Sunday Poster Session
Category: Interventional Endoscopy
P1373 - Does Timing of Endoscopy Impact Outcomes in Foreign Body Ingestion? A Nationwide Trend Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Dinuka Bandara, DO
Creighton University School of Medicine
Scottsdale, AZ
Presenting Author(s)
Silpa Choday, MD1, Dinuka Bandara, DO2, William Graham, MD1, Akanksha Togra, MD3, Dushyant S. Dahiya, MD4, Hassam Ali, MD5, Manesh Gangwani, MD6, Keng-Yu Chuang, MD7, Neil Vyas, MD1
1Creighton University School of Medicine, Phoenix, AZ; 2Creighton University School of Medicine, Scottsdale, AZ; 3Texas Tech University Health Sciences Center, El Paso, El Paso, TX; 4University of Kansas School of Medicine, Kansas City, KS; 5East Carolina University/Brody School of Medicine, Greenville, NC; 6University of Arkansas for Medical Sciences, Little Rock, AR; 7GI Alliance, Phoenix, AZ
Introduction: Foreign body ingestion (FBI) is a common clinical condition encountered across various age groups, with significant implications for healthcare systems worldwide. Recurrent episodes of FBI present unique challenges, as they are often associated with underlying psychiatric disorders, developmental delays, or behavioral issues. This study aims to evaluate the trends and predictors of hospital readmissions following FBI.
Methods: A retrospective analysis was conducted using data from the Nationwide Readmissions Database (NRD) for index admissions and 30-day readmissions. The variables analyzed included patient demographics, insurance status, hospital characteristics, psychiatric disorders, and clinical outcomes such as mortality, length of stay (LOS), and total hospitalization costs. Inflation-adjusted costs were reported in 2021 U.S. dollars.
Results: Over six years, there were 141,889 index admissions, with 18,956 30-day readmissions. The mean age of patients ranged from 52.4 to 54.4 years, with males consistently comprising 55% of admissions. Medicare usage ranged from 45.2% to 48%, while Medicaid coverage increased from 22% to 24.4%. Psychiatric disorders associated with FB ingestion showed slight increases, particularly bipolar (0.8% to 1.1%) and mood disorders (0.6% to 1%). Mortality rates rose from 1.5% to 2.1%, and average length of stay (LOS) increased from 6.1 to 7 days, with total hospital charges rising from $66,614 to $79,026. Of 81,790 patients undergoing endoscopy, 62,834 had early EGD, and 18,956 had late EGD. Early EGD patients were younger (mean age 29 vs. 42) and more likely to have Medicaid, private insurance, and self-pay. Late EGD patients had higher Medicare usage (57.3%) and experienced more severe complications, including GI bleeding (21.1% vs. 14.3%), sepsis (6.2% vs. 3.3%), septic shock (2.3% vs. 1%), and higher mortality (2.1% vs. 1.3%). Late EGD patients also had longer LOS (8 vs. 3.8 days). These results indicate that late EGD is associated with older patients, more severe clinical conditions, and worse outcomes.
Discussion: The study highlights consistent trends in hospital utilization and outcomes, including rising mortality, length of stay, and hospitalization costs. The increasing prevalence of Medicaid coverage and the growing role of metropolitan teaching hospitals underscore shifts in healthcare delivery and patient demographics. These findings emphasize the need for targeted interventions to reduce readmissions and improve healthcare efficiency.
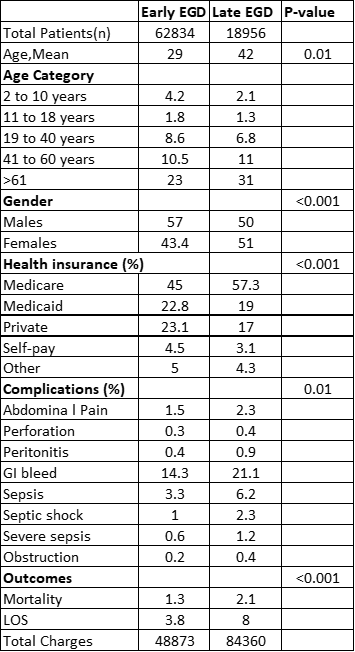
Figure: Early Versus Late EGD
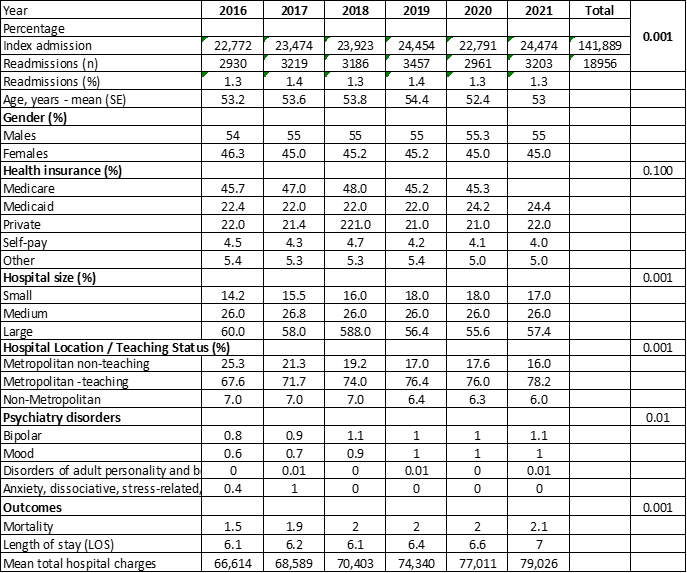
Figure: Demographic and Psychiatric Trends in Foreign Body Ingestion
Disclosures:
Silpa Choday indicated no relevant financial relationships.
Dinuka Bandara indicated no relevant financial relationships.
William Graham indicated no relevant financial relationships.
Akanksha Togra indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Hassam Ali indicated no relevant financial relationships.
Manesh Gangwani indicated no relevant financial relationships.
Keng-Yu Chuang indicated no relevant financial relationships.
Neil Vyas indicated no relevant financial relationships.
Silpa Choday, MD1, Dinuka Bandara, DO2, William Graham, MD1, Akanksha Togra, MD3, Dushyant S. Dahiya, MD4, Hassam Ali, MD5, Manesh Gangwani, MD6, Keng-Yu Chuang, MD7, Neil Vyas, MD1. P1373 - Does Timing of Endoscopy Impact Outcomes in Foreign Body Ingestion? A Nationwide Trend Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Creighton University School of Medicine, Phoenix, AZ; 2Creighton University School of Medicine, Scottsdale, AZ; 3Texas Tech University Health Sciences Center, El Paso, El Paso, TX; 4University of Kansas School of Medicine, Kansas City, KS; 5East Carolina University/Brody School of Medicine, Greenville, NC; 6University of Arkansas for Medical Sciences, Little Rock, AR; 7GI Alliance, Phoenix, AZ
Introduction: Foreign body ingestion (FBI) is a common clinical condition encountered across various age groups, with significant implications for healthcare systems worldwide. Recurrent episodes of FBI present unique challenges, as they are often associated with underlying psychiatric disorders, developmental delays, or behavioral issues. This study aims to evaluate the trends and predictors of hospital readmissions following FBI.
Methods: A retrospective analysis was conducted using data from the Nationwide Readmissions Database (NRD) for index admissions and 30-day readmissions. The variables analyzed included patient demographics, insurance status, hospital characteristics, psychiatric disorders, and clinical outcomes such as mortality, length of stay (LOS), and total hospitalization costs. Inflation-adjusted costs were reported in 2021 U.S. dollars.
Results: Over six years, there were 141,889 index admissions, with 18,956 30-day readmissions. The mean age of patients ranged from 52.4 to 54.4 years, with males consistently comprising 55% of admissions. Medicare usage ranged from 45.2% to 48%, while Medicaid coverage increased from 22% to 24.4%. Psychiatric disorders associated with FB ingestion showed slight increases, particularly bipolar (0.8% to 1.1%) and mood disorders (0.6% to 1%). Mortality rates rose from 1.5% to 2.1%, and average length of stay (LOS) increased from 6.1 to 7 days, with total hospital charges rising from $66,614 to $79,026. Of 81,790 patients undergoing endoscopy, 62,834 had early EGD, and 18,956 had late EGD. Early EGD patients were younger (mean age 29 vs. 42) and more likely to have Medicaid, private insurance, and self-pay. Late EGD patients had higher Medicare usage (57.3%) and experienced more severe complications, including GI bleeding (21.1% vs. 14.3%), sepsis (6.2% vs. 3.3%), septic shock (2.3% vs. 1%), and higher mortality (2.1% vs. 1.3%). Late EGD patients also had longer LOS (8 vs. 3.8 days). These results indicate that late EGD is associated with older patients, more severe clinical conditions, and worse outcomes.
Discussion: The study highlights consistent trends in hospital utilization and outcomes, including rising mortality, length of stay, and hospitalization costs. The increasing prevalence of Medicaid coverage and the growing role of metropolitan teaching hospitals underscore shifts in healthcare delivery and patient demographics. These findings emphasize the need for targeted interventions to reduce readmissions and improve healthcare efficiency.
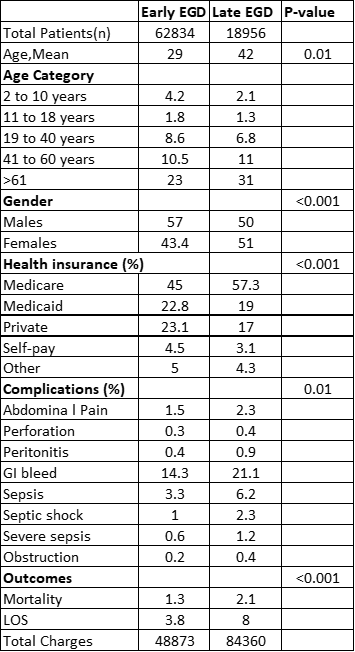
Figure: Early Versus Late EGD
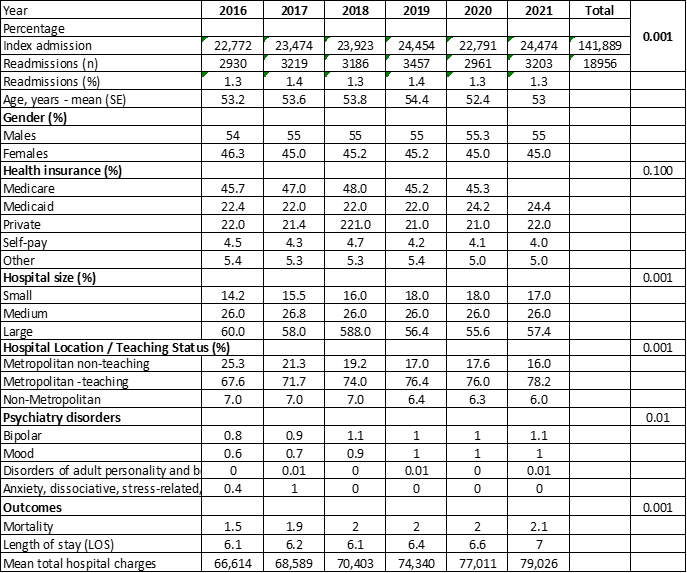
Figure: Demographic and Psychiatric Trends in Foreign Body Ingestion
Disclosures:
Silpa Choday indicated no relevant financial relationships.
Dinuka Bandara indicated no relevant financial relationships.
William Graham indicated no relevant financial relationships.
Akanksha Togra indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Hassam Ali indicated no relevant financial relationships.
Manesh Gangwani indicated no relevant financial relationships.
Keng-Yu Chuang indicated no relevant financial relationships.
Neil Vyas indicated no relevant financial relationships.
Silpa Choday, MD1, Dinuka Bandara, DO2, William Graham, MD1, Akanksha Togra, MD3, Dushyant S. Dahiya, MD4, Hassam Ali, MD5, Manesh Gangwani, MD6, Keng-Yu Chuang, MD7, Neil Vyas, MD1. P1373 - Does Timing of Endoscopy Impact Outcomes in Foreign Body Ingestion? A Nationwide Trend Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
