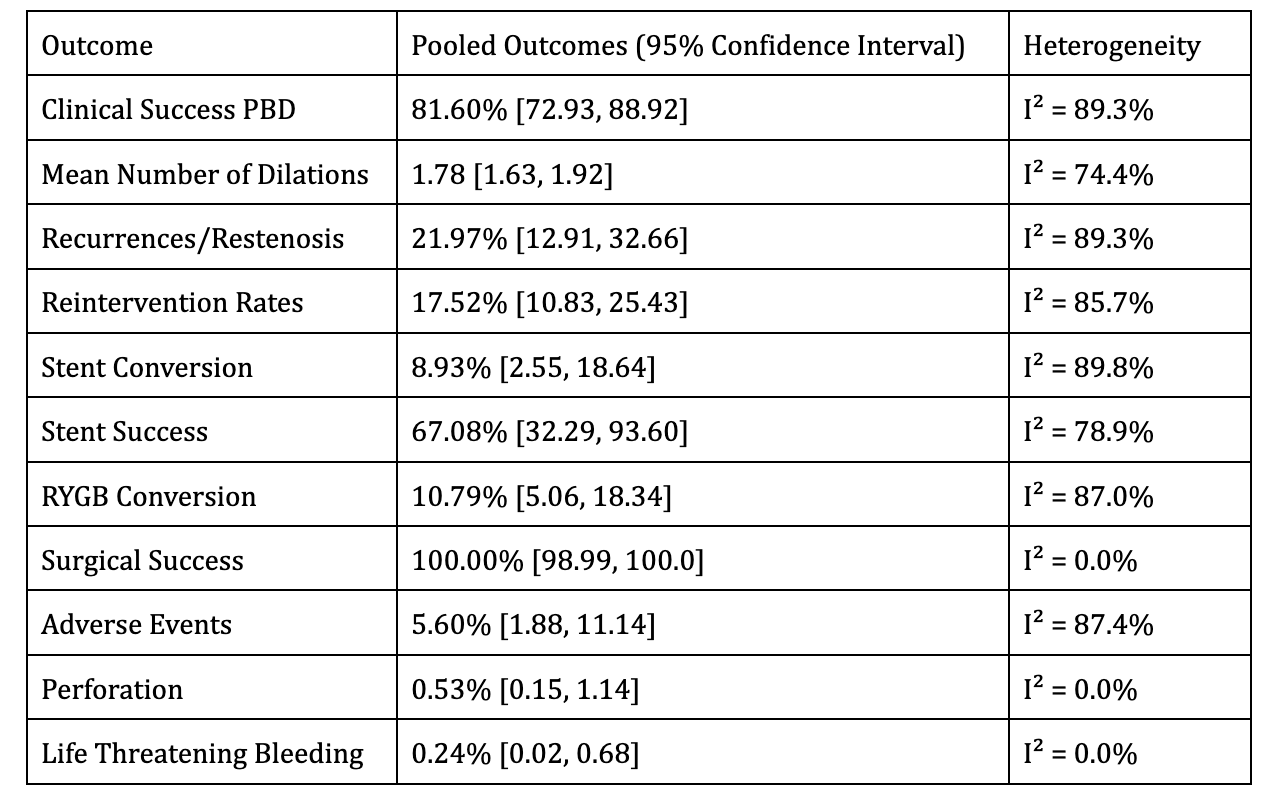
Figure: Table 1: Pooled clinical outcomes of endoscopic balloon dilation for gastric sleeve stenosis
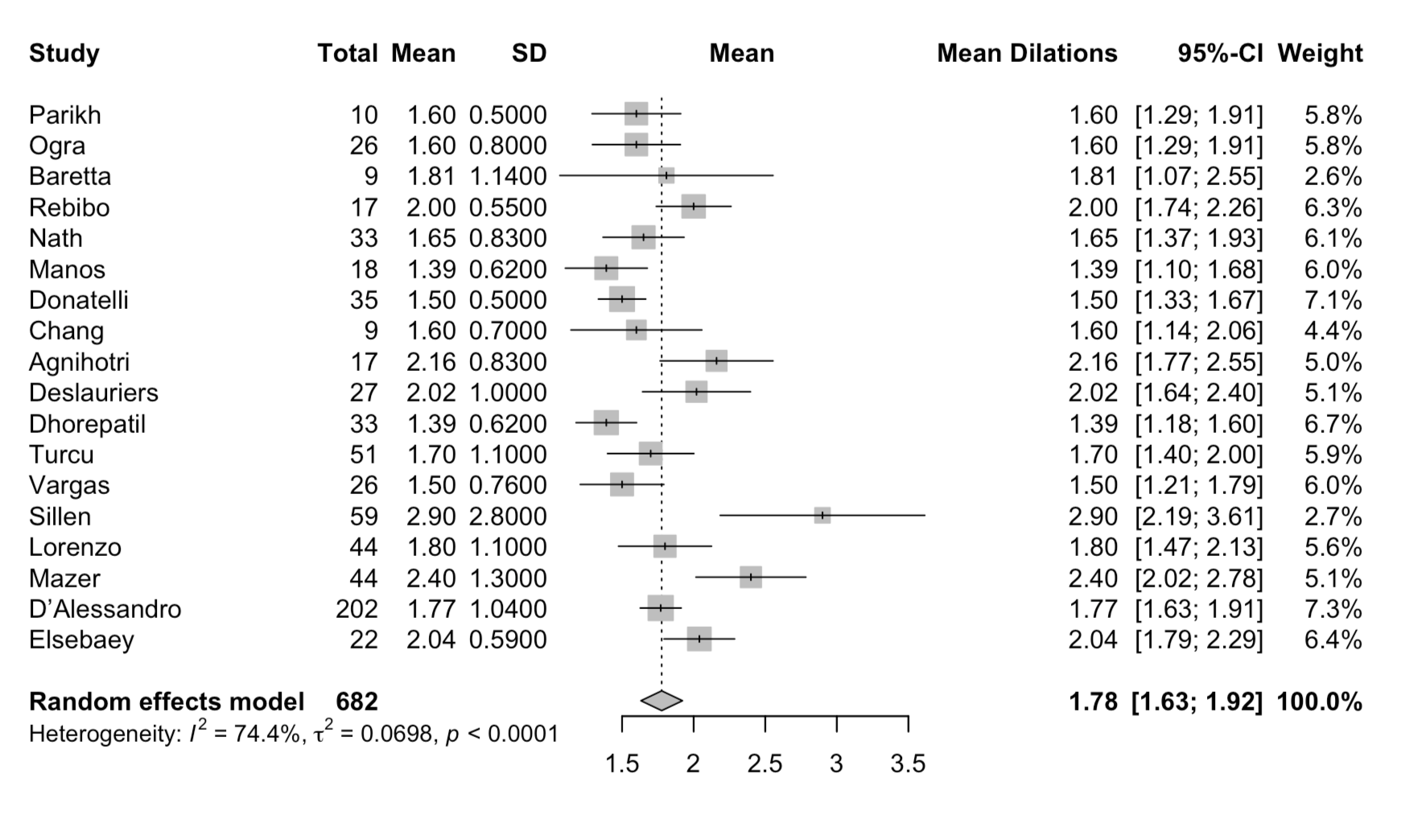
Figure: Figure 1: Forest Plot of Mean Number of Balloon Dilations for Gastric Sleeve Stenosis
Disclosures:
Harsimran Kalsi indicated no relevant financial relationships.
Nihal Khan indicated no relevant financial relationships.
Sanjeevani Tomar indicated no relevant financial relationships.
Hassam Ali indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Kobina Essilfie-Quaye indicated no relevant financial relationships.
Yeshika Thapa indicated no relevant financial relationships.
Yaseen Perbtani indicated no relevant financial relationships.
Tony Brar indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Rabindra Watson indicated no relevant financial relationships.
Rashmi Advani indicated no relevant financial relationships.
Harsimran Kalsi, MD1, Nihal I. Khan, MD2, Sanjeevani Tomar, MD3, Hassam Ali, MD4, Rahul Karna, MD5, Kobina Essilfie-Quaye, MD6, Yeshika Thapa, MD1, Yaseen Perbtani, DO6, Tony Brar, MD1, Babu Mohan, MD7, Rabindra Watson, MD8, Rashmi Advani, MD9. P1402 - How Many Dilations Are Too Many? A Meta-Analysis of Endoscopic Balloon Dilation Outcomes and Surgical Conversion in Gastric Sleeve Stenosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
