Sunday Poster Session
Category: Infections and Microbiome
P1364 - Actinomyces Within Polypoid Tissue
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- HS
Hannah Shinn, DO (she/her/hers)
Naval Medical Center Portsmouth
Suffolk, VA
Presenting Author(s)
Hannah Shinn, DO1, Max Santibanez, DO2, Sarah Zimmer, MD, BS3, Allison Bush, MD4, Varea Costello, DO, MPH5, Lindsay J. Jayne, DDS, MS5
1Naval Medical Center Portsmouth, Suffolk, VA; 2Naval Medical Center Portsmouth, Norfolk, VA; 3Naval Medical Center Portsmouth, Chesapeake, VA; 4Uniformed Services University of the Health Sciences, Portsmouth, VA; 5Naval Medical Center Portsmouth, Portsmouth, VA
Introduction: Actinomycosis is an infection caused by Actinomyces, a bacterium found in normal oral flora. Gastrointestinal (GI) involvement is rare, and when it occurs, is termed abdominal actinomycosis (AA). AA often arises in the setting of immunosuppression or disruption of the GI mucosa. Clinical presentations are often nonspecific, including altered bowel habits, abdominal pain or signs of peritonitis. We present a case of an immunocompetent patient with intermittent scant hematochezia and no other symptoms and colonoscopy revealed Actinomyces within polyp tissue.
Case Description/
Methods: A 52-year-old male presented to the GI clinic with five years of painless, intermittent hematochezia. He had one prior colonoscopy two years earlier that was limited by inadequate bowel preparation but was otherwise normal. He had no significant past medical or surgical history aside from remote treatment for latent TB and was on no medications. Laboratory evaluation revealed a recent negative test for human immunodeficiency virus, and a normal complete blood count and metabolic panel. Physical exam was without abnormalities. A diagnostic colonoscopy demonstrated internal hemorrhoids, three diminutive sessile polyps in the descending colon found to be tubular adenomas, and one 3mm sessile polyp (Figure 1) in the sigmoid colon with granulation tissue with actinomyces (Figure 2). The patient was evaluated by an Infectious Diseases specialist with plan to clinically monitor for signs of infection given the absence of risk factors or symptoms. The patient remained asymptomatic with plan for a repeat colonoscopy in three years his tubular adenomas.
Discussion: Actinomyces in an asymptomatic colon polyp is a rare finding. Actinomycosis involves the abdomen in approximately 20% of cases. Of the AA cases, only 15% involve the colon. When AA presents in the colon, it may manifest as abscesses or polyps or mimic other pathology such as malignancy or IBD. Most AA cases occur in the setting of immunosuppression or disruption to the mucosa and result in non-specific symptoms ranging from mild abdominal pain to signs of peritonitis. The standard of care is 2-6 weeks of intravenous penicillin followed by high-dose oral penicillin for a total of 6 months or until resolution. While actinomyces is present in gut flora, is it an uncommon finding in a colon polyp. Our case adds to the literature of colonic AA and highlights a rare finding of actinomyces in a diminutive colon polyp in an asymptomatic immunocompetent patient.
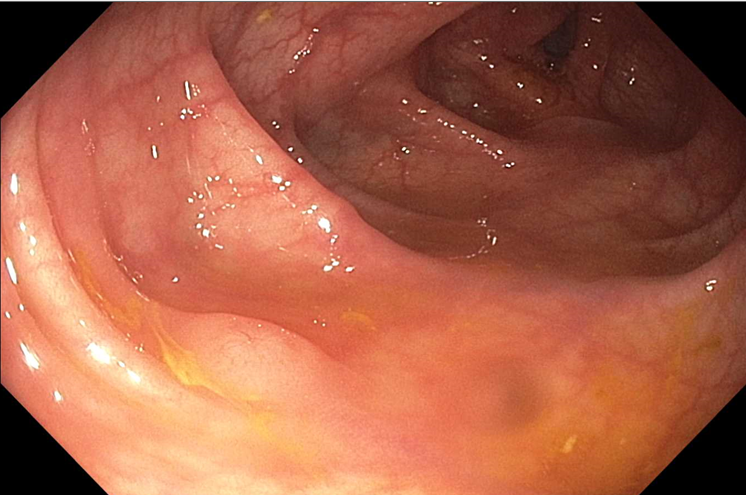
Figure: Sessile polyp Figure 1

Figure: 2x view Actinomyces with inflammation and colonic mucosa Figure 2
Disclosures:
Hannah Shinn indicated no relevant financial relationships.
Max Santibanez indicated no relevant financial relationships.
Sarah Zimmer indicated no relevant financial relationships.
Allison Bush indicated no relevant financial relationships.
Varea Costello indicated no relevant financial relationships.
Lindsay Jayne indicated no relevant financial relationships.
Hannah Shinn, DO1, Max Santibanez, DO2, Sarah Zimmer, MD, BS3, Allison Bush, MD4, Varea Costello, DO, MPH5, Lindsay J. Jayne, DDS, MS5. P1364 - Actinomyces Within Polypoid Tissue, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Naval Medical Center Portsmouth, Suffolk, VA; 2Naval Medical Center Portsmouth, Norfolk, VA; 3Naval Medical Center Portsmouth, Chesapeake, VA; 4Uniformed Services University of the Health Sciences, Portsmouth, VA; 5Naval Medical Center Portsmouth, Portsmouth, VA
Introduction: Actinomycosis is an infection caused by Actinomyces, a bacterium found in normal oral flora. Gastrointestinal (GI) involvement is rare, and when it occurs, is termed abdominal actinomycosis (AA). AA often arises in the setting of immunosuppression or disruption of the GI mucosa. Clinical presentations are often nonspecific, including altered bowel habits, abdominal pain or signs of peritonitis. We present a case of an immunocompetent patient with intermittent scant hematochezia and no other symptoms and colonoscopy revealed Actinomyces within polyp tissue.
Case Description/
Methods: A 52-year-old male presented to the GI clinic with five years of painless, intermittent hematochezia. He had one prior colonoscopy two years earlier that was limited by inadequate bowel preparation but was otherwise normal. He had no significant past medical or surgical history aside from remote treatment for latent TB and was on no medications. Laboratory evaluation revealed a recent negative test for human immunodeficiency virus, and a normal complete blood count and metabolic panel. Physical exam was without abnormalities. A diagnostic colonoscopy demonstrated internal hemorrhoids, three diminutive sessile polyps in the descending colon found to be tubular adenomas, and one 3mm sessile polyp (Figure 1) in the sigmoid colon with granulation tissue with actinomyces (Figure 2). The patient was evaluated by an Infectious Diseases specialist with plan to clinically monitor for signs of infection given the absence of risk factors or symptoms. The patient remained asymptomatic with plan for a repeat colonoscopy in three years his tubular adenomas.
Discussion: Actinomyces in an asymptomatic colon polyp is a rare finding. Actinomycosis involves the abdomen in approximately 20% of cases. Of the AA cases, only 15% involve the colon. When AA presents in the colon, it may manifest as abscesses or polyps or mimic other pathology such as malignancy or IBD. Most AA cases occur in the setting of immunosuppression or disruption to the mucosa and result in non-specific symptoms ranging from mild abdominal pain to signs of peritonitis. The standard of care is 2-6 weeks of intravenous penicillin followed by high-dose oral penicillin for a total of 6 months or until resolution. While actinomyces is present in gut flora, is it an uncommon finding in a colon polyp. Our case adds to the literature of colonic AA and highlights a rare finding of actinomyces in a diminutive colon polyp in an asymptomatic immunocompetent patient.
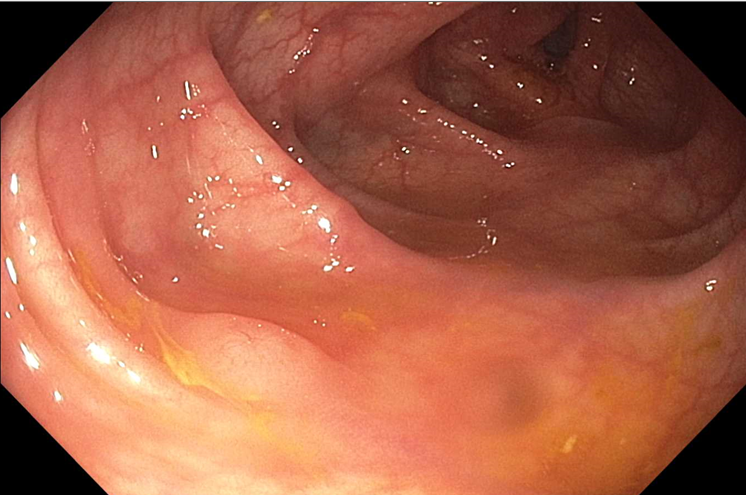
Figure: Sessile polyp Figure 1

Figure: 2x view Actinomyces with inflammation and colonic mucosa Figure 2
Disclosures:
Hannah Shinn indicated no relevant financial relationships.
Max Santibanez indicated no relevant financial relationships.
Sarah Zimmer indicated no relevant financial relationships.
Allison Bush indicated no relevant financial relationships.
Varea Costello indicated no relevant financial relationships.
Lindsay Jayne indicated no relevant financial relationships.
Hannah Shinn, DO1, Max Santibanez, DO2, Sarah Zimmer, MD, BS3, Allison Bush, MD4, Varea Costello, DO, MPH5, Lindsay J. Jayne, DDS, MS5. P1364 - Actinomyces Within Polypoid Tissue, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
