Sunday Poster Session
Category: Interventional Endoscopy
P1378 - Re-Evaluating the Optimal Timing of Lumen-Apposing Metal Stent Removal in Necrotizing Pancreatitis: Evidence From a Retrospective Cohort Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Himsikhar Khataniar, MD (he/him/his)
Allegheny General Hospital
Pittsburgh, PA
Presenting Author(s)
Himsikhar Khataniar, MD1, Prateek Harne, MD2, Katherine Albus, MS3, Hany Habib, MD4, Gursimran Kochhar, MD5, Abhijit Kulkarni, MD1, Adam Kichler, DO5, Manish K. Dhawan, MD5
1Allegheny General Hospital, Pittsburgh, PA; 2Allegheny Center for Digestive Health, Pittsburgh, PA; 3Drexel University College of Medicine, Pittsburgh, PA; 4Allegheny Health Network Medicine Institute, Pittsburgh, PA; 5Allegheny Health Network, Pittsburgh, PA
Introduction: Lumen-apposing metal stents (LAMS) have transformed endoscopic management of walled-off necrosis (WON) and large pseudocysts by permitting wide, stable cyst-gastrostomy and direct necrosectomy. Current societies advise retrieval at 3–5 weeks, yet these statements are based on limited data and conflicting single-center series.
Methods: All adults who underwent trans-gastric Hot AXIOS™ placement for WON or symptomatic pseudocyst between January 2017 and March 2025 were retrospectively reviewed. The composite 30-day adverse-event (AE) endpoint captured any post-removal bleeding, migration/burial, new or recurrent fluid collection >4 cm, unplanned readmission or death. Clinical success required radiographic resolution without further intervention. Categorical outcomes were compared with Fisher’s exact test; absolute risk differences (RD) carry 95% CIs.
Results: Forty-nine patients met inclusion (median age 57yr, IQR 48–66; 65% male). Twenty-seven had WON and 22 pseudocysts. Twelve stents were removed early, 17 in the standard window and 20 after >28d, yielding median dwell times of 11, 21 and 47d. Composite 30-day AEs occurred in 2/12 (16.7%) early, 9/17 (52.9%) standard and 4/20 (20%) delayed removals; RD standard–early = +36.3% (95% 4.5–68.0) and RD standard–delayed = +32.9% (3.4–62.4), whereas early and delayed differed less (–3.3%, –30.8–24.1). Bleeding was uncommon (8%) and evenly distributed, but unplanned readmissions were highest with standard timing (35.3% vs 8.3% early, 15.0% delayed). Clinical success was achieved in 10/11 early (90.9%), 12/15 standard (80.0%) and 17/17 delayed cases (100%). Multivariable analysis in 44 patients retained a non-significant but directionally consistent effect for standard removal (OR 4.95 vs early, 95% 0.67–36.3); no demographic or procedural covariate independently predicted AE. Subgroup analysis reinforced the pattern: in WON, AEs were 14.3% early, 54.5% standard and 33.3% delayed, while pseudocyst rates remained ≤25% irrespective of timing.
Discussion: In patients with large pseudocysts and WONs, removal of LAMS early (< 14 days) in showed lowest AE rates when compared to “standard” (14-28 days) and delayed ( >28 days) without compromising clinical success. Additionally, delayed removals also had lower AE rates when compared to standard window of removal. These findings challenge the current LAMS removal timing and suggest that selected patients may safely undergo earlier stent removal with lower AEs. Prospective validation is warranted.
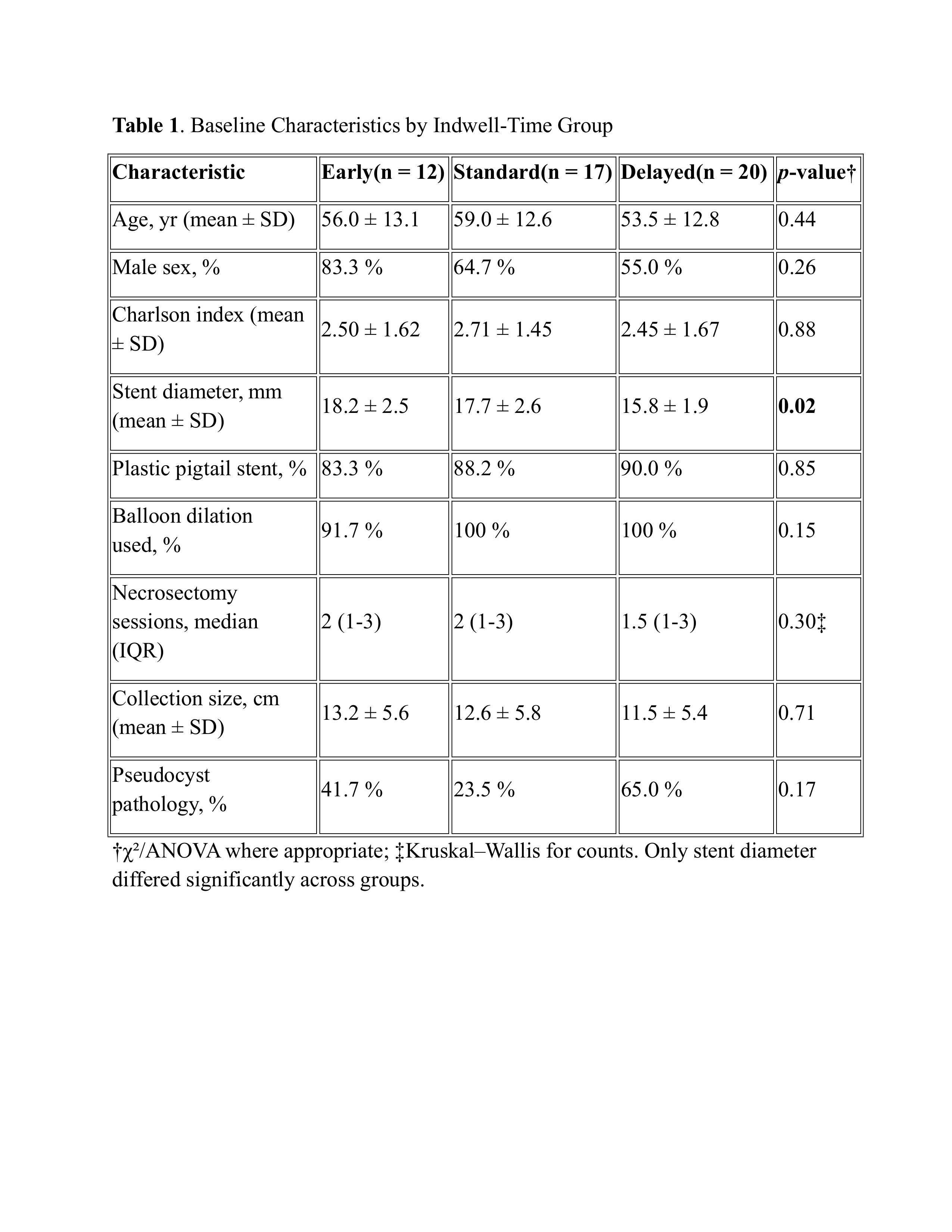
Figure: Table 1. Baseline Characteristics by Indwell-Time Group

Figure: Figure 1: 30-Day Adverse Events and Clinical Success by Timing of LAMS Removal
Disclosures:
Himsikhar Khataniar indicated no relevant financial relationships.
Prateek Harne indicated no relevant financial relationships.
Katherine Albus indicated no relevant financial relationships.
Hany Habib indicated no relevant financial relationships.
Gursimran Kochhar indicated no relevant financial relationships.
Abhijit Kulkarni indicated no relevant financial relationships.
Adam Kichler indicated no relevant financial relationships.
Manish Dhawan indicated no relevant financial relationships.
Himsikhar Khataniar, MD1, Prateek Harne, MD2, Katherine Albus, MS3, Hany Habib, MD4, Gursimran Kochhar, MD5, Abhijit Kulkarni, MD1, Adam Kichler, DO5, Manish K. Dhawan, MD5. P1378 - Re-Evaluating the Optimal Timing of Lumen-Apposing Metal Stent Removal in Necrotizing Pancreatitis: Evidence From a Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Allegheny General Hospital, Pittsburgh, PA; 2Allegheny Center for Digestive Health, Pittsburgh, PA; 3Drexel University College of Medicine, Pittsburgh, PA; 4Allegheny Health Network Medicine Institute, Pittsburgh, PA; 5Allegheny Health Network, Pittsburgh, PA
Introduction: Lumen-apposing metal stents (LAMS) have transformed endoscopic management of walled-off necrosis (WON) and large pseudocysts by permitting wide, stable cyst-gastrostomy and direct necrosectomy. Current societies advise retrieval at 3–5 weeks, yet these statements are based on limited data and conflicting single-center series.
Methods: All adults who underwent trans-gastric Hot AXIOS™ placement for WON or symptomatic pseudocyst between January 2017 and March 2025 were retrospectively reviewed. The composite 30-day adverse-event (AE) endpoint captured any post-removal bleeding, migration/burial, new or recurrent fluid collection >4 cm, unplanned readmission or death. Clinical success required radiographic resolution without further intervention. Categorical outcomes were compared with Fisher’s exact test; absolute risk differences (RD) carry 95% CIs.
Results: Forty-nine patients met inclusion (median age 57yr, IQR 48–66; 65% male). Twenty-seven had WON and 22 pseudocysts. Twelve stents were removed early, 17 in the standard window and 20 after >28d, yielding median dwell times of 11, 21 and 47d. Composite 30-day AEs occurred in 2/12 (16.7%) early, 9/17 (52.9%) standard and 4/20 (20%) delayed removals; RD standard–early = +36.3% (95% 4.5–68.0) and RD standard–delayed = +32.9% (3.4–62.4), whereas early and delayed differed less (–3.3%, –30.8–24.1). Bleeding was uncommon (8%) and evenly distributed, but unplanned readmissions were highest with standard timing (35.3% vs 8.3% early, 15.0% delayed). Clinical success was achieved in 10/11 early (90.9%), 12/15 standard (80.0%) and 17/17 delayed cases (100%). Multivariable analysis in 44 patients retained a non-significant but directionally consistent effect for standard removal (OR 4.95 vs early, 95% 0.67–36.3); no demographic or procedural covariate independently predicted AE. Subgroup analysis reinforced the pattern: in WON, AEs were 14.3% early, 54.5% standard and 33.3% delayed, while pseudocyst rates remained ≤25% irrespective of timing.
Discussion: In patients with large pseudocysts and WONs, removal of LAMS early (< 14 days) in showed lowest AE rates when compared to “standard” (14-28 days) and delayed ( >28 days) without compromising clinical success. Additionally, delayed removals also had lower AE rates when compared to standard window of removal. These findings challenge the current LAMS removal timing and suggest that selected patients may safely undergo earlier stent removal with lower AEs. Prospective validation is warranted.
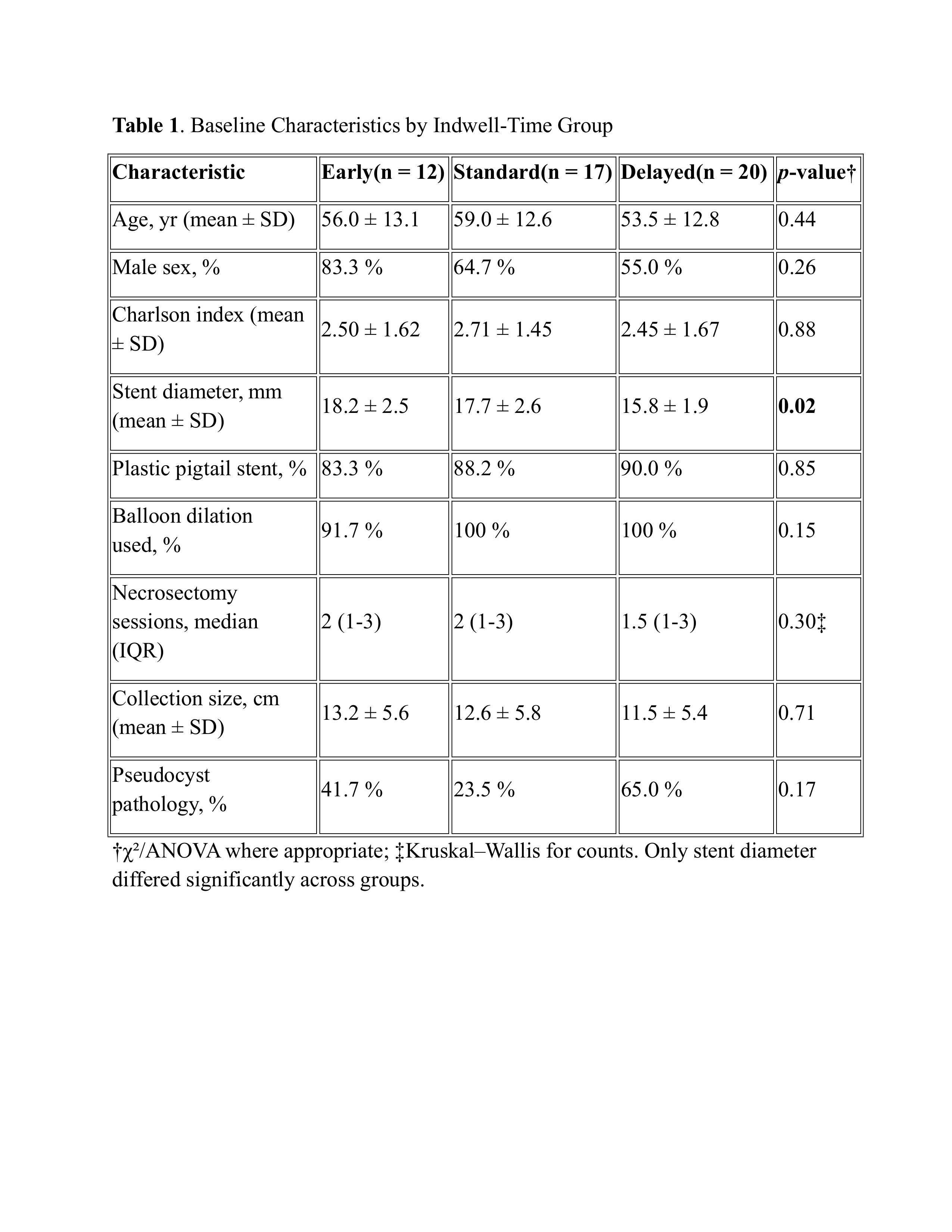
Figure: Table 1. Baseline Characteristics by Indwell-Time Group

Figure: Figure 1: 30-Day Adverse Events and Clinical Success by Timing of LAMS Removal
Disclosures:
Himsikhar Khataniar indicated no relevant financial relationships.
Prateek Harne indicated no relevant financial relationships.
Katherine Albus indicated no relevant financial relationships.
Hany Habib indicated no relevant financial relationships.
Gursimran Kochhar indicated no relevant financial relationships.
Abhijit Kulkarni indicated no relevant financial relationships.
Adam Kichler indicated no relevant financial relationships.
Manish Dhawan indicated no relevant financial relationships.
Himsikhar Khataniar, MD1, Prateek Harne, MD2, Katherine Albus, MS3, Hany Habib, MD4, Gursimran Kochhar, MD5, Abhijit Kulkarni, MD1, Adam Kichler, DO5, Manish K. Dhawan, MD5. P1378 - Re-Evaluating the Optimal Timing of Lumen-Apposing Metal Stent Removal in Necrotizing Pancreatitis: Evidence From a Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
