Sunday Poster Session
Category: Infections and Microbiome
P1363 - Disseminated Histoplasmosis Resulting in Small Bowel Gastrointestinal Bleeding
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- KB
Kelly Beharry, BS (she/her/hers)
University of Michigan Medical School
Ann Arbor, MI
Presenting Author(s)
Kelly Beharry, BS1, LaVana V. Greene-Higgs, MD2, Akbar K. Waljee, MD, MS2, Sarah Uttal, MD2, Nikhilesh Mazumder, MD, MPH2
1University of Michigan Medical School, Ann Arbor, MI; 2Michigan Medicine, Ann Arbor, MI
Introduction: Histoplasmosis is an infection caused by the dimorphic fungus Histoplasma capsulatum that is endemic to the Ohio and Mississippi river valleys. While immunocompetent individuals typically clear the infection, immunosuppressed patients may develop a disseminated form of the infection. Disseminated histoplasmosis represents a broad spectrum of clinical presentations including fever, anorexia, hepatosplenomegaly, lymphadenopathy and oropharyngeal ulcerations, and can be fatal if left untreated. Currently, there are limited reports on the effects of this infection on the gastrointestinal tract. This report presents a case of disseminated histoplasmosis involving the small bowel.
Case Description/
Methods: A 71-year-old man from Ohio with a history of sarcoidosis involving the lungs, brain, and liver on adalimumab and prednisone presented with three months of sore throat, anorexia, fatigue, and weakness. Given significant immunosuppression, there was concern for an infectious process with testing consistent with a diagnosis of disseminated histoplasmosis including positive urine, serum, and cerebral spinal fluid samples. While hospitalized and receiving Amphotericin for management, the patient developed hematochezia with hemodynamic instability. CT angiography was consistent with an arterial bleed in the proximal ileum. Patient underwent arterial embolization with resolution of hematochezia, but subsequently developed melena. At that time, bidirectional endoscopy was performed which revealed moderate inflammation in the terminal ileum and several jejunal ulcerations, the largest measuring 20mm (Figure 1). Biopsies of the ulcerations were obtained and evaluated with PAS-D and GMS stains, which demonstrated fungal microorganisms consistent with H. capsulatum (Figure 2). Patient was continued on Amphotericin therapy throughout hospitalization without further episodes of gastrointestinal bleeding.
Discussion: This case illustrates the complex and varied clinical manifestations of disseminated histoplasmosis. While it is known that this organism can affect the oropharyngeal tract, it has not often been associated with conditions involving the small bowel and gastrointestinal bleeding. This case highlights the need for heightened awareness among clinicians regarding the potential manifestations of fungal infections, particularly in immunocompromised patients from endemic regions.
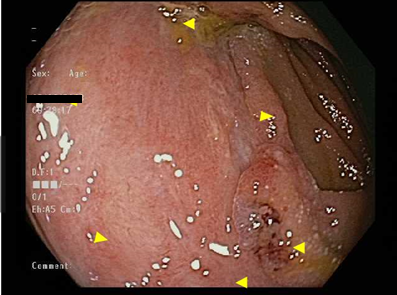
Figure: Figure 1. Jejunal Ulcer

Figure: Figure 2. Histoplasma capsulatum on GMS stain
Disclosures:
Kelly Beharry indicated no relevant financial relationships.
LaVana Greene-Higgs indicated no relevant financial relationships.
Akbar Waljee indicated no relevant financial relationships.
Sarah Uttal indicated no relevant financial relationships.
Nikhilesh Mazumder indicated no relevant financial relationships.
Kelly Beharry, BS1, LaVana V. Greene-Higgs, MD2, Akbar K. Waljee, MD, MS2, Sarah Uttal, MD2, Nikhilesh Mazumder, MD, MPH2. P1363 - Disseminated Histoplasmosis Resulting in Small Bowel Gastrointestinal Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Michigan Medical School, Ann Arbor, MI; 2Michigan Medicine, Ann Arbor, MI
Introduction: Histoplasmosis is an infection caused by the dimorphic fungus Histoplasma capsulatum that is endemic to the Ohio and Mississippi river valleys. While immunocompetent individuals typically clear the infection, immunosuppressed patients may develop a disseminated form of the infection. Disseminated histoplasmosis represents a broad spectrum of clinical presentations including fever, anorexia, hepatosplenomegaly, lymphadenopathy and oropharyngeal ulcerations, and can be fatal if left untreated. Currently, there are limited reports on the effects of this infection on the gastrointestinal tract. This report presents a case of disseminated histoplasmosis involving the small bowel.
Case Description/
Methods: A 71-year-old man from Ohio with a history of sarcoidosis involving the lungs, brain, and liver on adalimumab and prednisone presented with three months of sore throat, anorexia, fatigue, and weakness. Given significant immunosuppression, there was concern for an infectious process with testing consistent with a diagnosis of disseminated histoplasmosis including positive urine, serum, and cerebral spinal fluid samples. While hospitalized and receiving Amphotericin for management, the patient developed hematochezia with hemodynamic instability. CT angiography was consistent with an arterial bleed in the proximal ileum. Patient underwent arterial embolization with resolution of hematochezia, but subsequently developed melena. At that time, bidirectional endoscopy was performed which revealed moderate inflammation in the terminal ileum and several jejunal ulcerations, the largest measuring 20mm (Figure 1). Biopsies of the ulcerations were obtained and evaluated with PAS-D and GMS stains, which demonstrated fungal microorganisms consistent with H. capsulatum (Figure 2). Patient was continued on Amphotericin therapy throughout hospitalization without further episodes of gastrointestinal bleeding.
Discussion: This case illustrates the complex and varied clinical manifestations of disseminated histoplasmosis. While it is known that this organism can affect the oropharyngeal tract, it has not often been associated with conditions involving the small bowel and gastrointestinal bleeding. This case highlights the need for heightened awareness among clinicians regarding the potential manifestations of fungal infections, particularly in immunocompromised patients from endemic regions.
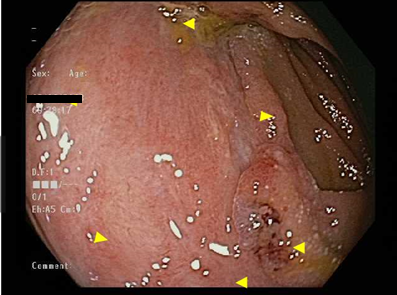
Figure: Figure 1. Jejunal Ulcer

Figure: Figure 2. Histoplasma capsulatum on GMS stain
Disclosures:
Kelly Beharry indicated no relevant financial relationships.
LaVana Greene-Higgs indicated no relevant financial relationships.
Akbar Waljee indicated no relevant financial relationships.
Sarah Uttal indicated no relevant financial relationships.
Nikhilesh Mazumder indicated no relevant financial relationships.
Kelly Beharry, BS1, LaVana V. Greene-Higgs, MD2, Akbar K. Waljee, MD, MS2, Sarah Uttal, MD2, Nikhilesh Mazumder, MD, MPH2. P1363 - Disseminated Histoplasmosis Resulting in Small Bowel Gastrointestinal Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

